Abstract
The ectodermal dysplasias are a heterogenous group of diseases, which have one or more anomalies of the hair, teeth, nails, and sweat glands. Hypohidrotic ectodermal dysplasia (HED) is the most common type and is usually transmitted as an X-linked recessive trait. It is characterized by classical triad of hypotrichosis, anhidrosis/hypohidrosis, and hypodontia/anodontia. Here, we describe an Indian boy affected with HED and rare features including ankylosis of temporomandibular joint and cleft palate.
Keywords: Cleft palate, hypodontia, hypohydrosis
Introduction
The ectodermal dysplasias (EDs) are a heterogenous group of diseases, which have one or more anomalies of the hair, teeth, nails, and sweat glands. To date, more than 170 different clinical conditions have been reported. Several ED syndromes may present in association with midfacial defects, such as cleft lip and palate.[1] X-linked hypohidrotic ectodermal dysplasia (XLHED), also known as Christ–Siemens–Touraine syndrome (OMIM 305100) is the most common type followed by autosomal recessive form and autosomal dominant form.[2] HED is characterized by classical triad of hypotrichosis (reduction in the amount of hair of scalp and body hair), anhidrosis/hypohidrosis (absence or reduction of sweat glands), and hypodontia/anodontia (congenital absence of teeth).[3,4] Males are affected severely while females are carrier and show only minor defects.[3] It results from mutations in the ectodysplasin-A (EDA) gene.[5] We hereby report very rare phenotype; cleft palate and ankylosis of temporomandibular joint (TMJ) in an Indian boy with HED.
Case Report
An 11-year-old boy visited genetic clinic with a chief complaint of missing teeth since childhood and facial dysmorphism. He was first in birth order of nonconsanguineous couple, delivered at full term with uneventful prenatal and perinatal period. Mother noted inability to open mouth at birth. He was found to have ankylosis (fusion) of bilateral TMJ with posterior cleft palate on oral examination. He was operated by fusion release of the band of right and left TMJ ankylosis with tracheostomy at 7 months of age. Cleft palate was partially repaired and is persistent yet. Postoperative spiral computed tomography scan of the face and neck at 7 month of age showed posterior cleft palate [Figure 1a and b]. History of present illness revealed that teeth were congenitally missing. There was a history of several episodes of high fever during infancy. Patient's mother noted that he remained warm, especially during the summer and was not able to sweat adequately. He had motor developmental delay as started walking at 2.5 years. The mental development was normal for his age. On examination, at 11 years of age, his weight and height were plotted <3 standard deviation for his age. His skin was dry and scaly. Hair examination revealed fine lusterless appearance with scanty body hair. Facial features revealed sparse scalp hair, frontal bossing, scanty eyebrows and eyelashes, hyperpigmentation around the eyes, depressed nasal bridge, prominent lips, bilateral low set ears [Figure 2a]. Eye examination showed dryness of the cornea and decreased tearing. Intraoral examination revealed two peg-shaped lower canine and two first upper molar teeth, the other were missing, dry mucous membrane, bifid tongue and posterior cleft palate [Figure 2b]. The color of alveolar mucosa and gingiva was normal. Vertical dimension of the lower face is reduced, and vermilion border was not present, giving senile look to the child as compared with children of his age. Hands and feet examination were normal. The nails were thin and brittle. None of the family members has a similar history in previous generations. The routine biochemical tests were within normal limits. Skeletal survey was normal for the age. Echocardiography and ultrasound abdomen were normal. Orthopantomogram revealed malformed incisors, impacted maxillary and mandibular teeth, and true partial anodontia [Figure 3]. Based on the history, oral and cutaneous examination, diagnosis of HED was made. Mutation analysis was not possible due to financial constringent. Patient was evaluated by dentist and planned for removable partial denture after reshaping the existing teeth with composite. As the patient was growing, parents were instructed to defer the placement of the implant until after the completion of jaw growth and eruption of other permanent teeth. Parents were also educated regarding periodic follow-up for modification and replacement. They did not follow for the treatment.
Figure 1.
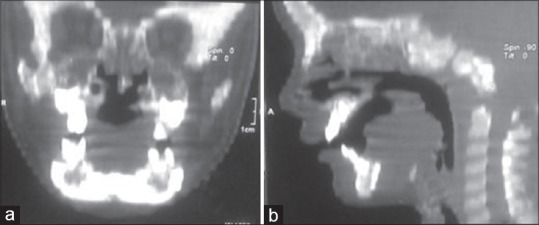
Computed tomography face and neck shows posterior cleft palate. (a) Coronal reconstruction image (b) sagittal section
Figure 2.

(a) Extraoral photograph showing characteristic features of ectodermal dysplasia. (b) Intraoral view shows hypodontia and cleft palate
Figure 3.
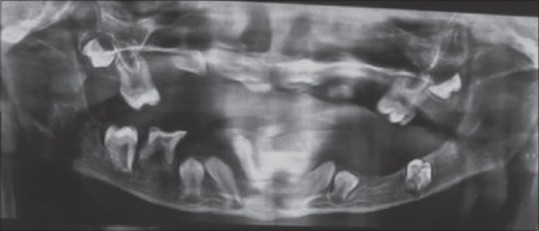
Orthopantomogram shows malformed and impacted incisors and molars with true partial anodontia
Discussion
Hypohidrotic ectodermal dysplasia is inherited in an X-linked recessive (95%), autosomal dominant, or autosomal recessive manner and is caused by mutation in the EDA, EDAR, and EDARADD gene, respectively. These genes regulate the protein EDA A, which forms a signal interaction between ectoderm and mesoderm. Mutation in this gene results in defective EDA A and hence impairs normal development of hair, sweat gland, and teeth. In our case, clinical diagnosis of HED was made based on the history of inability to sweat and hyperthermia, hypodontia, facial, and cutaneous features. Children can experience repeated episodes of hyperpyrexia and heat intolerance, which remain unexplained until the disorder is diagnosed. The interesting features in the present case were presence of TMJ ankylosis and cleft palate. Ankylosis means fusion of the bones forming the joint and caused by poorly-healing severe trauma or infection or congenitally. It was present congenitally along with a cleft palate in our case. In our literature review, this feature is not reported previously along with HED. The association of cleft palate with ED is known in the literature, but with only few cases reported so far. More et al. did retrospective study of 19 cases of ED and found 94.74% had partial anodontia, 84.21% had conical shaped teeth, 05.26% had complete anodontia, 100% had thin alveolar bone; and in one case (05.26%) cleft lip and cleft palate.[6]
The various syndromes which are associated with ED are Rapp-Hodgkin Syndrome, Strandberg-Ronchese's Syndrome, Rosseli-Gulienetti Syndrome, odonto-onycho-dermal dysplasia syndrome.[7] Major differential diagnosis of HED includes Margarita Island type of ED, ectrodactyly–ectodermal dysplasia–cleft (EEC) syndrome (ectrodactyly-ED-cleftlip/cleft palate) and hidrotic ED (clouston type). In Margarita Island type of ED, males and females are affected equally and characterized by cleft lip and palate, scanty eyebrows and eyelashes, sparse scalp hair, protruding ears, hypodontia, and partial syndactyly of the fingers and toes. Sweating is normal.[8] EEC syndrome is characterized by ectrodactyly (absence of all or a portion of one or more fingers and/or toes), cleft lip/cleft palate, hypodontia, nail dysplasia, dry skin fine, sparse, light scalp hair and eyebrows, absent eyelashes. Our case had normal hands and feet, excluded EEC syndrome.[9] Hidrotic ED is characterized by abnormalities involving the nails, hair, skin, and/or teeth with normal sweating.
Hypohidrotic ectodermal dysplasia can be associated with immunodeficiency and hence immunoglobulin levels and T-cell count is required. Laboratory tests include sweat pore counts, Pilocarpine iontophoresis, and skin biopsy. The treatment of HED is a coordinated effort of a multidisciplinary team including pediatricians, dermatologists, dental specialists, otolaryngologists, geneticist, and allergists. It is recommended that children with HED should be live in a cool climate. Preventive and protective measures should be advised including avoidance of physical exertion, protection from high temperatures, and excessive fluid intake during summer, cooling by water such as the use of cool clothes and sponge baths. Early dental intervention and restoration are very important. Reports suggested that children with HED usually suffer from poor psychological and physiological development. They are more likely to remain unaccepted and rejected by peers thus become more aggressive and may experience mental health problems in the adulthood. Therefore, successful dental treatment is required to assist the patient both physically and psychologically. Pigno et al. suggested that an initial prosthesis should be provided before school age of the patient.[10] Prosthodontic treatment commenced at an early age depends on the patient's age, the pattern of dysplasia, morphology of the alveolar ridge, and number and morphology of existing teeth. Treatment includes the use of removable prosthesis during the early stages of growth and when the patient growth is completed, a more stable and fixed prosthesis and of implant can be considered. It was suggested that Cephalometric analysis has a favorable effect on the growth of maxilla and mandible following the placement of dentures.[11] Future trial of Recombinant EDA-A1 administration is going on to correct the features of XLHED.[11] Prenatal diagnosis can be performed using mutation analysis by chorionic villus sampling at 11–12 weeks of pregnancy or indirect prenatal diagnosis may be performed by linkage analysis. In conclusion, an early diagnosis of HED and dental treatment is an essential part of the management because the psychological factor is always there in the absence of teeth thus dentures will give a psychological boost to the self-image of the child.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Shafer WG, Hine MK, Levy BM. Shafer's Textbook of Oral Pathology. 5th ed. Ch. 19. New Delhi: Elsevier Publications; 2006. Diseases of the skin; pp. 1099–102. [Google Scholar]
- 2.Lamartine J. Towards a new classification of ectodermal dysplasias. Clin Exp Dermatol. 2003;28:351–5. doi: 10.1046/j.1365-2230.2003.01319.x. [DOI] [PubMed] [Google Scholar]
- 3.Reed WB, Lopez DA, Landing B. Clinical spectrum of anhidrotic ectodermal dysplasia. Arch Dermatol. 1970;102:134–43. [PubMed] [Google Scholar]
- 4.Soloman LH, Kener EJ. The ectodermal dysplasia. Arch Dermatol. 1980;116:295–9. [Google Scholar]
- 5.Kere J, Srivastava AK, Montonen O, Zonana J, Thomas N, Ferguson B, et al. X-linked anhidrotic (hypohidrotic) ectodermal dysplasia is caused by mutation in a novel transmembrane protein. Nat Genet. 1996;13:409–16. doi: 10.1038/ng0895-409. [DOI] [PubMed] [Google Scholar]
- 6.More CB, Bhavsar K, Joshi J, Varma SN, Tailor M. Hereditary ectodermal dysplasia: A retrospective study. J Nat Sci Biol Med. 2013;4:445–50. doi: 10.4103/0976-9668.117012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saggoo S, Munde A, Hebbale M, Joshi M. Ectodermal dysplasia. J Indian Acad Oral Med Radiol. 2009;21:76–8. [Google Scholar]
- 8.Zlotogora J, Zilberman Y, Tenenbaum A, Wexler MR. Cleft lip and palate, pili torti, malformed ears, partial syndactyly of fingers and toes, and mental retardation: A new syndrome? J Med Genet. 1987;24:291–3. doi: 10.1136/jmg.24.5.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marwaha M, Nanda KD. Ectrodactyly, ectodermal dysplasia, cleft lip, and palate (EEC syndrome) Contemp Clin Dent. 2012;3:205–8. doi: 10.4103/0976-237X.96831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pigno MA, Blackman RB, Cronin RJ, Jr, Cavazos E. Prosthodontic management of ectodermal dysplasia: A review of the literature. J Prosthet Dent. 1996;76:541–5. doi: 10.1016/s0022-3913(96)90015-3. [DOI] [PubMed] [Google Scholar]
- 11.Deshmukh S, Prashanth S. Ectodermal dysplasia: A genetic review. Int J Clin Pediatr Dent. 2012;5:197–202. doi: 10.5005/jp-journals-10005-1165. [DOI] [PMC free article] [PubMed] [Google Scholar]


