Abstract
In this study, the in vitro effects of paclitaxel (PTX) and Cremophor-EL (CrEL) on blood viscosity and oxidative stress markers were investigated. Whole-blood samples were collected from healthy volunteers and co-incubated with PTX, CrEL or their combination then compared with control blood samples. After a 24 h incubation time, the whole-blood viscosity (WBV), erythrocyte sedimentation rate (ESR), levels of whole-blood malondialdehyde (MDA), protein carbonyl content (PCC) and reduced glutathione (GSH) were determined. Moreover, plasma nitrite and plasma sialic acid (SA) values were measured. The present results revealed that the incubation of blood samples with PTX, CrEL or PTX plus CrEL significantly increased the values of WBV, ESR, MDA and PCC compared to control samples. In contrast, a significant decrease in levels of GSH, SA and nitrite was observed after incubation of blood samples with tested agents compared to control. The effects of tested agents on the measured parameters were more pronounced in the case of blood samples treated with PTX plus CrEL. The present study demonstrates that PTX-induced oxidative stress is associated with an increase of WBV.
Keywords: Blood viscosity, Paclitaxel, Cremophor-EL, Glutathione, Oxidative stress
1. Introduction
Blood is a non-Newtonian fluid considered as a suspension or an emulsion, therefore, it has special rheological behavior. Erythrocytes aggregability and deformability are important regulators of blood rheology (Baskurt and Meiselman, 2003). Erythrocyte deformability is the determinant of blood viscosity at high shear rates, while at low shear, the viscosity reflects erythrocytes aggregability (Simmonds et al., 2013). Additionally, blood rheological parameters are affected by blood coagulation, paraproteinemia, lipid profile and complete blood count indices (vonTempelhoff et al., 2003). Blood biorheology was deteriorated by oxidative stress, inflammation, diabetes, obesity, aging, smoking and cancer (Hitsumoto, 2012). The alterations in blood rheological variables reduced blood flow and decreased tissue oxygenation. Therefore, monitoring of blood rheology is useful during chemotherapy (vonTempelhoff et al., 2003). As well, measurement of blood rheological parameters is beneficial in assessing the response to therapy and drug compliance (Awodu et al., 2007), however, up till now, there are not enough data about this issue.
Increasing oxidative products of lipids, malondialdehyde (MDA), proteins, carbonyl content (PCC), as well as decreasing of glutathione (GSH) were associated with increasing blood viscosity (Li et al., 2010; Richards and Nwose, 2010). Sialic acid (SA) is an essential constituent of many glycoproteins and glycolipids which have structural and regulatory roles in immunity, homoeostasis, inflammation and antioxidant activity (Byrne et al., 2007; Iijima et al., 2004; Ogasawara et al., 2007). Moreover, SA is responsible for erythrocytes zeta potential, morphology, deformability, aggregability and acts as a senescent marker (Huang et al., 2011; Lutz and Bogdanova, 2013; Mehdi et al., 2012). Exposure to oxidative stress resulted in desialylation and alteration of SA metabolism (Pawluczyk et al., 2014). The decrease in erythrocytes SA content may influence the rheological properties of blood (Hadengue et al., 1998).
Nitric oxide (NO) is an important signal molecule, in circulation, it is synthesized mainly by vascular endothelial cells and erythrocytes. NO plays an important role in the modulation of the rheological behavior of blood (Yerer et al., 2010; Baskurt et al., 2011). The reduction of NO influences erythrocyte deformability and subsequently impairs rheological properties (Suhr et al., 2009). Furthermore, nitrosative damage to the erythrocyte membrane leads to impairment of blood biorheological properties (Yerer et al., 2010). Despite that measurement of whole blood viscosity (WBV) may assist in earlier detection of asymptomatic oxidative stress (Richards and Nwose, 2010), the mechanisms by which oxidative stress induce WBV changes are not yet completely understood.
Paclitaxel (PTX) is an effective chemotherapeutic agent that is widely used for the treatment of breast carcinomas. The primary targets of PTX are components of the cytoskeleton, PTX acts to promote the stabilization of the microtubules (Hadzic et al., 2010). PTX induces cytotoxic effect by increased production of ROS and reactive nitrogen species (Alexandre et al., 2007). Cremophor EL (CrEL) is a synthetic, nonionic surfactant that has the ability to stabilize emulsions. CrEL is used as vehicle in commercial taxane formulations; it can cause adverse effects on blood rheology (Mark et al., 2001). However, not enough data are available about the effect of CrEL on blood rheology.
The precise mechanisms by which PTX and CrEL induced hemorheological alterations are still unclear. In this study, we hypothesized that PTX may influence blood rheology through an oxidative stress-mediated mechanism. Herein, the association between WBV and oxidative stress markers was investigated in vitro, in terms of MDA, PCC, GSH, SA and nitrite with PTX and/or CrEL treated blood samples.
2. Materials and methods
2.1. Materials
PTX was obtained from David Bull Laboratories (Victoria, Australia). Tert-butyl hydroperoxide (t-BHP), tetraethoxypropane, GSH and thiobarbituric acid (TBA) were obtained from Sigma Chemical Co. (St. Louis, MO, USA). All other chemicals were of analytical grade. The equipment used in this study included the following: a Spectro UV–Vis Split Beam PC spectrophotometer (Model UVS-2800; Labomed, Inc.), a SW22 shaking water bath (Julabo), a CT5 centrifuge and a LH 780 Hematology Analyzer (Beckman Coulter).
2.2. Subjects
Blood was collected in heparinized Vacuette tubes from adult volunteers (46–52 years old). The volunteers had no chronic or acute illnesses and had not taken any drugs, or dietary supplements in the previous four weeks. The protocol for this study conformed to the guidelines of our Institutional Ethics Committee.
2.3. Methods
2.3.1. Experimental design
Blood samples were divided into five groups, each with 6 samples as follows:
-
1-
Group 1: whole blood samples without any treatments, control group.
-
2-
Group 2: whole blood was incubated with 10 μM t-BHP, t-BHP group. In this group, t-BHP was acting as a reference oxidative stress inducer (Pandey and Rizvi, 2010).
-
3-
Group 3: whole blood was incubated with 100 μM PTX (Lang et al., 2006), PTX group.
-
4-
Group 4: whole blood was incubated with 5% CrEL (Mark et al., 2001), CrEL group.
-
5-
Group 5: whole blood was incubated with PTX and CrEL, PTX plus CrEL group.
Stock solutions of tBHP and PTX were prepared by dissolving a specific amount in 1% dimethylsulfoxide. The final concentration of dimethylsulfoxide was 0.1% in working solutions and 0.1% dimethylsulfoxide is used as a vehicle control.
All samples were incubated at 37 °C for 24 h with moderate shaking. After the incubation period, the samples were divided into 3 parts. The first part was used for the determination of WBV, mean cell volume (MCV) and erythrocytes distribution width (RDW), erythrocyte count and ESR. The second aliquot was hemolyzed with distilled water and centrifuged at 6000 rpm for 10 min. The supernatant was collected to determine the levels of GSH, MDA and PCC. The last part was centrifuged at 1500 rpm for the separation of plasma to determine SA and nitrite levels as an index for NO production.
2.3.2. Determination of GSH content
The concentration of GSH was determined in the whole-blood samples according to the method of Beutler et al. (1963). The first part of whole blood was hemolyzed with cold water and the proteins were precipitated by the addition of 30% TCA. Aliquots (50 μL) of the hemolyzed sample and 50 μL of 10 mM DTNB were mixed in a tube containing 0.8 mL of 200 mM phosphate buffer (pH 8.0). After 3 min, the absorbance was measured at 412 nm. Reduced GSH was used as standard.
2.3.3. Determination of plasma SA levels
The plasma SA level was determined according to the method of Spyridaki and Siskos (1996). 100 μL of 0.04 M periodic acid was added to a glass tube containing 500 μL of diluted (20 times) sample solution. The mixture was mixed thoroughly and allowed to stand in an ice bath for 30 min. Thereafter, 1.25 mL of resorcinol solution was mixed and heated at 98 °C for 5 min. Tubes were cooled in an ice bath for approximately 2 min, and 3.25 mL of n-butanol was added. Solutions were mixed vigorously and the tubes were placed in a water bath at 37 °C for 3 min for the color to stabilize. Immediately after removing the solutions from the water bath their absorbance was measured at 625 nm against a reagent blank. The unknown concentrations of SA in samples were calculated from a calibration graph and expressed as mM.
2.3.4. Determination of plasma nitrite levels
The plasma nitrite levels were measured as an index of NO production. For total nitrite detection, 300 μL of plasma was deproteinized by adding 600 μL of 75 mM zinc sulfate solution. The mixture was stirred and centrifuged at 1000 rpm for 5 min at ambient temperature and then 600 μL of 55 mM NaOH was added. Total nitrite was quantitated by Griess reaction after incubation of plasma samples with copperized cadmium granules for 90 min to convert nitrate to nitrite in glisin-NaOH buffer of pH 9.7. Griess reagent (1 mL 0.5% sulfanilamide and 0.05% N-naphthylethylenediamine hydrochloride) was then added to 1 mL of each specimen. Absorbance was monitored at 545 nm after 30 min incubation in the dark, the nitrite levels were expressed as μM (Namıduru et al., 2011).
2.3.5. Determination of MDA
MDA was determined by spectrophotometric measurement as an index for lipid peroxidation (Mihara and Uchiyama, 1978). A mixture of 200 μL of 8% sodium dodecyl sulfate, 200 μL of 0.9% TBA and 1.5 mL of 20% acetic acid was added to 200 μL of the hemolysate and 1.9 mL of distilled water was used to bring the volume up to 4 mL. After boiling for 1 h, the mixture was cooled, and 5 mL of a solution of n-butanol and pyridine (15:1 v/v) was added. The mixture was centrifuged at 5000 rpm for 15 min, and the absorbance was measured at 532 nm. MDA levels were calculated using tetraethoxypropane as standard.
2.3.6. Determination of PCC
PCC was quantified based on the reaction of protein carbonyl with 2,4-dinitrophenylhydrazine (Levine et al., 1990). The blood samples were hemolyzed, and proteins were precipitated by the addition of 10% trichloroacetic acid (TCA). The precipitate was resuspended in 1.0 mL of 2 M HCl for blank control or 2 M HCl containing 2% of 2,4-dinitrophenylhydrazine for test samples. After incubation for 1 h at 37 °C, protein samples were washed with alcohol and ethyl acetate and reprecipitated by the addition of 10% TCA. The precipitated protein samples were dissolved in 6 M guanidine hydrochloride, and the absorbance was measured at 370 nm. The molar extinction coefficient of 22 × 103 M−1 cm−1 was used to calculate the PCC level.
2.3.7. Determination of total protein
Total protein content in the hemolysates was assayed according to the method of Lowry et al. (1951). Briefly, 0.5 mL of the hemolysate was precipitated with 0.5 mL of 10% TCA and centrifuged for 10 min, and the precipitate was dissolved in 1.0 mL of 0.1 N sodium hydroxide. From this solution, 0.1 mL was removed and brought to 1.0 mL with distilled water. Then, 4.5 mL of alkaline copper reagent was added, and the sample was incubated at room temperature for 10 min. After the incubation, 0.5 mL of Folin’s reagent was added, and 20 min later, the developed blue color was measured at 620 nm. The total protein concentration was calculated using bovine serum albumin as a standard.
2.3.8. Determination of hemorheological parameters
Erythrocytes count, MCV and RDW were measured using Coulter®Ac·Tdiff™ hematology analyzer. The WBV was measured at shearing rates of 94.5 s−1 and 0.945 s−1 in a Viscometer (Model DV-II+; Brookfield, Middleboro, MA, USA) at 37 °C. The erythrocyte sedimentation rate (ESR) was measured using the Wintrobe tube method (Wintrobe and Landsberg, 1936).
2.3.9. Statistical analysis
Data were expressed as mean ± SD of each group. Data were evaluated by a one-way ANOVA followed by the Tukey–Kramer test for multiple comparisons. Comparison test was performed as appropriate. A probability value of <0.05 was used as the criterion for significance.
3. Results and discussion
The flow properties of blood are among the main determinants of proper tissue perfusion and oxygenation. Changes in blood biorheology play substantial roles in disease processes. Therefore, knowledge of these properties is vital to the understanding of hemorheology. In the present results whole blood GSH content was decreased in all treated groups relative to control samples. Similarly, Pandey and Rizvi (2010) observed that the exposure of whole blood to t-BHP as oxidative stress inducer decreased the GSH level. Also, it has been demonstrated that PTX treatment causes decreasing of antioxidant status (Alexandre et al., 2007; Panis et al., 2012; Hadzic et al., 2010). Likewise, Richards and Nwose (2010) demonstrated that oxidative stress caused a decline of GSH content with increased blood viscosity.
Erythrocytes are coated with a variety of highly glycosylated proteins with SA residues, which are mainly responsible for the negative surface charge of erythrocytes. There is about 2.4 × 107 SA residue per human erythrocyte. The negative surface charge prevents erythrocytes from coming into contact and aggregating (Fan et al., 2012). The SA content of circulating erythrocytes decreases with the aging of erythrocytes. This increase the friction of erythrocytes among themselves, with endothelial cells and rise propensity to oxidative damage to the erythrocyte membrane (Fan et al., 2012). The reduction of SA level is implicated in erythrocytes aggregation (Simmonds et al., 2013). ROS -induces structural alteration of SA residues on the cell surface (Eguchi et al., 2005).
In the current results, the levels of SA were significantly decreased by exposure of blood samples to the tested agents. However, this decrease was more pronounced in the case of PTX and CrEL combination. A similar observation was reported by Goswami and Koner (2002) who found that SA levels were decreased by exposure to oxidative stress. The ROS detach of SA (desialylation) and decrease of SA levels (Goswami and Koner, 2002). Moreover, the glycosidic linkage of SA is a potential target for ROS. Therefore, ROS enhance the cleavage of the glycosidic linkage liberating SA residue from cell surface (Pawluczyk et al., 2014). SA has an important role in decreasing H2O2 concentrations (Iijima et al., 2004). Herein, SA may be consumed in the scavenging of H2O2 induced by PTX and/or CrEL exposure.
NO plays an important role in blood biorheological properties. A decrease of NO leads to an impairment of blood biorheology (Kuwai and Hayashi, 2006; Yerer et al., 2010). Moreover, NO counteracts the oxidative stress by blocking peroxidation of lipids (Plekhova and Somova, 2012). In the present study, nitrite levels were measured as an index for NO production. Exposure of blood samples to tested agents produced a significant decrease in plasma nitrite levels compared to control samples. This effect was more noticeable in the case of t-BHP and PTX plus CrEL. These results are in agreement with several studies reported that oxidative stress leads to impairment of NO production (Yerer et al., 2010; Baskurt et al., 2011). Similarly, it has been demonstrated that, PTX adversely affects blood cells adhesion and aggregation through a decrease in NO production (Serizawa et al., 2012; Miljkovic et al., 2004).
The decrease of antioxidant parameters with the increase of lipid and protein oxidation is associated with increasing blood viscosity (Li et al., 2010; Siciliano et al., 2001). In the current study, a significant increase in levels of MDA and PCC was observed after incubation of blood samples with the tested agents. These results are consistent with former studies, indicating that PTX can increase the production of ROS (Harisa et al., 2013; Hadzic et al., 2010). Also, similar observations were reported by Luqman and Rizvi (2006), who demonstrated that exposure of whole blood to chemicals causes a significant increase in MDA and PCC levels. It has been demonstrated that, increases in lipid peroxidation and protein oxidation were associated with an increase of viscosity (Li et al., 2010; Richards and Nwose, 2010). Table 1 showed the effect of t-BHP, PTX, CrEL or PTX plus CrEL on oxidative stress markers (MDA, PCC and GSH) in whole blood as well as SA and nitrite in plasma after incubation at 37 °C for 24 h with t-BHP, PTX, CrEL or PTX plus CrEL.
Table 1.
Levels of MDA, PCC and GSH in whole blood as well as values of plasma SA and nitrite after incubation at 37 °C for 24 h with t-BHP, PTX, CrEL or PTX plus CrEL.
| Groups |
|||||
|---|---|---|---|---|---|
| Control | t-BHP | PTX | Cr-EL | PTX + Cr-EL | |
| Parameters | |||||
| GSH (μM) | 964 ± 93.5 | 448 ± 57.5a | 641 ± 67.9a | 619 ± 63.8a | 455 ± 64.7a,b |
| SA (mM) | 2.34 ± 0.34 | 0.55 ± 0.08a | 1.54 ± 0.37a | 1.43 ± 0.35a | 0.62 ± 0.16a,b |
| Nitrite (μM) | 66.8 ± 12.6 | 31.5 ± 9.63a | 46.2 ± 6.87a | 44.5 ± 7.49a | 25.5 ± 3.89a,b |
| MDA (μM) | 17.5 ± 2.27 | 33.1 ± 2.32c | 29.3 ± 3.64c | 30.9 ± 2.81c | 35.2 ± 3.72c,d |
| PC (nM/mg Pro) | 3.30 ± 4.55 | 6.80 ± 1.03c | 5.42 ± 0.29c | 5.05 ± 0.69c | 6.47 ± 1.07c,d |
Indicates significant decrease from control.
Indicates significant decrease from PTX-exposed aliquots.
Indicates significant increase from control.
Indicates significant increase from PTX-exposed aliquots.
ROS causes direct structural modification of proteins with subsequent formation of reactive carbonyl groups. Also, proteins are indirectly modified with reactive carbonyl formed by carbohydrates autoxidation (Aydemir et al., 2008). These modifications result in abnormal protein–protein interactions (Traverso et al., 2004) and lipids–proteins interactions (Aydemir et al., 2008). Similarly, Cicha et al. (1999), demonstrated that oxidative cleavage of protein contributes to alterations of blood viscosity. Furthermore, increase in lipid peroxidation rigidifies erythrocytes membrane and induces the cross-linking of hemoglobin with membrane skeletal proteins (Cicha et al., 1999). PTX-induced oxidative damage to blood constituents, hyperstabilizes microtubules and inhibits cytoskeletal restructuring (Hadzic et al., 2010), which affects aggregability and deformability of erythrocytes leading to an increase of WBV.
Erythrocytes aggregation is a physical factor affecting the erythrocyte sedimentation rate (Simmonds et al., 2013). Additionally, WBV was significantly correlated with the erythrocyte sedimentation rate (Tamer et al., 2002). Erythrocyte sedimentation rate test was done to assess erythrocytes aggregation. Herein, erythrocyte sedimentation rate was significantly increased by t-BHP, PTX, CrEL or PTX plus CrEL incubation compared to control cells, as shown in Fig. 1. These results are in agreement with earlier studies which reported that, the erythrocyte sedimentation rate increases in oxidative stress conditions (Maiti et al., 2007; Feijóo et al., 2010).
Figure 1.
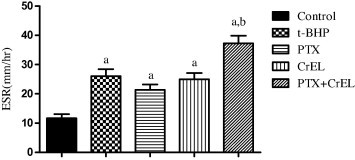
Erythrocytes sedimentation rate of blood samples incubated with t-BHP, PTX, CrEL or PTX plus Cr-EL at 37 °C for 24 h. a: Indicates significant increase from control. b: Indicates significant increase from PTX-exposed aliquots.
The present results showed that, MCV and RDW were markedly higher in blood samples incubated with the tested agents as shown in Table 2. These data are similar to those of previous studies demonstrating that MCV significantly increases upon exposure to oxidative stress and anticancer treatment (Kim et al., 2008; Arslan et al., 2011). These effects are attributed to an increase in erythrocytes aggregation that reduces the number and increases the size of erythrocytes.
Table 2.
Hematological parameters of control erythrocytes as well as erythrocytes incubated with t-BHP, PTX, CrEL or PTX plus CrEL for 24 h at 37 °C.
| Groups |
|||||
|---|---|---|---|---|---|
| Control | t-BHP | PTX | CrEL | PTX–CrEL | |
| Parameters | |||||
| RBCs × 106/μL | 4.93 ± 0.04 | 3.71 ± 0.67a | 3.77 ± 0.06a | 3.34 ± 0.71a | 3.24 ± 0.37b |
| Hb (g/dl) | 14.6 ± 0.86 | 11.6 ± 1.77a | 12.4 ± 0.22a | 9.85 ± 1.76a | 9.40 ± 0.55b |
| Hct (%) | 45.3 ± 1.22 | 34.0 ± 5.11a | 38.8 ± 1.09a | 32.1 ± 5.11a | 28.6 ± 0.92b |
| MCV (fl) | 91.8 ± 2.46 | 99.7 ± 3.07a | 102.1 ± 2.61a | 107.7 ± 3.07a | 108.7 ± 2.56b |
| MCH (pg) | 28.2 ± 2.06 | 24.4 ± 0.55 | 26.8 ± 0.46 | 23.4 ± 0.55 | 22.8 ± 1.51 |
| MCHC (g/dl) | 31.3 ± 1.59 | 28.2 ± 0.77 | 29.3 ± 0.60 | 27. 1 ± 0.77 | 26.8 ± 1.05 |
| RDW (%) | 14.9 ± 2.05 | 16.4 ± 2.24 | 15.7 ± 1.86 | 15.9 ± 2.24 | 18.8 ± 2.42 |
Indicated when significant changes seen from control and/or PTX-exposed samples, respectively, at p < 0.05.
Indicated when significant changes seen from control and/or PTX-exposed samples, respectively, at p < 0.05.
Increase in RDW and MCV is generally caused by either liver disease or hemolytic anemia. However, the present volunteers did not suffer from any diseases; thus, the increase in RDW and MCV is attributed to the effects of the tested agents. In the present investigation, increase in MCV and RDW are additional factors for the increase of WBV. Gluhcheva et al. (2011) reported that blood viscosity was increased by increasing MCV and RDW.
The current study showed that, at high and low shear rates, there is a significant increase in WBV by t-BHP, PTX or CrEL incubation. However, effect of PTX plus CrEL on WBV was more pronounced than other treated blood samples. Figs. 2 and 3., showed WBV at different shearing rates. These findings are consistent with the observations of previous studies by Mark et al. (2001) and Cicha et al. (1999), who demonstrated that blood viscosity was increased after incubation with chemicals. CrEL acts as a solubilizer and may increase the tendency of PTX to interact with the lipid bilayer of erythrocyte membranes (Mark et al., 2001).Therefore, CrEL enhances PTX induced oxidative stress and erythrocyte damage (Panis et al., 2012). Also, it has been reported that oxidative stress increases blood viscosity (Hitsumoto, 2012). However, PTX accelerated erythrocytes aging by an oxidative stress-dependent mechanism (Harisa, 2013). It has been reported that, WBV was increased by aging (Simmonds et al., 2013).
Figure 2.
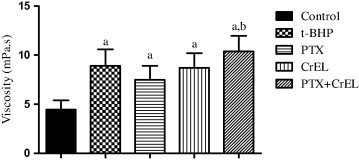
Viscosity of whole blood at high shear rate (94.5 s−1) after incubation with t-BHP, PTX, CrEL or PTX plus CrEL at 37 °C for 24 h. a: Indicates significant increase from control. b: Indicate significant increase from PTX-exposed aliquots.
Figure 3.
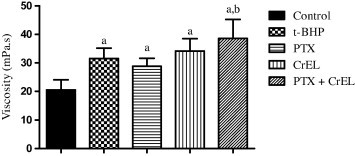
Viscosity of whole blood at a low shear rate (0.945 s−1) after incubation with t-BHP, PTX, CrEL or PTX plus CrEL for 24 h at 37 °C. a: Indicates significant increase from control. b: Indicates significant increase from PTX-exposed aliquots.
4. Conclusion
In conclusion, this study demonstrates that PTX induces oxidative stress evidence by a decrease of GSH, nitrite and SA levels. On the contrary, PTX increases the levels of MDA and PCC. The induction of oxidative stress by PTX was more noticeable in the presence of CrEL. PTX treatment elicits deleterious effect of WBV. Therefore, monitoring of WBV and reducing oxidative stress should be considered during chemotherapy, particularly with PTX. A relatively small sample size was the limitation of this study, large-scale prospective studies are needed to address this issue.
Conflict of Interest
The author has declared that no conflict of interest exists.
Acknowledgements
The author extends his appreciation to the Deanship of Scientific Research at King Saud University, Saudi Arabia for funding the work through the research group project No. RGP-238.
Footnotes
Peer review under responsibility of King Saud University.
References
- Alexandre J., Hu Y., Lu W., Pelicano H., Huang P. Novel action of paclitaxel against cancer cells: bystander effect mediated by reactive oxygen species. Cancer Res. 2007;67(8):3512–3517. doi: 10.1158/0008-5472.CAN-06-3914. [DOI] [PubMed] [Google Scholar]
- Arslan C., Aksoy S., Dizdar O., Kurt M., Güler N., Ozisik Y., Güllü I., Altundag K. Increased mean corpuscular volume of erythrocytes during capecitabine treatment: a simple surrogate marker for clinical response. Tumori. 2011;97(6):711–718. doi: 10.1177/030089161109700606. [DOI] [PubMed] [Google Scholar]
- Awodu O.A., Ajayi I.O., Famodu A.A. Haemorheological variables in Nigeria pulmonary tuberculosis patients undergoing therapy. Clin. Hemorheol. Microcirc. 2007;36(4):267–275. [PubMed] [Google Scholar]
- Aydemir B., Onaran I., Kiziler A.R., Alici B., Akyolcu M.C. The influence of oxidative damage on viscosity of seminal fluid in infertile men. J. Androl. 2008;29(1):41–46. doi: 10.2164/jandrol.107.003046. [DOI] [PubMed] [Google Scholar]
- Baskurt O.K., Meiselman H.J. Blood rheology and hemodynamics. Semin. Thromb. Hemost. 2003;29:435–450. doi: 10.1055/s-2003-44551. [DOI] [PubMed] [Google Scholar]
- Baskurt O.K., Ulker P., Meiselman H.J. Nitric oxide, erythrocytes and exercise. Clin. Hemorheol. Microcirc. 2011;49(1–4):175–181. doi: 10.3233/CH-2011-1467. [DOI] [PubMed] [Google Scholar]
- Beutler E., Duron O., Kelly B.M. Improved method for the determination of blood glutathione. J. Lab. Clin. Med. 1963;61:882–890. [PubMed] [Google Scholar]
- Byrne B., Donohoe G.G., O’Kennedy R. Sialic acids: carbohydrate moieties that influence the biological and physical properties of biopharmaceutical proteins and living cells. Drug Discov. Today. 2007;12(7–8):319–326. doi: 10.1016/j.drudis.2007.02.010. [DOI] [PubMed] [Google Scholar]
- Cicha I., Suzuki Y., Tateishi N., Maeda N. Rheological changes in human red blood cells under oxidative stress. Pathophysiology. 1999;6:121–128. [Google Scholar]
- Eguchi H., Ikeda Y., Ookawara T., Koyota S., Fujiwara N., Honke K., Wang P.G., Taniguchi N., Suzuki K. Modification of oligosaccharides by reactive oxygen species decreases sialyl Lewis x-mediated cell adhesion. Glycobiology. 2005;15(11):1094–1101. doi: 10.1093/glycob/cwj003. [DOI] [PubMed] [Google Scholar]
- Fan W., Yan W., Xu Z., Ni H. Erythrocytes load of low molecular weight chitosan nanoparticles as a potential vascular drug delivery system. Colloids Surf., B. 2012;95:258–265. doi: 10.1016/j.colsurfb.2012.03.006. [DOI] [PubMed] [Google Scholar]
- Feijóo M., Túnez I., Ruiz A., Tasset I., Muñoz E., Collantes E. Oxidative stress biomarkers as indicator of chronic inflammatory joint diseases stage. Reumatol. Clin. 2010;6(2):91–94. doi: 10.1016/j.reuma.2008.12.016. [DOI] [PubMed] [Google Scholar]
- Gluhcheva Y., Ivanov I., Atanasov V., Antonova N., Ivanova J., Mitewa M. Hematological changes in case of chronic cadmium intoxication and monens in detoxication. Relationship with rheological variables. Clin. Hemorheol. Microcirc. 2011;49(1–4):417–422. doi: 10.3233/CH-2011-1491. [DOI] [PubMed] [Google Scholar]
- Goswami K., Koner B.C. Level of sialic acid residues in platelet proteins in diabetes, aging, and Hodgkin’s lymphoma: a potential role of free radicals in desialylation. Biochem. Biophys. Res. Commun. 2002;297(3):502–505. doi: 10.1016/s0006-291x(02)02241-6. [DOI] [PubMed] [Google Scholar]
- Hadengue A.L., Del-Pino M., Simon A., Levenson J. Erythrocyte disaggregation shear stress, sialic acid, and cell aging in humans. Hypertension. 1998;32(2):324–330. doi: 10.1161/01.hyp.32.2.324. [DOI] [PubMed] [Google Scholar]
- Hadzic T., Aykin-Burns N., Zhu Y., Coleman M.C., Leickm K., Jacobsonm G.M., Spitz D.R. Paclitaxel combined with inhibitors of glucose and hydroperoxide metabolism enhances breast cancer cell killing via H2O2-mediated oxidative stress. Free Radical Biol. Med. 2010;48(8):1024–1033. doi: 10.1016/j.freeradbiomed.2010.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harisa G.I. Naringin mitigates erythrocytes aging induced by paclitaxel: an in vitro study. J. Biochem .Mol. Toxicol. 2013 doi: 10.1002/jbt.21544. [DOI] [PubMed] [Google Scholar]
- Harisa G.I., Mohamed F.I., Fars K.A., Gamal A.S. Engineering erythrocytes as a novel carrier for the targeted delivery of the anticancer drug paclitaxel. SPJ. 2013;22(3):223–230. doi: 10.1016/j.jsps.2013.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hitsumoto T. Factors affecting impairment of blood rheology in obese subjects. J. Cardiol. 2012;60(5):401–406. doi: 10.1016/j.jjcc.2012.06.012. [DOI] [PubMed] [Google Scholar]
- Huang Y.X., Wu Z.J., Mehrishi J., Huang B.T., Chen X.Y., Zheng X.J., Liu W.J., Luo M. Human red blood cell aging: correlative changes in surface charge and cell properties. J. Cell. Mol. Med. 2011;15(12):2634–2642. doi: 10.1111/j.1582-4934.2011.01310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iijima R., Takahashi H., Namme R., Ikegami S., Yamazaki M. Novel biological function of sialic acid (N-acetylneuraminic acid) as a hydrogen peroxide scavenger. FEBS Lett. 2004;561(1–3):163–166. doi: 10.1016/S0014-5793(04)00164-4. [DOI] [PubMed] [Google Scholar]
- Kim D.H., Kim Y.K., Won D.I., Shin S., Suh J.S. Assessment of hemorheological deformability of human red cells exposed to tert-butyl hydroperoxide, verapamil and ascorbate by ektacytometer. Korean J. Lab. Med. 2008;28(5):325–331. doi: 10.3343/kjlm.2008.28.5.325. [DOI] [PubMed] [Google Scholar]
- Kuwai T., Hayashi J. Nitric oxide pathway activation and impaired red blood cell deformability with hypercholesterolemia. J. Atheroscler. Thromb. 2006;13(6):286–294. doi: 10.5551/jat.13.286. [DOI] [PubMed] [Google Scholar]
- Lang P.A., Huober J., Bachmann C., Kempe D.S., Sobiesiak M., Akel A., Niemoeller O.M., Dreischer P., Eisele K., Klarl B.A., Gulbins E., Lang F., Wieder T. Stimulation of erythrocyte phosphatidylserine exposure by paclitaxel. Cell. Physiol. Biochem. 2006;18(1–3):151–164. doi: 10.1159/000095190. [DOI] [PubMed] [Google Scholar]
- Levine R., Garland D., Oliver C., Amici A., Climent I., Lenz A., Ahn B., Shaltiel S., Stadtman E. Determination of carbonyl content in oxidatively modified proteins. Methods Enzymol. 1990;186:464–478. doi: 10.1016/0076-6879(90)86141-h. [DOI] [PubMed] [Google Scholar]
- Li G., He H., Yan H., Zhao Q., Yin D. Does carbonyl stress cause increased blood viscosity during storage? Clin. Hemorheol. Microcirc. 2010;44(2):145–154. doi: 10.3233/CH-2010-1263. [DOI] [PubMed] [Google Scholar]
- Lowry O., Rosebrough N., Farr A., Randall R. Protein measurement with the Folin phenol reagent. J. Biol. Chem. 1951;193(1):265–275. [PubMed] [Google Scholar]
- Luqman S., Rizvi S.I. Protection of lipid peroxidation and carbonyl formation in proteins by capsaicin in human erythrocytes subjected to oxidative stress. Phytother. Res. 2006;20(4):303–306. doi: 10.1002/ptr.1861. [DOI] [PubMed] [Google Scholar]
- Lutz H.U., Bogdanova A. Mechanisms tagging senescent red blood cells for clearance in healthy humans. Front. Physiol. 2013;4:387. doi: 10.3389/fphys.2013.00387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiti R., Agrawal N.K., Dash D., Pandey B.L. Effect of pentoxifylline on inflammatory burden, oxidative stress and platelet aggregability in hypertensive type 2 diabetes mellitus patients. Vascul. Pharmacol. 2007;47(2–3):118–124. doi: 10.1016/j.vph.2007.05.004. [DOI] [PubMed] [Google Scholar]
- Mark M., Walter R., Meredith D.O., Reinhart W.H. Commercial taxane formulations induce stomatocytosis and increase blood viscosity. Br. J. Pharmacol. 2001;134(6):1207–1214. doi: 10.1038/sj.bjp.0704387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehdi M.M., Singh P., Rizvi S.I. Erythrocyte sialic acid content during aging in humans: correlation with markers of oxidative stress. Dis. Markers. 2012;32(3):179–186. doi: 10.3233/DMA-2011-0871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihara M., Uchiyama M. Determination of malonaldehyde precursor in tissues by thiobarbituric acid test. Anal. Biochem. 1978;86(1):271–278. doi: 10.1016/0003-2697(78)90342-1. [DOI] [PubMed] [Google Scholar]
- Miljkovic D., Cvetkovic I., Sajic M., Vuckovic O., Harhaji L., Markovic M., Trajkovic V. 5-Aza-2′-deoxycytidine and paclitaxel inhibit inducible nitric oxide synthase activation in fibrosarcoma cells. Eur. J. Pharmacol. 2004;485(1–3):81–88. doi: 10.1016/j.ejphar.2003.11.057. [DOI] [PubMed] [Google Scholar]
- Namıduru E., Tarakçıoğlu M., Namıduru M. Increased serum nitric oxide and malondialdehyde levels in patients with acute intestinal amebiasis. Asian Pac. J. Trop. Biomed. 2011;1:478–481. doi: 10.1016/S2221-1691(11)60104-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogasawara Y., Namai T., Yoshino F., Lee M.C., Ishii K. Sialic acid is an essential moiety of mucin as a hydroxyl radical scavenger. FEBS Lett. 2007;581(13):2473–2477. doi: 10.1016/j.febslet.2007.04.062. [DOI] [PubMed] [Google Scholar]
- Pandey K.B., Rizvi S.I. Protective effect of resveratrol on markers of oxidative stress in human erythrocytes subjected to in vitro oxidative insult. Phytother. Res. 2010;24(1):511–514. doi: 10.1002/ptr.2853. [DOI] [PubMed] [Google Scholar]
- Panis C., Herrera A.C., Victorino V.J., Campos F.C., Freitas L.F., De Rossi T., ColadoSimão A.N., Cecchini A.L., Cecchini R. Oxidative stress and hematological profiles of advanced breast cancer patients subjected to paclitaxel or doxorubicin chemotherapy. Breast Cancer Res. Treat. 2012;133(1):89–97. doi: 10.1007/s10549-011-1693-x. [DOI] [PubMed] [Google Scholar]
- Pawluczyk I.Z., GhaderiNajafabadi M., Patel S., Desai P., Vashi D., Saleem M.A., Topham P.S. Sialic acid attenuates puromycin aminonucleoside-induced desialylation and oxidative stress in human podocytes. Exp. Cell Res. 2014;320(2):258–268. doi: 10.1016/j.yexcr.2013.10.017. [DOI] [PubMed] [Google Scholar]
- Plekhova N.G., Somova L.M. The physiological role of nitric oxide in infectious process. Usp. Fiziol. Nauk. 2012;43(3):62–81. [PubMed] [Google Scholar]
- Richards R., Nwose E. Blood viscosity at different stages of diabetes pathogenesis. Br. J. Biomed. Sci. 2010;67(2):67–70. doi: 10.1080/09674845.2010.11730293. [DOI] [PubMed] [Google Scholar]
- Serizawa K., Yogo K., Aizawa K., Tashiro Y., Takahari Y., Sekine K., Suzuki T., Ishizuka N., Ishida H. Paclitaxel-induced endothelial dysfunction in living rats is prevented by nicorandil via reduction of oxidative stress. J. Pharmacol. Sci. 2012;119(4):349–358. doi: 10.1254/jphs.12067fp. [DOI] [PubMed] [Google Scholar]
- Siciliano L., Tarantino P., Longobardi F., Rago V., de Stefano C., Carpino A. Impaired seminal antioxidant capacity in human semen with hyperviscosity oligoasthenozoospermia. J Androl. 2001;22(5):798–803. [PubMed] [Google Scholar]
- Simmonds M.J., Meiselman H.J., Baskurt O.K. Blood rheology and aging. J. Geriatr. Cardiol. 2013;10(3):291–301. doi: 10.3969/j.issn.1671-5411.2013.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spyridaki M.H.E., Siskos P.A. An improved spectrophotometric method for the determination of free, bound and total N-acetylneuraminic acid in biological fluids. Anal. Chim. Acta. 1996;327:277–285. [Google Scholar]
- Suhr F., Porten S., Hertrich T., Brixius K., Schmidt A., Platen P., Bloch W. Intensive exercise induces changes of endothelial nitric oxide synthase pattern in human erythrocytes. Nitric Oxide. 2009;20(2):95–103. doi: 10.1016/j.niox.2008.10.004. [DOI] [PubMed] [Google Scholar]
- Tamer S., Cefle K., Palanduz S., Vatansever S. Rheological properties of blood in patients with chronic liver disease. Clin. Hemorheol. Microcirc. 2002;26(1):9–14. [PubMed] [Google Scholar]
- Traverso N., Menini S., Maineri E.P., Patriarca S., Odetti P., Cottalasso D., Marinari U.M., Pronzato M.A. Malondialdeyde, a lipoperoxidation- derived aldehyde, can bring about secondary oxidative damage to proteins. J. Gerontol. A Biol. Sci. Med. Sci. 2004;59(9):B890–B895. doi: 10.1093/gerona/59.9.b890. [DOI] [PubMed] [Google Scholar]
- vonTempelhoff G.F., Heilmann L., Hommel G., Pollow K. Impact of rheological variables in cancer. Semin. Thromb. Hemost. 2003;29(5):499–513. doi: 10.1055/s-2003-44641. [DOI] [PubMed] [Google Scholar]
- Wintrobe M.M., Landsberg J.W. Standardized technique for the blood sedimentation test. Am. J. Med. Sci. 1936;189:102. doi: 10.1097/MAJ.0b013e31826caf12. [DOI] [PubMed] [Google Scholar]
- Yerer M.B., Aydogan B., Aydogan S. Sodium nitroprusside-induced oxidative damage on erythrocytes: protective role of carnosine. Ser. Biomech. 2010;25:194–198. [Google Scholar]



