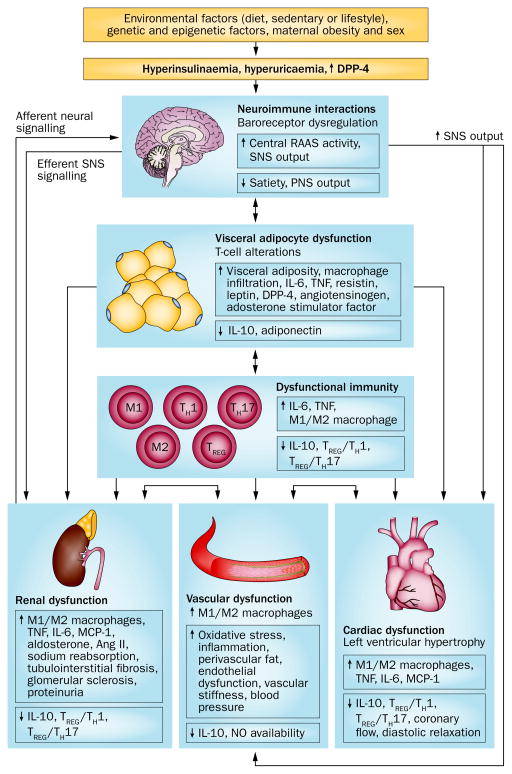
Figure 1.
Obesity contributes to the development of hypertension via the interaction of dietary, genetic, epigenetic and environmental factors. Visceral adipocyte dysfunction leads directly to renal, cardiac and vascular dysfunction, via an impaired immune or inflammatory response, and by affecting neuroimmune interactions that alter SNS signalling. Cardiac and/or renal abnormalities can lead to vascular dysfunction and vice-versa. Obesity-related hypertension is associated with structural and functional changes in the kidney, heart and vasculature. Hyperuricaemia might also affect adipocyte function and vascular remodelling, and cause renal abnormalities. Abbreviations: ↑, increased; ↓, decreased; Ang II, angiotensin II; DPP-4, dipeptidyl peptidase 4; MCP-1, monocyte chemoattractant protein-1; PNS, parasympathetic nervous system; RAAS, renin–angiotensin–aldosterone system; SNS, sympathetic nervous system; TH, T helper cell; TREG, T regulatory cell.