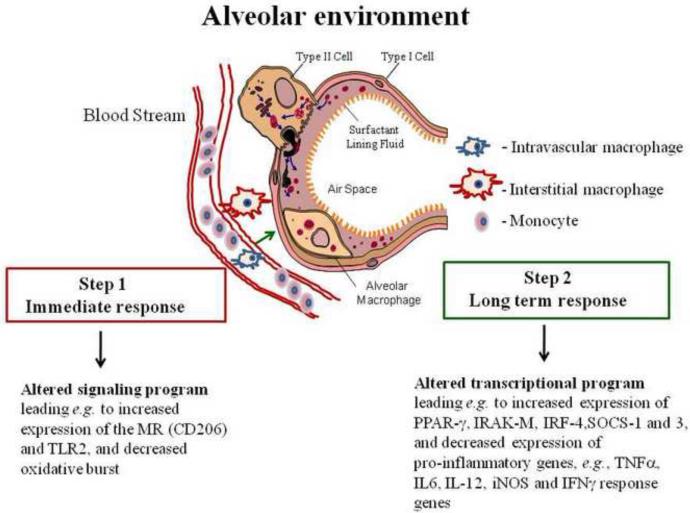
Figure 1. Depiction of the generation of AMs within the alveolar tissue environment.
Blood monocytes traverse the pulmonary alveolar capillary bed and differentiate into intravascular macrophages in situ or transit to the interstitium to become interstitial macrophages (IMs), or to the alveolar space to become AMs (there is also evidence for local production of macrophages in mice). On route, the macrophages are “shaped” by locally produced determinants such as cytokines like GM-CSF, etc. Upon entering the alveolar space, AMs encounter surfactant components which play a role in differentiating these cells to their unique immunoregulatory phenotype, enabling them to acquire their primary function of enhancing clearance of particulates while limiting excessive pro-inflammatory “collateral” damage. Step 1 AM changes are immediate as a result of surfactant components, and other ligands, engaging their cognate receptors to generate a signaling cascade which alters the phenotype and function. Step 2 is long term resulting from an alteration in transcriptional programming. The unique AM phenotype requires constant input from the alveolar environment.