Abstract
AIM: Gastrografin is a hyperosmolar water-soluble contrast medium. Besides its predictive value for the need for operative treatment, a potential therapeutic role of this agent in adhesive small bowel obstruction has been suggested. This study aimed at evaluating the effectiveness of gastrografin in adhesive small bowel obstruction when conservative treatment failed.
METHODS: Patients with adhesive small bowel obstruction were given trial conservative treatment unless there was fear of bowel strangulation. Those responded in the initial 48 h had conservative treatment continued. Patients who showed no improvement in the initial 48 h were given 100 mL of gastrografin through nasogastric tube followed by serial abdominal radiographs. Patients with the contrast appeared in large bowel within 24 h were regarded as having partial obstruction and conservative treatment was continued. Patients in which the contrast failed to reach large bowel within 24 h were considered to have complete obstruction and laparotomy was performed.
RESULTS: Two hundred and twelve patients with 245 episodes of adhesive obstruction were included. Fifteen patients were operated on soon after admission due to fear of strangulation. One hundred and eighty-six episodes of obstruction showed improvement in the initial 48 h and conservative treatment was continued. Two patients had subsequent operations because of persistent obstruction. Forty-four episodes of obstruction showed no improvement within 48 h and gastrografin was administered. Seven patients underwent complete obstruction surgery. Partial obstruction was demonstrated in 37 other cases, obstruction resolved subsequently in all of them except one patient who required laparotomy because of persistent obstruction. The overall operative rate in this study was 10%. There was no complication that could be attributed to the use of gastrografin.
CONCLUSION: The use of gastrografin in adhesive small bowel obstruction after unsuccessful conservative treatment is safe and reduces the need for surgical intervention.
Keywords: Gastrografin, Adhesions, Intestinal obstruction
INTRODUCTION
Adhesive small bowel obstruction is one of the most common surgical causes for admission. More than two-thirds of all small bowel obstructions were due to peritoneal adhesions[1]. At least 3% of patients after laparotomy developed adhesive small bowel obstruction. Adhesive obstruction may occur at any time after surgery, about 20% of the obstructions appeared more than 10 years after the initial abdominal operation[2].
Gastrografin (Schering AG, Berlin, Germany), a water-soluble contrast medium, has been found useful in the management of adhesive small bowel obstruction. A few studies reported that gastrografin could accurately predict the need for surgical treatment[3,4]. Our previous randomized trial on gastrografin showed that the use of this agent after unsuccessful conservative treatment markedly reduced the need for surgery[5]. Since January 2001, we adopted a protocol of offering gastrografin to patients who failed to respond to conservative treatment for 48 h. This study aimed at examining the results of our current management protocol in adhesive small bowel obstruction.
MATERIALS AND METHODS
Patients over 18 years of age admitted through the emergency room to the Department of Surgery, University of Hong Kong Medical Center, Queen Mary’s Hospital with clinical and radiological evidence of adhesive small bowel obstruction were included in this study. Patients with early postoperative obstruction, documented intraabdominal malignancy, inflammatory bowel disease, or history of abdominal irradiation were excluded. A detailed history, including information on previous abdominal surgery and adhesive obstruction, was taken and a complete physical examination was performed for every patient. A nasogastric tube was inserted for decompression, with strict measurement of output. Intravenous fluid replacement was given and electrolyte imbalances were corrected as required. Supine and erect abdominal radiographs were taken. Emergency laparotomy was performed for patients with suspicion of or clinically impending bowel strangulation. Those without fear of bowel strangulation were treated conservatively, with close monitoring of vital and abdominal signs and daily abdominal radiographs. Patients with obstruction that improved clinically or radiologically in the initial 48 h continued to receive conservative treatment. Clinical improvement was defined as the presence of decreased abdominal pain, distension, tenderness or nasogastric tube output, or bowel opening if the patient had constipation on admission. Radiological improvement was defined as a decrease in number of dilated bowel loops or in the diameter of dilated small bowel. Patients who showed neither clinical nor radiological improvement within 48 h were considered failed conservative treatment and gastrografin meal and follow through were performed. The gastrografin study was performed by a radiologist after an informed consent was obtained. One hundred milliliters gastrografin were administered through nasogastric tube, and the transit of contrast followed by fluoroscopy and serial abdominal radiographs. Patients in whom the contrast appeared in large bowel within 24 h were regarded as having partial obstruction. Conservative treatment was continued for these patients. If the contrast failed to reach the large bowel within 24 h, the patient was regarded as having complete obstruction; these patients were treated with laparotomy. Patients that showed no progressive clinical and radiological improvement after 48 h, either in the group of patients who had partial obstruction demonstrated by gastrografin study or in the group solely managed by conservative treatment, also underwent surgery. Complete resolution of bowel obstruction was established when the symptoms and signs of obstruction subsided and abdominal radiographs did not show the small bowel dilated. Complications, death rates, and hospital stays were recorded. A flow chart illustrating the management protocol in the study is shown in Figure 1. Data were prospectively collected and entered into a computer database. SPSS software (SPSS Inc., Chicago, IL) was used for data analysis. Univariate analysis was performed by the Student t test or the Mann-Whitney test for continuous variables and by Fisher exact tests for categorical variables. P<0.05 was considered statistically significant.
Figure 1.
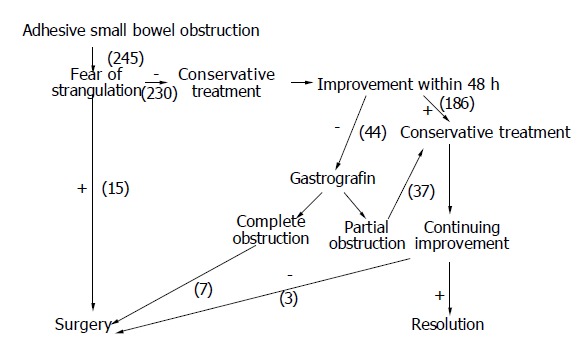
Protocol of study number of cases.
RESULTS
From January 2001 to December 2002, 212 patients (111 men and 101 women) with totally 245 episodes of adhesive small bowel obstruction were included. The mean age (range) was 66 (18-97) years. One hundred and forty-nine patients had single previous abdominal surgery. Colorectal surgery, cholecystectomy, gynecological surgery and appendectomy were the most common single antecedent operations. Sixty-three patients had more than one previous abdominal operation (Figure 2). Fifty-five patients had a prior history of adhesive obstruction.
Figure 2.
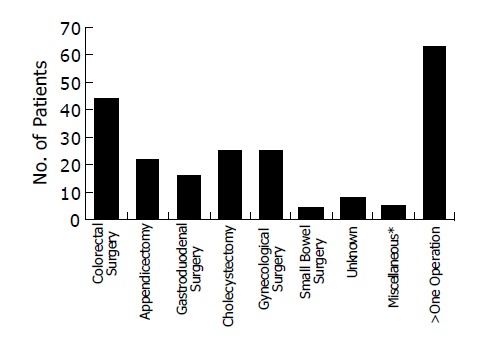
Antecedent operations. *Cystectomy Abdominal wall surgery Nephrectomy Spinal surgery.
The mean duration of symptoms before admission was 1.8 d (range 1-7). Because the duration of nasogastric tube decompression varied with different patients, the average nasogastric tube output of each patient (total amount of drainage/duration) was used for evaluation. For patients who underwent gastrografin study or surgery, only the output before the procedure was considered. The mean output was 23 mL/h (range 0-138).
Fifteen patients had emergency operation performed within 48 h after admission due to fear of bowel strangulation. The majority of them were operated on due to clinically impending bowel strangulation. Laparotomy confirmed strangulation in one patient and the diseased bowel was resected. One hundred and eighty-six episodes of obstruction showed improvement during the initial 48 h, and conservative treatment was continued. Only two patients required laparotomy and enterolysis subsequently because of persistent obstruction. The remaining 184 cases had the bowel obstruction resolved with conservative treatment; the mean time of complete resolution was 56 h (range 5-150) after admission.
Forty-four patients showed no improvement within 48 h. Gastrografin meal and follow through study was performed in these 44 patients. The mean time that the study started was 55 h (range 40-86) after admission. Partial obstruction was demonstrated in 37 patients. Obstruction resolved subsequently in 36 patients at a mean time of 49 h (range 8-117) after the administration of gastrografin. The remaining patient had persistent obstruction after gastrografin study and required operative treatment. There was no evidence of bowel strangulation at the time of surgery. Seven patients had complete obstruction demonstrated by gastrografin study and laparotomy was performed. Strangulation of bowel was noted in one patient and bowel resection was required. One patient, who had enterolysis performed after gastrografin study, developed recurrent small bowel obstruction due to bezoar and required re-operation. There was otherwise no complication in the group of patients who were treated with gastrografin. There was no mortality in this group of patients.
Comparison of patients with successful and unsuccessful conservative treatment showed that the nasogastric tube output was significantly higher in patients who failed to respond to conservative treatment versus those successfully treated conservatively (33 mL/h vs 19 mL/h, P = 0.003). Other variables including sex, age, duration of symptoms before admission and number of previous abdominal operations and adhesive small bowel obstruction were not significantly different between the two groups (Table 1).
Table 1.
Successful vs unsuccessful conservative treatment.
| Successful conservative treatment | Gastrografin n = 184 | P n = 46 | |
| Sex (M/F) | 102/82 | 19/27 | 0.09 |
| Age (mean) | 18-97 (67) | 31-92 (65) | 0.56 |
| Number of operation (mean) | 1-5 (1.4) | 1-3 (1.5) | 0.47 |
| Numberof obstruction (mean) | 0-5 (0.41) | 0-4 (0.6) | 0.28 |
| Duration of symptoms (mean) | 1-7 (1.8) d | 1-5 (1.8) d | 0.95 |
| Nasogastric tube output (mean) | 0-80 (19) mL/h | 5-87 (33) mL/h | 0.003 |
DISCUSSION
Adhesive small bowel obstruction is a common surgical problem, yet there has been no standard protocol for its management. In the absence of bowel strangulation, adhesive obstruction can be treated conservatively. However, the optimal duration of this trial conservative treatment is controversial. There is no definite answer as to when conservative treatment should be considered unsuccessful and operative treatment should be performed.
In a retrospective study, Cox et al, reported that 69% of adhesive obstructions resolved by conservative treatment. Among the cases that had successful conservative treatment, 88% resolved within 48 h[6]. In another study by Sosa et al, a 35% failure rate of non-operative treatment was reported. It was also found that significant complications occurred in those patients with surgery delayed for more than 48 h[7]. Based on the results of these studies, it is reasonable to recommend that adhesive small bowel obstruction can be managed conservatively for 48 h, surgical treatment should be offered promptly if there is no improvement within this time period.
The use of gastrografin in the management of adhesive small bowel obstruction has been evaluated in recent years. Gastrografin is a water-soluble contrast medium composed of sodium diatrizoate, meglumine amidotriozoate and a wetting agent (polysorbate 80). It has an osmolarity of 1 900 mOsm/L, which is approximately six times that of extracellular fluid. In Onoue et al’s study, Gastrografin was given to patients with adhesive obstruction on admission. Of those who had the contrast medium appeared in the colon within 24 h, 98% had the obstruction resolved by conservative treatment. On the other hand, 80% of patients who failed to have the contrast medium shown in the colon within 24 h required operative treatment[3]. Chen et al, have performed a similar study in which another water-soluble contrast medium, Urografin (Schering AG, Berlin, Germany), was used. Urografin has essentially the same composition as that of gastrografin. The main difference between the two agents is that urografin has a lower osmolarity. Similar results were obtained, indeed, the predictive value of water-soluble contrast medium for the need of operative treatment was even higher in the latter study[4].
Gastrografin may also have a therapeutic effect in adhesive small bowel obstruction. Because of its hyperosmolarity, Gastrografin promotes shifting of fluid into bowel lumen and increases the pressure gradient across an obstructive site. The bowel content is diluted and in the presence of the wetting agent, easier passage of bowel content through a narrowed lumen may be allowed. Gastrografin also decreases edema of bowel wall and enhances bowel motility. In a randomized controlled study performed by Assalia et al, about 100 mL of Gastrografin was given on admission to patients in the study group. A significant reduction in the need for operative treatment in the study group was reported[8]. The results of our previous randomized trial also supported a therapeutic role of Gastrografin in adhesive obstruction. Patients who showed neither clinical nor radiologic improvement in the initial 48 h were considered to have conservative treatment failed and underwent either Gastrografin study or surgery. The need for operative treatment was markedly reduced by 74% in the Gastrografin group[5]. Since then it has become our routine to use Gastrografin for patients with failure of conservative treatment.
The administration of Gastrografin in adhesive small bowel obstruction is safe even after unsuccessful conservative treatment. There was no complication or mortality that could be attributed to the use of Gastrografin in the present study. In fact, adverse effects due to the use of Gastrografin in small bowel obstruction have rarely been reported. A potential complication of using Gastrografin in the presence of bowel obstruction is aspiration pneumonia. In our management protocol, Gastrografin was only given after 48 h of conservative treatment. By the time that the contrast medium was administered, the stomach should have been adequately decompressed through nasogastric tube and therefore the risk of aspiration pneumonia minimized. Another potential adverse effect of Gastrografin is that it may further dehydrate a patient with small bowel obstruction because of the shifting of fluid into bowel lumen. The practise of giving Gastrografin at 48 h may also reduce the risk of this adverse phenomenon because the patients should have been adequately rehydrated prior to the administration of Gastrografin.
The incidence of bowel strangulation in patients with adhesive small bowel obstruction ranged from 6% to 11% in previous reports[9-11]. In our study, the overall strangulation rate was 0.8%. Among the 44 patients who had Gastrografin given after unsuccessful conservative treatment, only one patient suffered from strangulation of bowel. There was no evidence that the use of Gastrografin would increase the risk of bowel strangulation.
Surgery was required in 27-35% of patients with adhesive small bowel obstruction according to previous retrospective studies[6,7,10,11]. The overall need for surgical treatment was 10% under our management protocol. To our knowledge, we have achieved the lowest operative rate for adhesive small bowel obstruction in the literature. If we had not used gastrografin, all the 44 cases which showed no improvement in the initial 48 h would have had to be operated on and the overall operative rate in our series would have increased to 25%. We conclude that the use of gastrografin in adhesive small bowel obstruction after unsuccessful conservative treatment is safe and reduces the need for operative treatment.
Footnotes
Science Editor Li WZ Language Editor Elsevier HK
References
- 1.Menzies D. Postoperative adhesions: their treatment and relevance in clinical practice. Ann R Coll Surg Engl. 1993;75:147–153. [PMC free article] [PubMed] [Google Scholar]
- 2.Menzies D, Ellis H. Intestinal obstruction from adhesions--how big is the problem? Ann R Coll Surg Engl. 1990;72:60–63. [PMC free article] [PubMed] [Google Scholar]
- 3.Onoue S, Katoh T, Shibata Y, Matsuo K, Suzuki M, Chigira H. The value of contrast radiology for postoperative adhesive small bowel obstruction. Hepatogastroenterology. 2002;49:1576–1578. [PubMed] [Google Scholar]
- 4.Chen SC, Lin FY, Lee PH, Yu SC, Wang SM, Chang KJ. Water-soluble contrast study predicts the need for early surgery in adhesive small bowel obstruction. Br J Surg. 1998;85:1692–1694. doi: 10.1046/j.1365-2168.1998.00919.x. [DOI] [PubMed] [Google Scholar]
- 5.Choi HK, Chu KW, Law WL. Therapeutic value of gastrografin in adhesive small bowel obstruction after unsuccessful conservative treatment: a prospective randomized trial. Ann Surg. 2002;236:1–6. doi: 10.1097/00000658-200207000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cox MR, Gunn IF, Eastman MC, Hunt RF, Heinz AW. The safety and duration of non-operative treatment for adhesive small bowel obstruction. Aust N Z J Surg. 1993;63:367–371. doi: 10.1111/j.1445-2197.1993.tb00404.x. [DOI] [PubMed] [Google Scholar]
- 7.Sosa J, Gardner B. Management of patients diagnosed as acute intestinal obstruction secondary to adhesions. Am Surg. 1993;59:125–128. [PubMed] [Google Scholar]
- 8.Assalia A, Kopelman D, Bahous H, Klein Y, Hashmonai M. Gastrografin for mechanical partial, small bowel obstruction due to adhesions. Harefuah. 1997;132:629–633. [PubMed] [Google Scholar]
- 9.Miller G, Boman J, Shrier I, Gordon PH. Natural history of patients with adhesive small bowel obstruction. Br J Surg. 2000;87:1240–1247. doi: 10.1046/j.1365-2168.2000.01530.x. [DOI] [PubMed] [Google Scholar]
- 10.Matter I, Khalemsky L, Abrahamson J, Nash E, Sabo E, Eldar S. Does the index operation influence the course and outcome of adhesive intestinal obstruction? Eur J Surg. 1997;163:767–772. [PubMed] [Google Scholar]
- 11.Seror D, Feigin E, Szold A, Allweis TM, Carmon M, Nissan S, Freund HR. How conservatively can postoperative small bowel obstruction be treated? Am J Surg. 1993;165:121–125; discussion 125-126. doi: 10.1016/s0002-9610(05)80414-3. [DOI] [PubMed] [Google Scholar]


