Abstract
Objective
Whether human papillomavirus (HPV) self-testing can expand access to cervical cancer screening will depend on making the test accessible and acceptable to higher-risk women. To evaluate a novel delivery mode, we mailed HPV self-test kits to low-income, under-screened women and assessed their perceptions of self-testing and cervical cancer prevention.
Materials and Methods
We conducted a telephone survey of 199 women in North Carolina. Eligibility criteria included not having had a Pap test in 4 years and reporting 1 or more indicators of economic hardship, such as being uninsured.
Results
Over half (55%) of women in the diverse sample were non-Hispanic black, and almost three-quarters (74%) reported annual household incomes of $20,000 or less. Trust in HPV self-testing was moderate to high, with almost all women (98%) agreeing the mailed test was safe. A few women (6%) preferred HPV self-testing to Pap testing for protecting health, but most (75%) had no preference. Trust in or preference for mailed self-testing did not vary by race or income. However, compared to white women, black women had lower HPV-related knowledge (OR=0.46, 95% CI, 0.23–0.92) and perceived lower cervical cancer risk in the absence of screening (OR=0.44, 95% CI, 0.22–0.86). We found similar patterns of disparities for women with very low (<$10,000) versus relatively higher incomes.
Conclusions
Our findings suggest that, across racial and economic subgroups, under-screened women generally trust HPV self-tests delivered by mail. To succeed, programs for HPV self-testing must overcome disparities in knowledge and perceptions related to cervical cancer screening.
Keywords: human papillomavirus (HPV) testing, self-collection, cervical cancer, health disparities
INTRODUCTION
Each year in the United States, over 4,000 women die from cervical cancer, almost all cases of which are caused by persistent infection with human papillomavirus (HPV) [1]. The highest priority for prevention are women disproportionately affected by cervical cancer mortality, including women who are racial and ethnic minorities, those with low socioeconomic status, and those who have not been recently screened [2–5]. Patterns of disparities in cervical cancer mortality have changed little in recent decades, despite the broader success of provider-based cervical cancer screening programs that have dramatically reduced the burden of disease in the general population [1, 6]. These persistent disparities suggest the need for novel and highly-targeted approaches to reaching the minority of women who are not currently served by existing in-person screening programs.
HPV testing with self-collected sampling (or “HPV self-testing”) is one proposed strategy for expanding access to cervical cancer screening. Using equipment and procedures similar to those that healthcare providers use to conduct HPV testing, HPV self-testing allows women themselves to collect the sample using a brush that extends into the cervico-vaginal canal, albeit less deeply into the cervix. The FDA recently licensed HPV DNA testing as a primary screening test for cervical cancer. By contrast, HPV self-testing is not currently licensed for use in the United States, but extensive population-based research suggests that the sensitivity of the self-test is high for the detection of high-grade cervical lesions [7, 8].
One advantage of HPV self-testing is that kits can be sent through the mail, potentially increasing reach to women who are less likely to come to clinics for Pap tests. Because mailed HPV self-testing is conducted outside of a provider’s office, it may increase access to screening by reducing barriers, such as those related to privacy, transportation, cost, insurance status, or provider availability [9–11]. In the United States, mailed HPV self-testing will not replace provider-based screening, but rather may serve as an outreach strategy to initiate the screening process and identify those women who are most in need of follow-up services.
For mailed HPV self-testing to be worthwhile, women must be willing to use it. Of special importance, the test must be acceptable to higher-risk women who do not regularly participate in cervical cancer screening programs [12]. Although research to date has found that low-income and under-screened women in the U.S. are generally amenable to self-testing [10–12], no studies have evaluated the acceptability of programs that offer HPV testing by mail. Because such programs could increase access to care, we sought to evaluate perceptions of a novel, mail-based approach to HPV self-testing in a diverse sample of low-income, under-screened women in North Carolina. Given disparities in cervical cancer incidence and mortality, we also aimed to better understand how these perceptions varied by demographic characteristics including race and income.
MATERIALS AND METHODS
Participants
We recruited low-income women in North Carolina at high risk for cervical cancer. Eligibility criteria included not having had a Pap test in 4 years and meeting one or more of the following indicators of economic hardship: having an income less than or equal to 200% of the federal poverty level; being eligible for Medicaid; being uninsured; or having children who qualify for a free or reduced-price school lunch program. Additionally, women were between the ages of 30–65 years, the age for which the HPV test is recommended; were not pregnant; and had never had a hysterectomy.
Recruitment and screening occurred in 10 counties classified as “low resource” based on North Carolina Department of Commerce designations of economic well-being [13]. In these counties, we recruited women using several methods: (1) we provided information to women calling the North Carolina 2-1-1 information hotline seeking social services; (2) we distributed informational brochures to community and social service agencies, safety net healthcare clinics, and local health departments; and (3) we encouraged study participants and ineligible callers to share information about the study with friends and family members who might be eligible.
We screened 902 women and invited the 411 who met eligibility criteria to participate. Of those eligible, 211 (51%) women completed study activities. We excluded 12 women from the analytic sample because they did not did not report on their race/ethnicity which was a central variable in this analysis. The final analytic sample consisted of the remaining 199 women.
Procedures
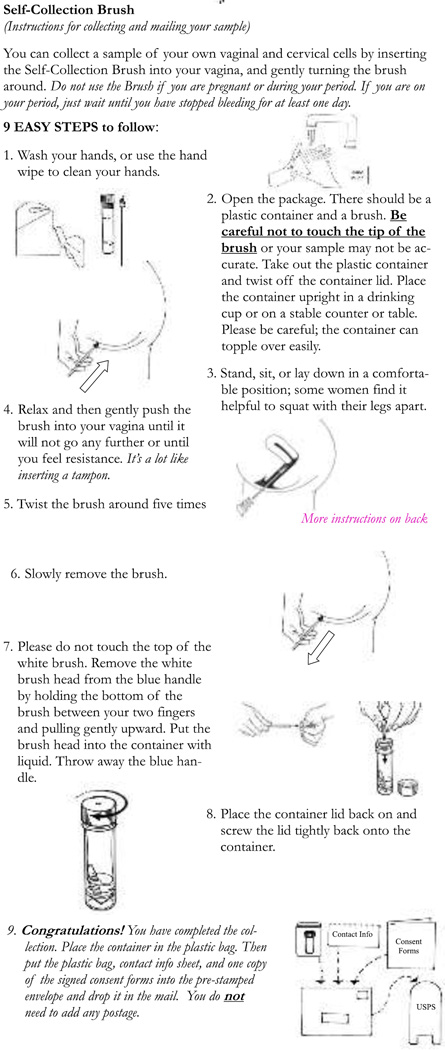
We mailed participants HPV self-testing kits that included a collection vial and brush as well as instructions designed for lower-literacy populations (Figure 1). After using the kits and returning their samples, women participated in a telephone survey after receiving an HPV self-test by mail. Trained interviewers from the American Sexual Health Association contacted each woman and conducted a 15- to 20-minute telephone survey. Women gave written consent and were eligible to receive $10 for completing the survey. The University of North Carolina Institutional Review Board approved the study protocol.
Figure 1.
HPV self-collection kit instructions
Measures
Our main outcomes were psychosocial measures related to three topics: mailed HPV self-testing, HPV, and cervical cancer.
Mailed HPV self-testing
Three items assessed respondents’ trust in HPV self-testing, including belief the test was safe, belief that the mailed self-test gave accurate information about cervical cancer risk (i.e., sensitivity), and belief that a positive self-test result indicated high risk for cervical cancer (i.e., positive predictive value). Using these items, we constructed a composite score of HPV self-test trust. First, we assigned each item a score of 1 to 4 based on 4-point response scales for which a higher score indicated a higher level of trust. We then totaled scores across the three items and dichotomized respondents. Those with scores of 9 or lower had “lower trust” and those with scores of 10 or higher had “higher trust” in the HPV self-test. The survey also assessed respondents’ beliefs about which test they believed protects women’s health better. We scored responses as 1 for the “Pap test,” 2 for “no preference,” and 3 for “HPV self-test.”
HPV
The survey assessed HPV-related knowledge with five items concerning whether HPV causes cervical cancer, genital warts, and herpes and whether HPV is rare and curable. To reduce co-linearity in our final model, we combined these items into an index. We assigned a score of 1 to each correct response. For each respondent, we then calculated the sum of all five items and collapsed scores into two categories: “lower HPV-related knowledge” (scores 0–2) and “higher HPV-related knowledge” (scores 3–5).
Cervical cancer screening
The survey included three items related to cervical cancer screening. First, respondents rated their future likelihood of getting cervical cancer without regular screening using a 4-point response scale ranging from “no chance” to “high chance.” Second, respondents indicated how often they believed women their age should get a Pap test with five responses ranging from never to annually. Lastly, respondents indicated whether their thoughts about the Pap test were mostly negative, mostly positive, or neutral.
Participant characteristics
The survey assessed demographic characteristics, including age, race/ethnicity, educational attainment, health insurance coverage, annual household income and county of residence. We defined counties located within a metropolitan statistical area (MSA) as “urban/ suburban” and those outside an MSA as “rural” [14].
Data analysis
We used logistic and linear regression to assess bivariate associations between demographic characteristics and psychosocial measures related to HPV self-testing, HPV, and cervical cancer screening. We then entered statistically significant (p<0.05) correlates into multivariate models. We analyzed data using Stata Version 12.0 (Statacorp, College Station, TX). All statistical tests were 2-tailed with a critical alpha of 0.05.
RESULTS
Sample characteristics
Most women were non-Hispanic black (55%) or white (33%) (Table 1). About two-thirds (65%) reported being uninsured, and almost one quarter (23%) lacked a high school degree. Most women (86%) reported an annual household income at or below $20,000.
Table 1.
Sample characteristics
| n | (%) | |
|---|---|---|
| Age (years) | ||
| 30–39 | 69 | (35) |
| 40–49 | 74 | (37) |
| 50–65 | 56 | (28) |
| Race | ||
| Non-Hispanic white | 65 | (33) |
| Non-Hispanic black | 109 | (55) |
| Other | 25 | (13) |
| Health insurance coverage | ||
| No | 130 | (65) |
| Yes | 69 | (35) |
| Educational attainment | ||
| Some high school or less | 46 | (23) |
| High school degree | 80 | (40) |
| Some college or more | 73 | (37) |
| Annual household income | ||
| <$10,000 | 85 | (43) |
| $10,000–$20,000 | 62 | (31) |
| >$20,000 | 27 | (14) |
| Not reported | 25 | (13) |
| Urbanicity | ||
| Urban/suburban | 161 | (81) |
| Rural | 38 | (19) |
Note. Percentages may not total 100% due to rounding.
Mailed HPV self-testing
Trust in mailed HPV self-test
Almost all women (98%) somewhat or strongly agreed the HPV self-test was safe. Most (92%) trusted the test moderately or completely in terms of its ability to detect cervical cancer when present (i.e., perceived sensitivity). Despite these positive evaluations of the test, few women (26%) trusted that a positive test result always or most of the time correctly identified women who had cervical cancer (i.e., perceived positive predictive value). With regard to the composite trust score, 12% of women had higher levels of overall trust in the HPV self-test. Women’s overall trust in the HPV self-test was not associated with participants’ demographic characteristics.
Preferred test
When asked whether HPV self-testing or Pap testing protects women’s health better, most said the tests would protect equally well: 19% believed the Pap test protects better and 6% believed the HPV self-test protects better. In multivariate analyses, preference for the HPV self-test was associated with older age (beta: 0.20, 95% CI: 0.04–0.37) and having insurance coverage (beta: 0.15, 95% CI: 0.02–0.29) (Table 2).
Table 2.
Correlates of believing the HPV self-test protects women’s health better than the Pap test
| Believe HPV self- test protects better than Pap testa |
Bivariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| mean | (SD) | beta | (95% CI) | beta | (95% CI) | |
| Age (years) | ||||||
| 30–39 | 1.75 | (0.45) | Ref | Ref | ||
| 40–49 | 1.85 | (0.48) | 0.10 | (−0.06–0.25) | .10 | −0.05–0.25 |
| 50–65 | 1.97 | (0.49) | 0.21 | (0.05–0.38)* | .20 | 0.04–0.37* |
| Race | ||||||
| Non-Hispanic white | 1.88 | (0.49) | Ref | |||
| Non-Hispanic black | 1.83 | (0.47) | −0.05 | (−0.19–0.10) | ||
| Other | 1.83 | (0.47) | −0.05 | (−0.27–0.18) | ||
| Health insurance coverage | ||||||
| No | 1.79 | (0.50) | Ref | Ref | ||
| Yes | 1.96 | (0.42) | 0.16 | (0.03–0.30)* | 0.15 | 0.02–0.29* |
| Educational attainment | ||||||
| Some high school or less | 1.94 | (0.52) | Ref | |||
| High school degree | 1.84 | (0.42) | −0.10 | (−0.28–0.07) | ||
| Some college or more | 1.80 | (0.50) | −0.14 | (−0.32–0.04) | ||
| Annual household income | ||||||
| <$10,000 | 1.89 | (0.41) | Ref | |||
| $10,000–$20,000 | 1.78 | (0.50) | −0.10 | (−0.26–0.05) | ||
| >$20,000 | 1.73 | (0.52) | −0.16 | (−0.36–0.05) | ||
| Not reported | 2.01 | (0.54) | 0.12 | (−0.09–0.33) | ||
| Urbanicity | ||||||
| Urban/suburban | 1.84 | (0.50) | Ref | |||
| Rural | 1.87 | (0.39) | 0.03 | (−0.14–0.20) | ||
Responses as to which test protects better were “Pap test” (coded as “1”), no preference (coded as “2”), and “self-test” (coded as “3”).
Note CI: confidence interval.
p < 0.05
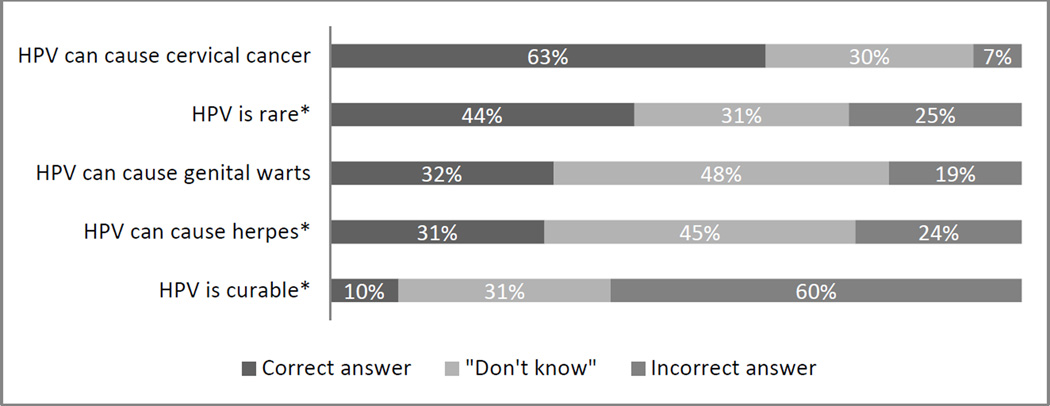
HPV-related knowledge
Women’s HPV knowledge was low (Figure 2). Although a majority of women knew that HPV can cause cervical cancer (63%), fewer correctly indicated that HPV is not rare (44%). Very few knew that HPV can cause genital warts (32%), does not cause herpes (31%), and is incurable (10%).
Figure 2.
Distribution of responses for 5 items in HPV knowledge index (n=198)
* Correct response was “false.”
In bivariate and multivariate analyses, knowledge about HPV correlated with race and income (Table 3). Black women less often held HPV-related knowledge compared to white women (multivariate odds ratio [OR]=0.46, 95% confidence interval [CI]: 0.23–0.92). Women who reported an income greater than $20,000 had almost three times greater odds of having higher HPV-related knowledge (OR= 2.94, 95% CI: 1.15–7.53).
Table 3.
Correlates of HPV-related knowledge (n=198)
| Higher HPV- related knowledgea |
Bivariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| n/N | (%) | OR | (95% CI) | OR | (95% CI) | |
| Age (years) | ||||||
| 30–39 | 21/69 | (30) | 1 | |||
| 40–49 | 18/73 | (25) | 0.75 | (0.36–1.57) | ||
| 50–65 | 20/56 | (36) | 1.27 | (0.60–2.69) | ||
| Race | ||||||
| Non-Hispanic white | 24/65 | (37) | 1 | 1 | ||
| Non-Hispanic black | 24/109 | (22) | 0.48 | (0.24–0.95)* | 0.46 | (0.23–0.92)* |
| Other | 11/24 | (46) | 1.45 | (0.56–3.73) | 1.41 | (0.53–3.69) |
| Health insurance coverage | ||||||
| No | 38/129 | (29) | 1 | |||
| Yes | 21/69 | (30) | 1.05 | (0.55–1.98) | ||
| Educational attainment | ||||||
| Some high school or less | 13/46 | (28) | 1 | |||
| High school degree | 19/79 | (24) | 0.80 | (0.35–1.83) | ||
| Some college or more | 27/73 | (37) | 1.49 | (0.67–3.31) | ||
| Annual household income | ||||||
| <$10,000 | 19/85 | (22) | 1 | 1 | ||
| $10,000–$20,000 | 19/61 | (31) | 1.57 | (0.75–3.31) | 1.53 | (0.72–3.28) |
| >$20,000 | 12/27 | (44) | 2.78 | (1.11–6.94)* | 2.94 | (1.15–7.53)* |
| Not reported | 9/25 | (36) | 1.95 | (0.75–5.12) | 2.00 | (0.75–5.35) |
| Urbanicity | ||||||
| Urban/suburban | 46/160 | (29) | 1 | |||
| Rural | 13/38 | (34) | 1.29 | (0.61–2.74) | ||
Note OR: odds ratio. CI: confidence interval.
Respondents had “high” HPV-related knowledge if they correctly answered three or more items in a 5-item HPV knowledge index.
p < 0.05
Cervical cancer screening
Perceived likelihood of cervical cancer
Overall, 60% of women believed their chance of getting cervical cancer in the future was moderate or high without regular screening. Perceived likelihood of getting cervical cancer varied based on race and income (Table 4). Black women less often believed they had a moderate or high likelihood of getting cervical cancer than white women (OR: 0.44, 95% CI: 0.22–0.86). Women who reported an annual household income of $10,000–$20,000 had lower odds compared to those with incomes under $10,000 (OR: 0.32, 95% CI: 0.16–0.65).
Table 4.
Correlates of perceived likelihood of cervical cancer without regular screening (n=198)
| High/moderate perceived likelihood of cervical cancer without screeninga |
Bivariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| n/N | (%) | OR | (95% CI) | OR | (95% CI) | |
| Age (years) | ||||||
| 30–39 | 37/68 | (54) | 1 | |||
| 40–49 | 49/74 | (66) | 1.64 | (0.83–3.24) | ||
| 50–65 | 32/56 | (57) | 1.12 | (0.55–2.28) | ||
| Race | ||||||
| Non-Hispanic white | 45/65 | (69) | 1 | 1 | ||
| Non-Hispanic black | 56/108 | (52) | 0.48 | (0.25–0.92)* | 0.44 | (0.22–0.86)* |
| Other | 17/25 | (68) | .94 | (0.35–2.55) | 0.94 | (0.34–2.61) |
| Health insurance coverage | ||||||
| No | 78/130 | (60) | 1 | |||
| Yes | 40/68 | (59) | 0.95 | (0.52–1.73) | ||
| Educational attainment | ||||||
| Some high school or less | 30/46 | (65) | 1 | |||
| High school degree | 49/79 | (62) | 0.87 | (0.41–1.86) | ||
| Some college or more | 39/73 | (53) | 0.61 | (0.29–1.31) | ||
| Annual household income | ||||||
| <$10,000 | 60/84 | (71) | 1 | 1 | ||
| $10,000–$20,000 | 29/62 | (47) | 0.35 | (0.18–0.70)* | 0.32 | (0.16–0.65)* |
| >$20,000 | 14/27 | (52) | 0.43 | (0.18–1.05) | 0.43 | (0.17–1.07) |
| Not reported | 15/25 | (60) | 0.60 | (0.24–1.52) | 0.59 | (0.23–1.52) |
| Urbanicity | ||||||
| Urban/suburban | 92/160 | (58) | 1 | |||
| Rural | 26/38 | (68) | 1.60 | (0.75–3.40) | ||
Note OR: odds ratio. CI: confidence interval.
p < 0.05
We assessed perceived likelihood of cervical cancer using a 4-point response scale ranging from “no chance” to “high chance.”
Belief about how often women should get Pap tests
Most women (87%) believed that Pap tests are needed annually rather than less often. Only 2% correctly indicated that screening once every 3 years with Pap testing is appropriate. Compared to those with an annual income under $10,000, women who reported an annual income of more than $20,000 less often endorsed annual testing (OR: 0.26, 95% CI: 0.08- 0.82). Believing women should be annually screened was not associated with other demographic characteristics considered in this study.
Overall thoughts on Pap tests
Respondents had mostly positive (59%) or neutral (28%) thoughts about the Pap test. Thoughts about Pap tests did not differ by demographic characteristics.
DISCUSSION
In this study of low-income North Carolina women rarely or never screened for cervical cancer, we found that trust in HPV self-testing conducted by mail was moderate to high across demographic subgroups. Almost all of the women in our sample believed that the self-test was safe, and only about one-fifth preferred the Pap test over the HPV self-test for protecting health. These findings lend support to an emerging literature that suggests the acceptability of HPV self-testing is high among under-screened women in the United States. Prior studies have found, for example, that a sizeable minority of under-screened women prefer HPV self-testing to provider-based HPV or Pap testing and that women value the convenience and privacy self-testing affords [10, 11, 15]. Given persistent racial- and income-based disparities in cervical cancer incidence and mortality, the absence of variation in trust across demographic subgroups in our sample is encouraging and suggests that programs for self-testing would not exacerbate existing disparities by being less trustworthy to those women who could most benefit from screening.
We were similarly encouraged to find that women trusted the self-test even though they received kits by mail from someone other than their primary healthcare provider. This finding suggests that organizations such as state health departments might play a key role in the initiation of cervical cancer screening via self-testing, thereby centralizing program planning and reducing burden on primary care providers. The approach we used could be especially valuable for overcoming the geographic barriers that can limit access to care for rural populations. Further research is needed to more fully understand how trust and other dimensions of acceptability vary according to factors related to recruitment and service delivery.
In contrast to our findings on trust, we found evidence of disparities with regard to women’s knowledge and perceptions related to cervical cancer screening more generally. Compared to white women, black women were less likely to have accurate HPV-related knowledge or to perceive cervical cancer as likely in the absence of regular screening. These perceptions, which are consistent with our prior research [16], could discourage screening. In addition to variation by race, we found a similar pattern of economic disparities for all three variables, such that women in the lowest income category (<$10,000 annually) were also less likely to have accurate HPV-related knowledge or perceive cervical cancer risk.
In terms of implications for practice, our findings suggest that great care will be needed when communicating the rationale for and benefits of HPV self-testing. Nurses, physicians, and public health program planners cannot assume that under-screened women know about HPV or that they perceive themselves as being at risk for cervical cancer without regular screening. In addition, communicating that most women need screening every three to five years, rather than annually, may serve to encourage screening by reducing the perceived burden of adhering to current guidelines [17]. Attention to these and other sociocultural factors such as acculturation, religiosity, distrust of physicians, and healthcare discrimination may help to ensure equal participation in screening programs despite racial and economic disparities in screening-related knowledge and perceptions.
The findings of this study should be interpreted in light of several limitations, including a modestly-sized sample in one state. At the same time, this study’s sample constitutes one of its primary strengths given that study participants were racially diverse, low-income, under-screened women. This understudied group is a minority in the U.S. population, but stands to gain the most from programs to expand cervical cancer screening through modalities such as HPV self-testing. This study is also one of only a small number to evaluate HPV self-testing in the context of home versus clinic-based provision; it, thus, better approximates how the test would likely be used in actual practice. Further research will be needed to determine how the results of this study generalize to women who are recruited through methods other than those used in this study as well as to women living in other states or countries.
In summary, this study suggests that HPV self-testing holds promise for expanding cervical cancer screening modalities to reach higher-risk women by mailing screening kits directly to them. We found that women indicated moderate to high trust in the self-test, despite receiving it by mail from an organization outside of their usual network of clinical care. Trust in the HPV self-test did not vary across demographic subgroups, but we did find evidence of both racial and economic disparities in cognitions related to cervical cancer more generally such that black and very low-income women were less likely to hold perceptions that support screening. To fully capitalize on the potential of self-testing, healthcare providers and program planners should be aware that some demographic groups may have lower levels of knowledge and perceived risk related to cervical cancer.
Acknowledgements
We would like to thank Andrea Des Marais, Rachel Larsen, Kristen Ricchetti-Masterson, Kelly Murphy, Belinda Yen-Lieberman, and Jerome Belinson for supporting this study.
Sources of funding: This research was supported by Kate B. Reynolds Charitable Trust. Additional support for staff time came from the Cancer Control Education Program at UNC Lineberger Comprehensive Cancer Center (R25 CA57726), the NCCU-LUCC Partnership in Cancer Research (5 U54 CA156733), and an unrestricted gift from GlaxoSmithKline.
Footnotes
Conflicts of interest: JS has received grants from or served on paid advisory boards for Hologic-Genprobe, QIAGEN, and BD Corporation. NB has received grants from or served on paid advisory boards for GlaxoSmithKline and Merck Sharp & Dohme Corp. AR has received grants from Merck Sharp & Dohme Corp. KG, MG, and LB have no conflicts to report.
REFERENCES
- 1.American Cancer Society. Cervical cancer. 2014 Retrieved from: http://www.cancer.org/cancer/cervicalcancer/detailedguide/cervical-cancer-key-statistics. [Google Scholar]
- 2.Singh GK, Miller BA, Hankey BF, Edwards BK. Persistent area socioeconomic disparities in U.S. incidence of cervical cancer, mortality, stage, and survival, 1975–2000. Cancer. 2004;101:1051–1057. doi: 10.1002/cncr.20467. [DOI] [PubMed] [Google Scholar]
- 3.Freeman HP, Wingrove BK. Excess Cervical Cancer Mortality: A Marker for Low Access to Health Care in Poor Communities. Rockville, MD: National Cancer Institute, Center to Reduce Cancer Health Disparities. NIH Pub. No. 05-5282; 2005. [Google Scholar]
- 4.Albano JD, Ward E, Jemal A, Anderson R, Cokkinides VE, Murray T, et al. Cancer mortality in the United States by education level and race. Journal of the National Cancer Institute. 2007;99:1384–1394. doi: 10.1093/jnci/djm127. [DOI] [PubMed] [Google Scholar]
- 5.Simard EP, Ward EM, Siegel R, Jemal A. Cancers with increasing incidence trends in the United States: 1999 through 2008. CA: A Cancer Journal for Clinicians. 2012;62:118–128. doi: 10.3322/caac.20141. [DOI] [PubMed] [Google Scholar]
- 6.National Cancer Institute. SEER stat fact sheet: Cervix uteri. 2014 Retrieved from: http://seer.cancer.gov/statfacts/html/cervix.html.
- 7.Petignat P, Faltin DL, Bruchim I, Tramèr MR, Franco EL, Coutlée F. Are self-collected samples comparable to physician-collected cervical specimens for human papillomavirus DNA testing? A systematic review and meta-analysis. Gynecologic Oncology. 2007;105:530–535. doi: 10.1016/j.ygyno.2007.01.023. [DOI] [PubMed] [Google Scholar]
- 8.Lazcano-Ponce E, Lorincz AT, Cruz-Valdez A, Salmerón J, Uribe P, Velasco-Mondragón E, et al. Self-collection of vaginal specimens for human papillomavirus testing in cervical cancer prevention (MARCH): A community randomized controlled trial. Lancet. 2011;378:1868–1873. doi: 10.1016/S0140-6736(11)61522-5. [DOI] [PubMed] [Google Scholar]
- 9.Balasubramanian A, Kulasingam SL, Baer A, Hughes JP, Myers ER, Mao C, et al. Accuracy and cost-effectiveness of cervical cancer screening by high-risk HPV DNA testing of self-collected vaginal samples. Journal of Lower Genital Tract Disease. 2010;14:185–195. doi: 10.1097/LGT.0b013e3181cd6d36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Litton AG, Castle PE, Partridge EE, Scarinci IC. Cervical cancer screening preferences among African American women in the Mississippi Delta. Journal of Health Care for the Poor and Underserved. 2013;24:46–55. doi: 10.1353/hpu.2013.0017. [DOI] [PubMed] [Google Scholar]
- 11.Anhang R, Nelson JA, Telerant R, Chiasson MA, Wright TC., Jr Acceptability of self-collection of specimens for HPV DNA testing in an urban population. Journal of Women’s Health. 2005;14:721–728. doi: 10.1089/jwh.2005.14.721. [DOI] [PubMed] [Google Scholar]
- 12.Scarinci IC, Litton AG, Garces-Palacio IC, Partridge EE, Castle PE. Acceptability and usability of self-collected sampling for HPV testing among African-American women living in the Mississippi Delta. Women’s Health Issues. 2013;23:e123–e130. doi: 10.1016/j.whi.2012.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.North Carolina Department of Commerce. County tier designations. Retrieved from: https://www.nccommerce.com/research-publications/incentive-reports/2011-county-tier-designations.
- 14.US Census. Geographic Comparability File, 2010 to 2000 county subdivisions. Retrieved from: http://www.census.gov/geo/maps-data/data/comp-sub.html.
- 15.De Alba I, Anton-Culver H, Hubbell FA, Ziogas A, Hess JR, Bracho A, et al. Self-sampling for human papillomavirus in a community setting: Feasibility in Hispanic women. Cancer Epidemiology, Biomarkers & Prevention. 2008;17:2163–2168. doi: 10.1158/1055-9965.EPI-07-2935. [DOI] [PubMed] [Google Scholar]
- 16.Cates JR, Brewer NT, Fazekas KI, Mitchell CE, Smith JS. Racial differences in HPV knowledge, HPV vaccine acceptability, and related beliefs among rural, southern women. Journal of Rural Health. 2009;25:93–97. doi: 10.1111/j.1748-0361.2009.00204.x. [DOI] [PubMed] [Google Scholar]
- 17.American Cancer Society. Cervical cancer: Prevention and early detection. Retrieved from: http://www.cancer.org/cancer/cervicalcancer/moreinformation/cervicalcancerpreventionandearlydetection/cervical-cancer-prevention-and-early-detection-toc.