Abstract
This study explored the role of organizational factors in the ability of Veterans Health Administration (VHA) clinics to implement colocated mental health care in primary care settings (PC-MH). The study used data from the VHA Clinical Practice Organizational Survey collected in 2007 from 225 clinic administrators across the United States. Clinic degree of implementation of PC-MH was the dependent variable, whereas independent variables included policies and procedures, organizational context, and leaders’ perceptions of barriers to change. Pearson bivariate correlations and multivariable linear regression were used to test hypotheses. Results show that depression care training for primary care providers and clinics’ flexibility and participation were both positively correlated with implementation of PC-MH. However, after accounting for other factors, regressions show that only training primary care providers in depression care was marginally associated with degree of implementation of PC-MH (p = 0.051). Given the importance of this topic for implementing integrated care as part of health care reform, these null findings underscore the need to improve theory and testing of more proximal measures of colocation in future work.
Keywords: Integration of mental health and primary care, PC-MH, Veterans health administration, Organizational correlates
Organizational Correlates of Implementation of Colocation of Mental Health and Primary Care in the Veterans Health Administration
Provision of mental health care in primary care settings (PC-MH) is associated with improvements in care processes and health outcomes (Gilbody et al. 2006; Hedrick et al. 2003), placing the implementation of PC-MH among the most significant and cost-effective service delivery expansions in health care settings (Butler et al. 2008; Chalk et al. 2010). However, mental health and medical care systems are characterized by different philosophies, approaches, and cultures that impede implementation of PC-MH (Weisner et al. 2001). Colocating care is challenging even in large health systems that provide both types of services, such as the Veterans Health Administration (VHA) of the U.S. Department of Veterans Affairs. Although the VHA has experienced significant structural transformation in the organization and delivery of integrated care during the last 20 years (Oliver 2007; Pomerantz and Sayers 2010), there is limited understanding of the organizational factors that support colocation of care. Co-location of mental health care in primary care settings in the VHA system can be defined as the presence of mental health professionals who provide services in a primary care setting—specifically, mental health providers operating in a dedicated space within a primary care clinic that is centrally located and offers ease of access to every provider (Dundon et al. 2011). When fully implemented, such arrangements locate mental health and primary care providers “in the thick of things,” or where the core clinical activity occurs (Dundon et al. 2011, p. 31). As such, co-location is considered one of the most substantial moves toward development of integrated care, because it is intended to facilitate care coordination and communication between providers and increase access for patients (Butler et al. 2008). The aim of this study was to identify the relationship between promising organizational factors and the uptake of PC-MH services in the VHA system.
Of the veterans served by the VHA, 40 % report comorbid behavioral and physical health conditions (Hankin et al. 2006). Recognizing the need for comprehensive and collaborative care, the VHA first integrated primary care and mental health in the mid-1990s with the creation of the Veterans Integrated Service Networks as part of a systemwide transformation (Edmondson et al. 2008; Kizer et al. 1997). This integration of services substantially increased the VHA's ability to successfully deliver mental health care in primary care settings, enhancing veterans’ access to integrated care (Jha et al. 2003). More recently, following the enactment of VHA's Uniform Mental Health Services package in 2008 (VHA 2008), various VHA facilities developed collaborative PC-MH programs that improved detection of mental health needs, referral to mental health specialists when appropriate, and coordination of ongoing patient care (Post et al. 2010; Zivin et al. 2010). These programs spread rapidly throughout the VHA between 2007 and 2012, with 97 % of VHA medical centers reporting some level of colocated PC-MH services in 2012 (Wray et al. 2012).
Embedding mental health treatment in collaborative primary care settings has enabled primary care units to improve mental health screening, diagnosis, and treatment referrals (Zivin et al. 2010). However, recent service outcome data have suggested variation in PC-MH services and inconsistent quality of coordination across sites (Wray et al. 2012). Several qualitative studies have demonstrated that internal organizational factors act as enablers of or barriers to the delivery of integration models in the VHA (e.g., Chang et al. 2013; Fickel et al. 2009), but there is limited research on the organizational context that promotes organizational change in large health care systems, such as the VHA. Federal agencies and the Institute of Medicine have emphasized the examination of functional components of organizational change to inform the development of comprehensive and integrated systems of care (Agency for Healthcare Research and Quality 2013; Rosenberg 2003; Sung et al. 2003). Evaluating the role of organizational factors in the implementation of PC-MH in one of the largest integrated health care systems in the United States can provide critical knowledge about how to improve service integration.
Conceptual Framework of PC-MH in the VHA System
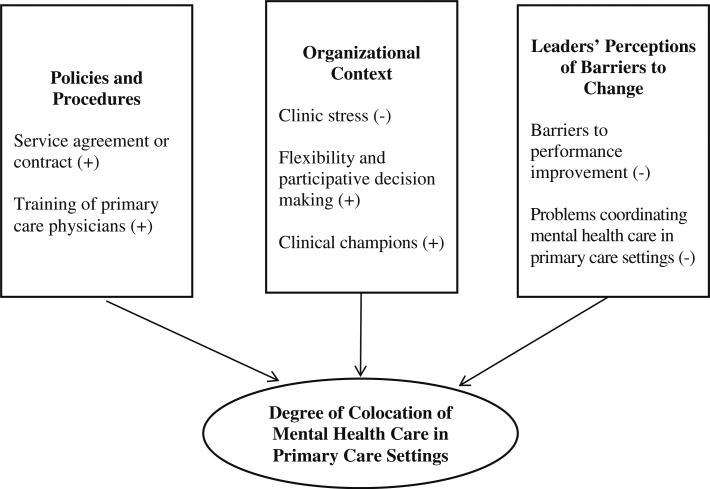
Research has identified broad enablers of and barriers to delivery of PC-MH, including policies and procedures, organizational context, and leaders’ perceptions of barriers to change (Butler et al. 2008; Fickel et al. 2009). These factors informed our conceptual framework of colocated care (see Fig. 1) applied specifically to the VHA system. In particular, we considered the structure and organization of service delivery in the VHA system to explore facilitators (e.g., existing policies, procedures and training, organizational context, and leaders’ perceptions of change) and barriers (e.g., lack of resources for improvement and maintaining champions of change and problems coordinating PC-MH).
Fig. 1.
Organizational enablers of and barriers to the implementation of colocated of mental health care in primary care settings in Veterans Health Administration clinics
Policies, Procedures, and Training
Because primary care and mental health services are generally provided in different settings and characterized by different service delivery cultures, colocation requires policies that establish formal service agreements and provide guidance regarding service delivery. Research has suggested that the establishment of specific treatment protocols and service agreements among programs is a promising strategy to promote delivery of integrated care practices (Zapka et al. 2005). In addition, provision of training across programs has been associated with service integration (Benzer et al. 2012; Chang et al. 2013). Medical personnel who are not mental health specialists can be trained in the diagnosis and treatment of depression (Ell et al. 2007; Rubin et al. 1993), whereas mental health providers can be trained in the complexity of serving patients with medical comorbidities, such as individuals with diabetes and depression (e.g., Chiverton et al. 2007). In addition to providing skills and knowledge, training can increase understanding of and appreciation for the benefits of integrated care.
Organizational Context
Studies on systems change in health and human services organizations have stressed the importance of supportive cultures that allow flexibility for professionals to identify issues in quality of care, provide feedback, and refine practices (Aarons et al. 2011; Glisson and James 2002). When providers have the ability to take initiative, participate in decision making, and act proactively, their capacity to implement program changes increases (Baer and Frese 2003). However, when cultures are characterized by stress, as is commonplace in the hectic environments of health services organizations, the ability of providers to implement new practices may be compromised (Aarons et al. 2011; Glisson et al. 2006; Guerrero and Kim 2013). Providers struggling to manage busy schedules and heavy workloads may be limited in their capacity to follow new practice guidelines, especially in unsupportive environments (Mohr et al. 2013).
Leaders’ Perceptions of Barriers to Change
Research has emphasized the significant role of leaders in advocating the implementation of new practices in PC-MH, particularly those that challenge established routines, internal subcultures, and target outcomes (Aarons et al. 2011; Donahue et al. 2013; Young 2000). Studies on integrating care in the VHA have indicated that leadership plays an important role in terms of allocating resources, resolving conflicts, bridging services, defining job duties, supporting providers, and identifying clinical champions of change (Benzer et al. 2012; Kirchner et al. 2010). Given the influence of leaders, their attitudes toward change— including perceptions of barriers to performance improvement and retention of key staff members—can affect how integrated service delivery programs are implemented. In particular, leaders’ assessment of problems coordinating PC-MH in primary care units is likely to be associated with difficulty colocating care.
Barriers to Performance Improvement
The implementation and sustainment of change in health care organizations require the mobilization of organizational resources (Mendel et al. 2008). These resources include financial, social, and human capital such as adequate funding for change, support of key stakeholders, and adequate administrative and supportive staffing. Studies have demonstrated that organizations that have adequate resources to support provider performance and that are oriented toward quality improvement are more likely to successfully integrate care (Chang et al. 2013; Lehman et al. 2002). Conversely, insufficient staffing, funding, technology, and management support can act as barriers to PC-MH (Benzer et al. 2012). If leaders perceive inadequate support or resources for program changes, implementation of colocated care is likely to be hindered.
Barriers to Maintaining Clinical Champions
The VHA often utilizes clinical champions when implementing new programs and guidelines (Box et al. 2010; Gordon et al. 2011). These champions are often widely respected clinicians who act as change agents during processes such as implementation of PC-MH. They serve as contact points and disseminate information about implementation activities to both patients and staff (Kirchner et al. 2010). The use of clinical champions of depression treatment in primary care has been associated with the colocation of mental health care in primary care settings in the VHA (Chang et al. 2013). However, clinical champions must take time away from other duties such as direct patient care, leading to challenges maintaining their champion role (U.S. Department of Veterans Affairs, 2012). Because the use of clinical champions can be an integral part of implementing change, difficulty maintaining champions may lead to problems with implementation.
Hypotheses
As reviewed earlier, researchers have correlated organizational factors with provider attitudes and uptake of program changes. However, it is unclear how the capacity of VHA clinics to deliver PC-MH is influenced by organizational policies (e.g., service agreements and cross-disciplinary training), organizational context (e.g., clinic stress, flexibility in decision making, and participatory decision making), and leaders’ perception of barriers to change (e.g., barriers to performance improvement, difficulty maintaining clinical champions, and problems coordinating PCMH).
This study aimed to evaluate how each of these factors may act as an organizational barrier to or facilitator of colocation of mental health care in primary care settings in the VHA system. Clinic stress, barriers to improving performance, and problems coordinating PC-MH may be classified as potential barriers to implementation of colocation, whereas flexibility and participation in decision making, the existence of a service agreement or contract to coordinate depression screening and treatment, and provision of training in depression care for primary care providers may act as facilitators of the colocation process (see Fig. 1). The following exploratory hypotheses were tested.
Hypothesis 1 Clinic stress, barriers to performance improvement, and problems coordinating PC-MH would be negatively related to a clinic's degree of implementation of colocated mental health care in primary care settings.
Hypothesis 2 Flexibility and participative decision making, the existence of a service agreement or contract to coordinate depression screening and treatment, provision of training in depression care for primary care providers, and the presence of a clinical champion of depression care would be positively related to a clinic's degree of implementation of colocated mental health care in primary care settings.
Methods
Sample
The VHA Clinical Practice Organizational Survey (CPOS) was conducted in 2007 to measure key clinical practice characteristics associated with VHA performance to inform the development of evidence-based strategies to improve quality of care. The target sample consisted of 250 VHA facilities that met caseload and workload criteria (Farmer et al. 2011; Yano et al. 2008). Specifically, the CPOS was sent to primary care directors at 250 geographically distinct VHA medical centers and community-based outpatient clinics that served 4,000 or more unique outpatient clients and conducted 20,000 or more outpatient visits during the previous year. The survey instrument included items regarding the organization and management of primary care at each site, with a focus on program characteristics such as structure, resources, practice arrangements, and quality improvement. Participants completed the survey via express mail or an emailed electronic version that could be completed online. Repeat mailings were sent to nonresponders after 4 weeks, with email and telephone follow-up from research and primary care staff, resulting in a 90 % response rate (n = 225). The research was approved by the institutional review board of the VA Greater Los Angeles Healthcare System.
Dependent Variable
The study's dependent variable was degree of implementation of colocated mental health care in primary care settings. Respondents were asked, “Do the following models of integrating mental health (MH) services in primary care exist at your site?” Subquestions focused on mental health colocated in primary care (i.e., mental health provider located in primary care setting). Degree of implementation was measured with an ordinal response scale, with increasing degrees of implementation across the following four response options (1) neither planned nor implemented, (2) planned but not implemented, (3) partially implemented, and (4) fully implemented. See Table 1 for descriptive statistics of all variables.
Table 1.
Characteristics of Participating VHA Facilities (N = 225)
| n (%) | M (SD) | |
|---|---|---|
| Dependent variable | ||
| Degree of implementation of PC-MH | ||
| Neither planned nor implemented | 53 (23.8) | |
| Planned but not implemented | 63 (28.3) | |
| Partially implemented | 46 (20.6) | |
| Fully implemented | 61 (27.4) | |
| Independent variables | ||
| Clinic stress | 3.57 (.75) | |
| Barriers to improving performance | 2.65 (.53) | |
| Flexibility and participation | 3.20 (.86) | |
| Service agreement/contract | 199 (88.4) | |
| Training PC providers in depression care | 178 (79.1) | |
| Problems coordinating PC-MH | 23 (10.2) |
MH mental health care, PC primary care, PC-MH mental health care in primary care settings, VHA, veterans health administration
Independent Variables
Policies, Procedures, and Training
The analysis included a dichotomous variable indicating whether each site had partially or fully implemented (vs not implemented) a service agreement or contract between primary care and mental health clinics for coordinated depression screening and treatment. An additional dichotomous variable indicated whether primary providers at the site were trained in the use of guidelines or protocols for depression care.
Organizational Context
As a measure of clinic stress, respondents were asked to indicate their level of agreement with six statements, such as “This practice is almost always in chaos” and “It is hard to make any changes in this practice because we are so busy seeing patients.” Response options ranged from 1 (strongly disagree) to 5 (strongly agree), with a neutral midpoint. Cronbach's alpha for the six items was 0.87. The six scores were averaged for each site to create an overall score.
Two items assessed the extent to which each facility was viewed as flexible toward change and encouraging of staff participation in decision making, with response options of (1) not at all, (2) very little, (3) some, (4) great, (5) very great, and (6) don't know. After recoding two “don’t know” responses (0.8 % of the sample) to missing, the pairwise correlation between the two items was 0.73. The two scores were averaged for each site to create a summary score of flexibility and participation that ranged from 1 to 5.
Problems Coordinating Mental Health Care in Primary Care Settings
Respondents were presented with a statement: “Many veterans have multiple chronic illnesses which require coordination with other clinics, providers, and services to obtain consults, tests, and procedures in a timely way.” Participants were asked, “How often do the primary care providers in your clinic encounter problems with the following subspecialty clinics or ancillary services when trying to coordinate care for their patients with multiple chronic illnesses?” We used responses to the mental health category to evaluate the frequency with which primary care providers had problems coordinating mental health care for their patients, with the following response options: never, rarely, occasionally, often, and always. Given the skewed distribution towards never, rarely, or occasionally, responses were coded as 1 (often or always) or 0 (never, rarely, or occasionally).
Leadership Perceptions of Barriers to Change
The questionnaire included eight questions about perceived barriers to performance improvement, such as limited financial resources, resistance from local managers, and insufficient administrative and support staffing. Respondents were asked to indicate whether they perceived each item as (1) not a barrier, (2) a small barrier, (3) a moderate barrier, or (4) a large barrier. Cronbach's alpha for the eight questions was 0.76. The eight scores were averaged for each site to create a summary score of performance barriers that ranged from 1 to 4.
Presence of a Clinical Champion of Depression Care
The questionnaire included two questions regarding whether each clinic had a designated local clinical champion of depression screening and treatment. Responses to these two questions were used to create a dichotomous independent variable coded as 1 if the clinic had such a champion and 0 if not.
Data Analysis
Stata/SE (version 12) was used to conduct all analyses. We estimated Pearson product-moment correlations of the aforementioned variables. We then fitted a multiple linear regression with degree of implementation of PC-MH as the dependent variable. Each respondent (clinic manager) represented a single clinic, so clinics were the unit of analysis. Table 1 displays characteristics of participating VHA facilities.
Results
VHA facilities reported much variation in the degree of implementation of colocated care. Although almost half of the sampled facilities reported implementing colocated care, the degree of implementation varied, with 20.6 % reporting partial implementation and 27.4 % reporting full implementation. The other facilities were either in the planning stages (28.3 %) or had not initiated efforts (23.8 %).
The bivariate analysis showed that depression care training for primary care providers (r = 0.16, p < 0.05) and clinics’ flexibility and participation (r = 0.15, p < 0.05) were both positively correlated with degree of implementation of PC-MH. Other bivariate correlations revealed expected relationships among some of the main variables of interest (Table 2). Clinic stress was positively associated with barriers to improvement (r = 0.48, p < 0.001) and negatively correlated with flexibility and participation (r = −0.27, p < 0.001). Barriers to improvement were negatively associated with flexibility and participation (r = −0.20, p < 0.01). A positive correlation was found between depression care training for primary care providers and having a service agreement or contract to coordinate care (r = 0.17, p < 0.05). Depression care training for primary care providers was positively associated with having a clinical champion of depression care (r = 0.21, p < 0.001). Finally, problems coordinating PC-MH were negatively related to potential enablers of PC-MH, namely flexibility and participation (r = −0.17, p < 0.05) and service agreements or contracts (r = −0.16, p < 0.05), and positively associated with barriers to improvement (r = 0.20, p < 0.01).
Table 2.
Correlations among study variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| Clinic stress | |||||||
| Barriers to improvement | 0.48*** | ||||||
| Flexibility and participation | –0 27*** | –0.20** | |||||
| Service agreement or contract | –0.09 | –0.05 | 0.08 | ||||
| Clinical champion for depression care | –0.05 | 0.05 | 0.05 | 0.02 | |||
| Training PC providers in depression care | 0.001 | 0.02 | 0.10 | 0.17* | 0.21*** | ||
| Problems coordinating PC-MH | 0.10 | 0.20** | –0.17* | –0.16* | 0.09 | –0.01 | |
| Degree of implementation of PC-MH | –0.09 | –0.08 | 0.15* | –.04 | 0.06 | 0.16* | –0.11 |
MH mental health care, PC primary care, PC-MH mental health care in primary care settings
p < 0.05
p < .01
p < .001
Although problems coordinating PC-MH was not associated with degree of implementation of PC-MH at p < 0.05, the relationship was negative as expected and observation of patterns by level of implementation also varied as expected. Cross-tabulation of these two measures showed that as categories moved toward full implementation (neither planned nor implemented to fully implemented), fewer VHA clinics reported problems with coordination—from an 11 % prevalence of problems among clinics that had neither planned nor implemented colocated care to a 4 % prevalence of problems among clinics with fully implemented colocated care.
Findings did not support Hypothesis 1, which posited that clinic stress, barriers to performance improvement, and problems coordinating PC-MH would be negatively related to degree of implementation of PC-MH. As shown in Table 3, there were no statistically significant relationships between these barriers to improvement and implementation of PC-MH.
Table 3.
Multiple Linear Regression of Colocated Mental Health in Primary Care (n = 214)
| Degree of Implementation of PC-MH | ||
|---|---|---|
| Clinic characteristics | B (SE) | p |
| Barriers | ||
| Clinic stress | –0.10 (0.12) | 0.398 |
| Barriers to improving performance | –0.14 (0.16) | 0.403 |
| Problems coordinating PC-MH | –0.33 (0.26) | 0.209 |
| Enablers | ||
| Flexibility and participation | 0.13 (0.10) | 0.187 |
| Service agreement or contract | –0.38 (0.28) | 0.179 |
| Training primary care providers in depression care | 0.39 (0.20) | 0.051 |
| Clinical champion of depression care | 0.12 (0.18) | 0.521 |
| Alpha (α) | 2.86 (0.68) | <0.001 |
| Adjusted R2 | 0.031 | |
Analytic sample size was 214 due to nine clinics with missing data. PC-MH, mental health care in primary care settings
Findings partially supported Hypothesis 2, which posited that flexibility and participation, the existence of a service agreement or contract to coordinate depression screening and treatment, provision of training in depression care for primary care providers, and the presence of a clinical champion of depression care would be positively related to degree of implementation of PC-MH. Only provision of training in depression care for primary care providers was marginally related to implementation of colocated care (p = .051). As a post hoc sensitivity analysis, we refitted this model to the 23 sites that reported problems coordinating mental health care in primary care settings. None of the covariates in this model was associated with implementation of PC-MH in this subgroup of clinics.
Discussion
This study highlighted perceptions of clinical leaders regarding barriers to performance improvement as an organizational factor of importance in the coordination of PC-MH. Although problems coordinating PC-MH was correlated with units with lower flexibility, participation, and service agreements or contracts, it was not related to implementation of PC-MH. Further, clinics reporting more problems coordinating PC-MH reported lower degrees of implementation of colocated care; however, this association was not statistically significant.
The only statistically significant finding, that training primary care providers in depression care was associated with degree of implementation of PC-MH, was marginally significant (p = 0.051). These preliminary null findings are important for the VHA health system because the Affordable Care Act has bolstered parity legislation promoting the integration of primary care and mental health services (National Council for Behavioral Health 2013). Enhancing our understanding of relevant organizational factors associated with the implementation of PC-MH in the VHA is critical and requires further investigation.
The VHA has undergone significant transformation during the last 15 years, including the adoption of an integrated care model (Chang et al. 2013; Edmondson et al. 2008; Young 2000). Yet full implementation of this model throughout the country and particularly the effective integration of primary care in mental health settings has been challenging. More than 100 years of research on leadership has indicated that leaders play a significant role in the change process in organizations (Yukl 2012), and it is clear that VHA leaders have been regarded as the driving force of transformational change leading to higher quality of care (Edmondson et al. 2008). Previous work has suggested that having a clinical champion for depression treatment is associated with PC-MH, but only among a subgroup clinics reporting full implementation (Chang et al. 2013). Although the role of clinic champions in facilitating colocation was not explicitly tested in the current study, it is surprising that their presence and perceptions of barriers to change were not related to higher degrees of implementation of colocated care in a nationwide sample of VHA programs.
Limitations
Several issues complicated our analysis of the relationships between organizational factors and the implementation of PC-MH in the VHA system and should be considered when interpreting these findings. The cross-sectional structure of the survey data and the existing conceptual frameworks did not allow for establishing causality, directionality, or analysis of the implementation of practices over time. Explored factors may be bidirectional (e.g., problems coordinating mental health care may lead to clinic stress). We also relied on clinic leaders as key informants to assess information (e.g., organizational culture, clinic stress) that is typically collected from departmental or organizational units and validated by group agreement. Managers are generally subject to response bias that may result in minimizing problems with coordination due to social desirability (Marsden et al. 2006; Scholle et al. 2008). However, in this study biased reporting was minimized because the survey was administered internally by VHA researchers who had access to validating information. Finally, although significant efforts were made to include clinic measures that were theoretically and empirically relevant to the delivery of PC-MH, few statistically significant relationships were found. This issue highlights the need for more refined and proximal measures of service delivery changes in the VHA system (e.g., targeted institutional support in terms of funding and human resources for integration). Therefore, this study represents a preliminary view of co-location efforts and challenges as perceived by clinical administrators of a large and diverse group of VHA health providers across the United States.
Despite these methodological challenges, this analysis of a sample of VHA clinics related to organizational factors associated with PC-MH is one of few studies on this topic conducted in the VHA system. As such, this study highlights the importance of searching for proximal and theoretically driven organizational factors that may enable programs to colocate mental health care in primary care settings to serve a significant population of veterans requiring comprehensive integrated care.
Future Research
Our study found no statistically significant associations between variables of interest, highlighting the importance of future studies to identify critical factors that may contribute to colocation of mental health care in primary care settings in one of the largest health care systems in the United States. Further exploration should focus on active enablers of colocation, such as cross-competence training for key staff, efforts to reduce attitude- and resource-based barriers to integration, and enhancing the ability of leaders to initiate, supervise, and evaluate efforts to implement PCMH services. Future research should also rely on both qualitative and quantitative methods to identify theory-driven, proximal, and multilevel factors, including health care reform regulation, Medicare and Medicaid payment incentives, and efforts by providers to offer colocated services for millions of veterans across the nation.
Your article is protected by copyright and all rights are held exclusively by Springer Science +Business Media New York. This e-offprint is for personal use only and shall not be self-archived in electronic repositories. If you wish to self-archive your article, please use the accepted manuscript version for posting on your own website. You may further deposit the accepted manuscript version in any repository, provided it is only made publicly available 12 months after official publication or later and provided acknowledgement is given to the original source of publication and a link is inserted to the published article on Springer's website. The link must be accompanied by the following text: “The final publication is available at link.springer.com”.
Contributor Information
Erick G. Guerrero, School of Social Work, University of Southern California, Los Angeles, CA, USA
Kevin C. Heslin, Veterans Emergency Management Evaluation Center, Veterans Health Administration, North Hills, CA, USA
Evelyn Chang, Center for the Study of Healthcare Innovation, Implementation and Policy, Veterans Health Administration, North Hills, CA, USA.
Karissa Fenwick, School of Social Work, University of Southern California, Los Angeles, CA, USA.
Elizabeth Yano, Center for the Study of Healthcare Innovation, Implementation and Policy, Veterans Health Administration, North Hills, CA, USA.
References
- Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Administration and Policy in Mental Health and Mental Health Services Research. 2011a;38:4–23. doi: 10.1007/s10488-010-0327-7. doi:10.1007/s10488-010-0327-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aarons GA, Sommerfeld DH, Willging CE. The soft underbelly of system change: The role of leadership and organizational climate in turnover during statewide behavioral health reform. Psychological Services. 2011b;8:269–281. doi: 10.1037/a002619. doi:10.1037/a0026196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality The academy: Integrating behavioral health and primary care. 2013 Retrieved from http://integrationacademy.ahrq.gov/
- Baer M, Frese M. Innovation is not enough: Climates for initiative and psychological safety, process innovations, and firm performance. Journal of Organizational Behavior. 2003;24:45–68. doi:10.1002/job.179. [Google Scholar]
- Benzer JK, Beehler S, Miller C, Burgess JF, Sullivan JL, Mohr DC, et al. Grounded theory of barriers and facilitators to mandated implementation of mental health care in the primary care setting. Depression Research and Treatment. 2012;2012:597157. doi: 10.1155/2012/597157. doi:10.1155/2012/597157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Box TL, McDonell M, Helfrich CD, Jesse RL, Fihn SD, Rumsfeld JS. Strategies from a nationwide health information technology implementation: The VA CART story. Journal of General Internal Medicine. 2010;25(1, Suppl):72–76. doi: 10.1007/s11606-009-1130-6. doi:10.1007/s11606-009-1130-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler M, Kane RL, McAlpine D, Kathol RG, Fu SS, Hagedorn H, et al. Integration of mental health/ substance abuse and primary care (AHRQ Publication No. 09-E003) Agency for Healthcare Research and Quality; Rockville: 2008. [Google Scholar]
- Chalk M, Dilonardo J, Rinaldo SG, Oehlmann P. Integrating appropriate services for substance use conditions in health care settings: An issue brief on lessons learned and challenges ahead. Treatment Research Institute; Philadelphia: 2010. [Google Scholar]
- Chang ET, Rose DE, Yano EM, Wells KB, Metzger ME, Post EP, et al. Determinants of readiness for primary care-mental health integration (PC-MHI) in the VA health care system. Journal of General Internal Medicine. 2013;28:353–362. doi: 10.1007/s11606-012-2217-z. doi:10.1007/s11606-012-2217-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiverton P, Lindley P, Tortoretti DM, Plum KC. Well balanced: 8 steps to wellness for adults with mental illness and diabetes. Journal of Psychosocial Nursing and Mental Health Services. 2007;45(11):46–55. doi: 10.3928/02793695-20071101-08. [DOI] [PubMed] [Google Scholar]
- Donahue KE, Halladay JR, Wise A, Reiter K, Lee S-YD, Ward K, et al. Facilitators of transforming primary care: A look under the hood at practice leadership. Annals of Family Medicine. 2013;11:S27–S33. doi: 10.1370/afm.1492. doi:10.1370/afm.1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dundon M, Dollar K, Schohn M, Latinga LJ. Primary care-mental health integration: Co-located, collaborative care: An operations manual. Center for Integrated Healthcare; Syracuse: 2011. [Google Scholar]
- Edmondson AC, Golden BR, Young GJ. Turnaround at the Veterans Health Administration. Harvard Business School; Boston: 2008. [Google Scholar]
- Ell K, Unützer J, Aranda M, Gibbs NE, Lee P-J, Xie B. Managing depression in home health care: A randomized clinical trial. Home Health Care Services Quarterly. 2007;26(3):81–104. doi: 10.1300/J027v26n03_05. doi:10.1300/J027v26n03_05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer MM, Rose DE, Riopelle D, Lanto AB, Yano EM. Gender differences in smoking and smoking cessation treatment: An examination of the organizational features related to care. Women's Health Issues. 2011;21:S182–S189. doi: 10.1016/j.whi.2011.04.018. doi:10.1016/j.whi.2011.04.018. [DOI] [PubMed] [Google Scholar]
- Fickel JJ, Yano EM, Parker LE, Rubenstein LV. Clinic-level process of care for depression in primary care settings. Administration and Policy in Mental Health and Mental Health Services Research. 2009;36:144–158. doi: 10.1007/s10488-009-0207-1. doi:10.1007/s10488-009-0207-1. [DOI] [PubMed] [Google Scholar]
- Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: A cumulative meta-analysis and review of longer-term outcomes. Archives of Internal Medicine. 2006;166:2314–2321. doi: 10.1001/archinte.166.21.2314. doi:10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- Glisson C, Dukes D, Green P. The effects of the ARC organizational intervention on caseworker turnover, climate, and culture in children's service systems. Child Abuse and Neglect. 2006;30:855–880. doi: 10.1016/j.chiabu.2005.12.010. doi:10.1016/j.chiabu.2005.12.010. [DOI] [PubMed] [Google Scholar]
- Glisson C, James LR. The cross-level effects of culture and climate in human service teams. Journal of Organizational Behavior. 2002;23:767–794. doi:10.1002/job.162. [Google Scholar]
- Gordon AJ, Kavanagh G, Krumm M, Ramgopal R, Paidisetty S, Aghevli M, et al. Facilitators and barriers in implementing buprenorphine in the Veterans Health Administration. Psychology of Addictive Behaviors. 2011;25:215–224. doi: 10.1037/a0022776. doi:10.1037/a0022776. [DOI] [PubMed] [Google Scholar]
- Guerrero EG, Kim A. Organizational structure, leadership and readiness for change and the implementation of organizational cultural competence in addiction health services. Evaluation and Program Planning. 2013;40:74–81. doi: 10.1016/j.evalprogplan.2013.05.002. doi:10.1016/j.evalprogplan.2013.05.002. [DOI] [PubMed] [Google Scholar]
- Hankin CS, Spiro A, I. I. I., Mansell D, Miller DR, Kazis LE. Mental disorders and medical care utilization of VA ambulatory care patients: The Veterans Health Study. Journal of Ambulatory Care Management. 2006;29:51–60. doi: 10.1097/00004479-200601000-00006. doi:10.1097/00004479-200601000-00006. [DOI] [PubMed] [Google Scholar]
- Hedrick SC, Chaney EF, Felker B, Liu C-F, Hasenberg N, Heagerty P, et al. Effectiveness of collaborative care depression treatment in Veterans’ Affairs primary care. Journal of General Internal Medicine. 2003;18:9–16. doi: 10.1046/j.1525-1497.2003.11109.x. doi:10.1046/j.1525-1497.2003.11109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs health care system on the quality of care. New England Journal of Medicine. 2003;348:2218–2227. doi: 10.1056/NEJMsa021899. doi:10.1056/NEJMsa021899. [DOI] [PubMed] [Google Scholar]
- Kirchner J, Edlund CN, Henderson K, Daily L, Parker LE, Fortney JC. Using a multi-level approach to implement a primary care mental health (PCMH) program. Families, Systems, & Health. 2010;28:161–174. doi: 10.1037/a0020250. doi:10.1037/a0020250. [DOI] [PubMed] [Google Scholar]
- Kizer KW, Fonseca ML, Long LM. The veterans healthcare system: Preparing for the twenty-first century. Hospital & Health Services Administration. 1997;42:283–298. [PubMed] [Google Scholar]
- Lehman WEK, Greener JM, Simpson DD. Assessing organizational readiness for change. Journal of Substance Abuse Treatment. 2002;22:197–209. doi: 10.1016/s0740-5472(02)00233-7. doi:10.1016/S0740-5472(02)00233-7. [DOI] [PubMed] [Google Scholar]
- Marsden PV, Landon BE, Wilson IB, McInnes K, Hirschhorn LR, Ding L, et al. The reliability of survey assessments of characteristics of medical clinics. Health Services Research. 2006;41:265–283. doi: 10.1111/j.1475-6773.2005.00480.x. doi:10.1111/j.1475-6773.2005.00480.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendel P, Meredith LS, Schoenbaum M, Sherbourne CD, Wells KB. Interventions in organizational and community context: A framework for building evidence on dissemination and implementation in health services research. Administration and Policy in Mental Health and Mental Health Services Research. 2008;35:21–37. doi: 10.1007/s10488-007-0144-9. doi:10.1007/s10488-007-0144-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Benzer JK, Young GJ. Provider workload and quality of care in primary care settings: Moderating role of relational climate. Medical Care. 2013;51:108–114. doi: 10.1097/MLR.0b013e318277f1cb. doi:10.1097/ MLR.0b013e318277f1cb. [DOI] [PubMed] [Google Scholar]
- National Council for Behavioral Health Reclaiming the new frontier: Annual report: June 2012–May 2013. 2013 Retrieved from http://www.thenationalcouncil.org/about/annual-report/
- Oliver A. The Veterans Health Administration: An American success story? Milbank Quarterly. 2007;85:5–35. doi: 10.1111/j.1468-0009.2007.00475.x. doi:10.1111/j.1468-0009.2007.00475.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pomerantz AS, Sayers SL. Primary care-mental health integration in healthcare in the Department of Veterans Affairs. Families, Systems, & Health. 2010;28:78–82. doi: 10.1037/a0020341. doi:10.1037/a0020341. [DOI] [PubMed] [Google Scholar]
- Post EP, Metzger M, Dumas P, Lehmann L. Integrating mental health into primary care within the Veterans Health Administration. Families, Systems, & Health. 2010;28:83–90. doi: 10.1037/a0020130. doi:10.1037/a0020130. [DOI] [PubMed] [Google Scholar]
- Rosenberg RN. Translating biomedical research to the bedside: A national crisis and a call to action. Journal of the American Medical Association. 2003;289:1305–1306. doi: 10.1001/jama.289.10.1305. doi:10.1001/jama.289.10.1305. [DOI] [PubMed] [Google Scholar]
- Rubin RR, Peyrot M, Saudek CD. The effect of a diabetes education program incorporating coping skills training on emotional well-being and diabetes self-efficacy. Diabetes Educator. 1993;19:210–214. doi:10.1177/014572179301900308. [Google Scholar]
- Scholle SH, Pawlson LG, Solberg LI, Shih SC, Asche SE, Chou AF, et al. Measuring practice systems for chronic illness care: Accuracy of self-reports from clinical personnel. Joint Commission Journal on Quality and Patient Safety. 2008;34:407–416. doi: 10.1016/s1553-7250(08)34051-3. [DOI] [PubMed] [Google Scholar]
- Sung NS, Crowley WF, Jr, Genel M, Salber P, Sandy L, Sherwood LM, et al. Central challenges facing the national clinical research enterprise. Journal of the American Medical Association. 2003;289:1278–1287. doi: 10.1001/jama.289.10.1278. doi:10.1001/jama.289.10.1278. [DOI] [PubMed] [Google Scholar]
- Veterans Health Administration . Uniform mental health services in VA medical centers and clinics. Department of Veterans Affairs; Washington: 2008. [Google Scholar]
- Weisner C, Mertens J, Parthasarathy S, Moore C, Lu Y. Integrating primary medical care with addiction treatment: A randomized controlled trial. Journal of the American Medical Association. 2001;286:1715–1723. doi: 10.1001/jama.286.14.1715. doi:10.1001/jama.286.14.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray LO, Szymanski BR, Kearney LK, McCarthy JF. Implementation of primary care-mental health integration services in the Veterans Health Administration: Program activity and associations with engagement in specialty mental health services. Journal of Clinical Psychology in Medical Settings. 2012;19:105–116. doi: 10.1007/s10880-011-9285-9. doi:10.1007/s10880-011-9285-9. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs Putting clinical practice guidelines to work in VHA. 2012 Retrieved from http://www.healthquality.va.gov/VA_Manual.pdf.
- Yano EM, Fleming B, Canelo I, Lanto AB, Yee T, Wang M, et al. VHA clinical practice organizational survey: National survey results for the VA primary care director module. Sepulveda: 2008. VA HSR&D Center for the Study of Healthcare Provider Behavior. [Google Scholar]
- Young GJ. Managing organizational transformations: The case of the Veterans Health Administration. California Management Review. 2000;43:66–82. [Google Scholar]
- Yukl G. Effective leadership behavior: What we know and what questions need more attention. Academy of Management Perspectives. 2012;26(4):66–85. doi:10.5465/amp.2012.0088. [Google Scholar]
- Zapka JG, White MJ, Reed G, Ockene JK, List E, Pbert L, et al. Organizational systems to support publicly funded tobacco treatment services. American Journal of Preventive Medicine. 2005;28:338–345. doi: 10.1016/j.amepre.2005.01.008. doi:10.1016/j.amepre.2005.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zivin K, Pfeiffer PN, Szymanski BR, Valenstein M, Post EP, Miller EM, et al. Initiation of primary care–mental health integration programs in the VA health system: Associations with psychiatric diagnoses in primary care. Medical Care. 2010;48:843–851. doi: 10.1097/MLR.0b013e3181e5792b. doi:10.1097/MLR.0b013e3181e5792b. [DOI] [PubMed] [Google Scholar]