Abstract
Aims
This randomized controlled trial (RCT) evaluated whether a process with single combined testing of copeptin and troponin at admission in patients with low-to-intermediate risk and suspected acute coronary syndrome (ACS) does not lead to a higher proportion of major adverse cardiac events (MACE) than the current standard process (non-inferiority design).
Methods and results
A total of 902 patients were randomly assigned to either standard care or the copeptin group where patients with negative troponin and copeptin values at admission were eligible for discharge after final clinical assessment. The proportion of MACE (death, survived sudden cardiac death, acute myocardial infarction (AMI), re-hospitalization for ACS, acute unplanned percutaneous coronary intervention, coronary artery bypass grafting, or documented life threatening arrhythmias) was assessed after 30 days. Intention to treat analysis showed a MACE proportion of 5.17% [95% confidence intervals (CI) 3.30–7.65%; 23/445] in the standard group and 5.19% (95% CI 3.32–7.69%; 23/443) in the copeptin group. In the per protocol analysis, the MACE proportion was 5.34% (95% CI 3.38–7.97%) in the standard group, and 3.01% (95% CI 1.51–5.33%) in the copeptin group. These results were also corroborated by sensitivity analyses. In the copeptin group, discharged copeptin negative patients had an event rate of 0.6% (2/362).
Conclusion
After clinical work-up and single combined testing of troponin and copeptin to rule-out AMI, early discharge of low- to intermediate risk patients with suspected ACS seems to be safe and has the potential to shorten length of stay in the ED. However, our results need to be confirmed in larger clinical trials or registries, before a clinical directive can be propagated.
Keywords: Copeptin, Acute coronary syndrome (ACS), Rule-out, Acute myocardial infarction (AMI), Randomized controlled trial (RCT)
See page 333 for the editorial comment on this article (doi:10.1093/eurheartj/ehu211)
Introduction
Rule-out of acute myocardial infarction (AMI) is a major challenge in Emergency Medicine. Around 10% of all internal medicine emergency patients present to the Emergency Department (ED) with chest pain, but only ∼10% of these patients have an AMI as the underlying disease.1 Due to the potential hazards of overseeing an evolving MI, most patients are subjected to 6–12 h observation on chest pain units (CPU) with the effect of an excellent prognosis at high costs.2,3
Copeptin (CT-pro-vasopressin) is a marker of acute (haemodynamic) stress4 and is elevated immediately at presentation of patients with AMI.5 A series of observational studies have shown that due to complementary pathophysiology and kinetics, copeptin in combination with conventional and high sensitivity (hs) cardiac troponin (cTn) is an excellent rule-out marker for AMI5–11 with a high negative predictive value (NPV) of up to 99%. Some studies were not able to reproduce this high NPV12,13 or to show an added value when copeptin was combined with hsTn.14,15 These results could partially be influenced by late copeptin testing,12 which impacts the ability to detect an early copeptin rise, by late patient presentation or by the selection of patient cohorts including high-risk patients. These factors would lead to a higher prevalence of positive hsTn test results at presentation, thus increasing the NPV for hsTn alone. Additionally, most studies used a copeptin assay which did not allow choosing a cut-off below 14 pmol/L.
So far, it has not been prospectively tested whether patients with negative copeptin and troponin test results can safely be discharged to outpatient care. The instant rule-out of AMI has a potentially high impact on future clinical practice, but safety of this strategy has to be assured.
We conducted a randomized controlled trial (RCT) to assess the safety of an early discharge after rule-out of AMI with a single combined testing of troponin and copeptin at presentation to the ED/CPU when compared with the current standard process with serial troponin measurements in low-to-intermediate risk patients with suspected acute coronary syndrome (ACS). The primary endpoint was the proportion of major adverse cardiac events (MACE) at 30 days, including events during the index stay. Given that the current process of evaluating patients with ACS is regarded as very safe, a non-inferiority design was chosen to test the hypothesis.
Methods
Participants
This is a multi-centre, interventional clinical process RCT. The methods are reported in full in the protocol (notfallmedizin.charite.de/forschung_lehre/nord_campi/forschung/biomarkers_in_cardiology/). Participants were recruited in the EDs and/or CPUs in five German, one Swiss, and one Austrian site from April 2011 until May 2013. Patients were eligible if they were aged ≥18 years, presented with signs and symptoms of ACS, and had a negative troponin value at presentation. Patients were excluded if they were diagnosed with ST-elevation myocardial infarction (STEMI), if hospital admission was indicated due to high risk as defined in current guidelines (continuing chest pain or recurrent episodes of chest pain under therapy, GRACE score above 140), and if hospital admission was necessary for any other reasons.
The study complies with the Declaration of Helsinki and received ethics approvals from all study sites' ethics committees. All patients provided written informed consent. The study is registered at the German Clinical Trials Register (DRKS00000276), the International Clinical Trials Registration platform of the WHO (UTN U1111-1118-1665), and at ClinicalTrials.gov (NCT0149873).
Procedures
Patients were enrolled by the treating physician and randomized using 1:1 computer-generated block randomization stratified by centre (DatInf® RandList, DatInf GmbH, Tübingen). Copeptin was measured from the same initial blood draw as the first troponin value after written informed consent and randomization.
In the standard group, patients were managed according to the current guidelines for the management of patients with suspected ACS. The copeptin values were measured but not revealed to the treating staff to assure standard care.
In the copeptin group, further patient management was dependent on the copeptin result. In case of a negative result, patients were considered low risk and could be discharged into ambulant care. Before discharge, patients had a final visit to secure their well-being. The final discharge decision was at the discretion of the attending physician who was allowed to overrule the biomarker result. All discharged patients had an outpatient cardiology appointment within a maximum of 3 days after discharge. In case of a positive copeptin result, patients were managed like the standard group.
All patients were contacted at 30 days to assess their outcome (Supplementary material online, Figure S1).
Outcome
Primary endpoint was the proportion of combined MACE, defined as all-cause death or survived sudden cardiac death, AMI, re-hospitalization for ACS, acute unplanned percutaneous coronary intervention (PCI), coronary artery bypass grafting (CABG), and documented life-threatening arrhythmias (ventricular tachycardia, ventricular fibrillation, atrio-ventricular-block III) within 30 days, including events during the index hospital stay.
Acute myocardial infarction was defined as per Universal Definition.16 Every patient was assigned only one MACE with priority of the event that occurred first.
Secondary endpoints were proportion of coronary angiography (CA), split MACE at 30 and all MACE at 90 days, major bleeding events (as per TIMI definition), and length of stay (LOS).
All MACE and bleeding events were adjudicated by two independent Cardiologists blinded to copeptin result and group assignment.
Biomarker testing
Copeptin was measured from the routine blood sample at admission, using the Thermo Scientific B·R·A·H·M·S Copeptin ultrasensitive Kryptor assay. The assay has a detection limit of 0.9 pmol/L and a functional assay sensitivity of <2 pmol/L. A value of 10 pmol/L and above was considered positive. The cut-off was chosen with reference to Keller et al.5 who determined different cut-offs in a reference population and tested the diagnostic performance of these cut-offs in an ACS population.
Troponin was tested as by routine practice at the individual sites. A conventional troponin T (TnT) POCT assay (AQT 90 -Radiometer) was used at two sites (cut-off >30 ng/L).
High-sensitive TnT (Roche) was used at four sites for all and at two sites for further serial troponin measurements (cut-off >14 ng/L). One site used troponin I (Siemens Dimension®-System) (cut-off level 56 ng/L) until November 2012 and troponin I (Siemens Dimension Vista®-System) thereafter (cut-off level 45 ng/L).
Additional blood samples were drawn as per standard practice after 3–6 h.
Statistical analysis
All data were entered into an online electronic case report form. Statistical analyses were performed using the software packages SPSS (IBM® SPSS Statistics, Version 21) and SAS Version 9.3 (SAS® Institute Inc.).
Statistical testing of categorical variables was performed using exact binomial tests; for numerical variables, t-tests (in case of normal distribution) or Wilcoxon tests (no normal distribution) were used. For the comparison between more than two groups, Kruskall–Wallis test was used. A P-value below 0.05 was considered significant.
The study hypothesis was non-inferiority of the copeptin process against the standard process regarding the primary endpoint. The power calculation was based on an anticipated proportion of MACE within 30 days of 10%.17–19 Confidence intervals (CI) for differences were calculated as one-sided 97.5% CI using the Wilson procedure with a correction for continuity.20 The non-inferiority margin was set at 5%. Note: This means, that non-inferiority of the new process can be accepted if the lower bound of the one-sided 97.5% CI of MACE difference between both study groups does not exceed the 5% margin. The rationale for this margin was based on own data, previous studies, and expert consensus. The sample size calculation resulted in a required number of 446 participants per group (892 overall) with a power of 80% and a level of significance of 5%.
In the intention to treat (ITT) analysis for the primary endpoint, all patients were analysed as randomized irrespective of protocol deviations, excluding all patients with an unknown outcome.
In the per protocol (PP) analysis, all patients with protocol deviations (n = 40), over-rulers (n = 71), as well as patients with unknown outcome (n = 14) were excluded. Additionally, sensitivity analyses, assuming that all patients who were lost to follow-up (FU) (n = 14) developed either a good (no MACE) or a poor (MACE) outcome, were conducted. Patients with protocol deviations were not excluded from this sensitivity analysis and were analysed as randomized. Confidence intervals for the primary endpoint were calculated as exact binomial 95% CIs.
Results
Patient characteristics
A total of 902 patients were randomized to either the standard (n = 451) or the copeptin (n = 451) group (Figure 1). Randomisation proved successful with very similar patient characteristics, risk profile, and medical history profile in the two groups (Table 1).
Figure 1.
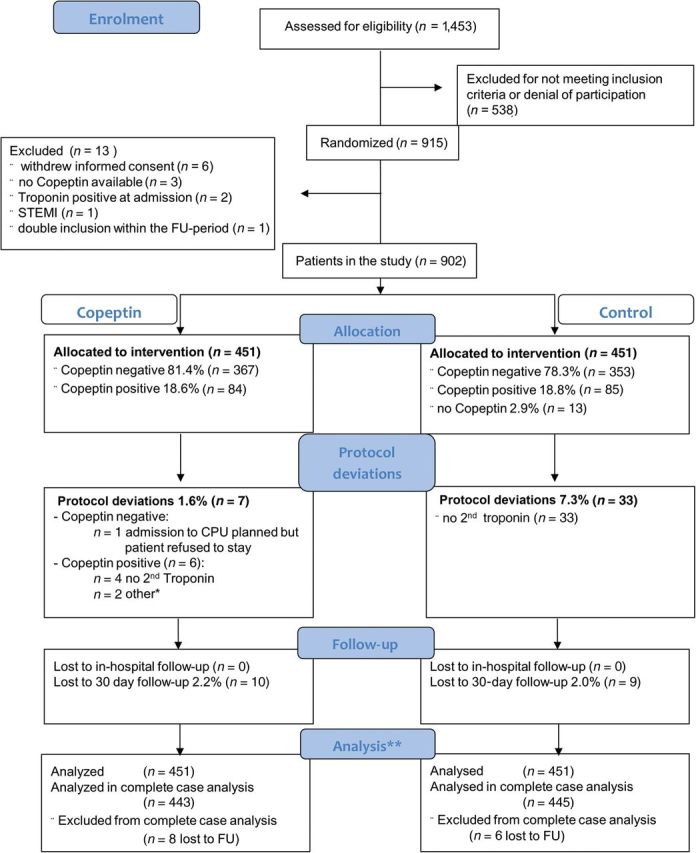
Consort flow diagram. A total of 13 patients were excluded from the study (6 patients withdrew, of 3 patients in the copeptin group, copeptin values were not available, 2 patients were troponin positive at admission, 1 patient had a ST-elevation myocardial infarction at admission, 1 patient had been randomized previously). In 72 copeptin-negative patients in the copeptin group, the treating physician decided that discharge was not possible, 71 of them were admitted to the chest pain units, 1 refused to be admitted. A total of 14 patients (1.6%) were lost to follow-up (FU) at 30 days and not considered in the complete case analysis, 8 in the copeptin and 6 in the standard group, the in-hospital FU was available for all patients. *n = 1 randomized 12 h after admission; n = 1 suspected aortic dissection at admission; **n = 5 patients were lost to 30d-FU but included in the complete case analysis (ITT). Of those n = 4 had an in-hospital major cardiac events (MACE), one patient did not have an initial event but his death date was identified in the German central registry.
Table 1.
Characteristics of all patients and in the study groups
| All patients (n = 902) | Standard group (n = 451) | Copeptin group (n = 451) | |
|---|---|---|---|
| Patient characteristics | |||
| Age (years) (mean ± SD) | 54.1 ± 15.6 | 54.1 ± 15.1 | 54.1 ± 16.2 |
| Male sex | 63.2 (570) | 65.4 (295) | 61.0 (275) |
| Risk factors | |||
| BMI | 27.3 ± 4.86 | 27.3 ± 4.64 | 27.3 ± 5.1 |
| Diabetes | 13.6 (123) | 14.0 (63) | 13.3 (60) |
| Hypertension | 57.5 (519) | 57.0 (257) | 58.1 (262) |
| Hyperlipidaemia | 43.5 (392) | 45.2 (204) | 41.7 (188) |
| Family history of MI | 25.5 (230) | 22.2 (100) | 28.8 (130) |
| Smoker | 32.4 (292) | 33.7 (152) | 31.0 (140) |
| Ex-smoker | 30.8 (278) | 30.2 (136) | 31.5 (142) |
| GRACE-score (mean ± SD) | 80.32 ± 27.6 | 79.8 ± 27.6 | 80.9 ± 27.5 |
| TIMI risk score (Median/IQR) | 1 (0–3) | 1 (0–2) | 1 (0–3) |
| Medical history | |||
| Known CAD | 25.7 (232) | 24.6 (111) | 26.8 (121) |
| Prior MI | 14.6 (132) | 15.3 (69) | 14.0 (63) |
| Prior PCI | 22.2 (200) | 22.1 (100) | 22.2 100) |
| Prior CABG | 5.0 (45) | 3.5 (16) | 6.4 (29) |
| Chronic heart failure | 5.8 (52) | 4.2 (19) | 7.3 (33) |
| Primary valve disease | 6.9 (62) | 7.1 (32) | 6.7 (30) |
| Prior valve surgery | 1.2 (11) | 0.9 (4) | 1.6 (7) |
| Cardiomyopathy | 2.1 (19) | 1.1 (5) | 3.1 (14) |
| Renal disease | 6.2 (56) | 4.9 (22) | 7.5 (34) |
| Time since symptom onset | |||
| 0–3 h | 43.2 (345) | 43.8 (178) | 42.6 (167) |
| <6 h | 54.8 (437) | 54.4 (221) | 55.1 (216) |
| <12 h | 64.0 (511) | 62.3 (253) | 65.8 (258) |
| Missing data | n = 104 | n = 45 | n = 59 |
Patient characteristics at admission of all patients and in the study groups as randomized. Data are shown as percent (numbers) or as stated. Abbreviations: SD, standard deviation; IQR, inter quartile ranges; BMI, body mass index.
Outcome
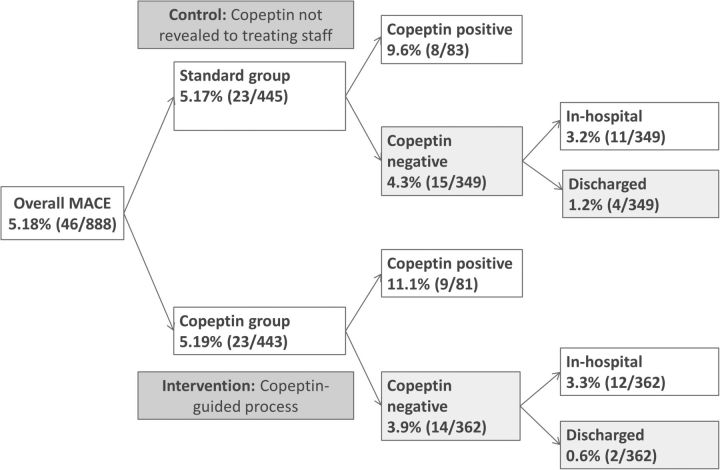
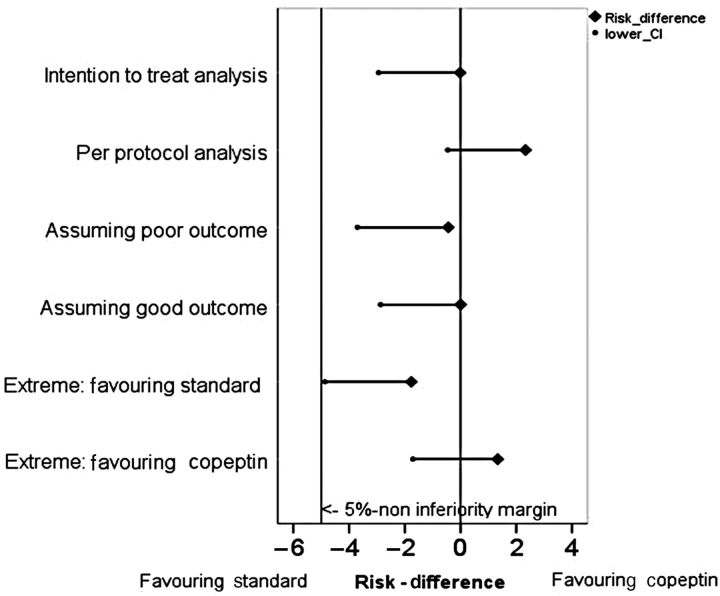
A total of 46 of all patients developed a MACE during the 30-day FU period. The absolute number of patients with MACE was equal between the two groups (n = 23 for both; Table 2, Figure 2). Intention to treat analysis showed a MACE proportion of 5.17% (95% CI 3.30–7.65%) in the standard group and 5.19% (95% CI 3.32–7.69%) in the copeptin group (Table 2). In the PP analysis, the MACE proportion was 5.34% (95% CI 3.38–7.97%) in the standard group, and 3.01% (95% CI 1.51–5.33%) in the copeptin group. In all four sensitivity analyses, including extreme case analyses, the non-inferiority margin was not exceeded by the one-sided 97.5% CI (Figure 3).
Table 2.
Primary endpoint analyses
| Standard group (n = 451) | Copeptin group (n = 451) | Absolute difference in MACE proportion (97.5% one-sided CI) | |
|---|---|---|---|
| MACE at 30 days | |||
| Yes | 23 | 23 | – |
| No | 422 | 422 | – |
| Unknown | 6 | 8 | – |
| MACE % (95% CI): (absolute numbers) | |||
| Intention to treat analysis | 5.17 (3.30–7.65) (23/445) | 5.19 (3.32–7.69) (23/443) | −0.02 (−2.94) |
| Per protocol analysis | 5.34 (3.38–7.97) (22/412) | 3.01 (1.51–5.33) (11/365) | 2.33 (−0.46) |
| Sensitivity analyses | |||
| Assuming poor outcome | 6.43 (4.35–9.10) (29/451) | 6.87 (4.72–9.61) (31/451) | −0.44 (−3.70) |
| Assuming good outcome | 5.10 (3.26–7.55) (23/451) | 5.10 (3.26–7.55) (23/451) | 0.00 (−2.87) |
| Extreme case: favouring standard group | 5.10 (3.26–7.55) (23/451) | 6.87 (4.72–9.61) (31/451) | −1.77 (−4.87) |
| Extreme case: favouring copeptin group | 6.43 (4.35–9.10) (29/451) | 5.10 (3.26–7.55) (23/451) | 1.33 (−1.71) |
Analysis of the primary endpoint: All MACE within 30 days.
The CIs for the absolute difference between the proportions in the respective study groups did not exceed the 5% non-inferiority margin in any analysis, confirming non-inferiority of the copeptin based process as hypothesized, even if the worst case was assumed.
Figure 2.
Major adverse cardiac events (MACE) proportions in study groups and in copeptin subgroups. Patients were randomized into copeptin and standard group, where MACE proportions were very similar. Copeptin results were only revealed to the treating staff in the copeptin group. In subgroups of copeptin-positive and copeptin-negative patients, major adverse cardiac event (MACE) rates are higher in copeptin positives. MACE proportions are lowest in discharged copeptin-negative patients.
Figure 3.
Forest plot for differences in major adverse cardiac event (MACE) proportions. Absolute differences in MACE proportions within 30 days between the study groups with one-sided 97.5% CIs. The non-inferiority margin was prospectively defined at 5%. In none of the performed analyses, the non-inferiority margin was exceeded.
More information on the outcome data of the compound endpoint is shown in Supplementary material online, Table S1 and Supplementary material online, Figure S2. No MIs or deaths occurred in the discharged copeptin-negative patients of the copeptin group. Detailed information on copeptin-negative patients with MACE is shown in the Supplementary material online, Table S3. Diagnoses, in-hospital course, in-hospital procedures, and length of hospital stay are shown in Supplementary material online, Table S2. Of all patients, 39.8% (359/902) were discharged from the ED. In the copeptin group, 67.6% (305/451) were discharged from the ED as opposed to 12.0% (54/451) in the standard group (P<0.001; Table 3).
Table 3.
Secondary endpoints
| All patients n = (902) | Standard group (n = 451) | Copeptin group (n = 451) | P-value | |
|---|---|---|---|---|
| In-hospital course | ||||
| Discharge from ED | 39.8 (359) | 12.0 (54) | 67.6 (305) | <0.001 |
| Index in-hospital procedures | ||||
| CA | 10.6 (96) | 9.1 (41) | 12.2 (55) | 0.132 |
| PCI | 4.6 (41) | 3.3 (15) | 5.8 (26) | 0.080 |
| PCI/CA ratio (%) | 42.7 | 36.6 | 47.3 | 0.307 |
| CABG | 0.2 (2) | – | 0.4 (2) | – |
| LOS in % (n) | ||||
| 0–1 day | 85.1 (767) | 84.9 (383) | 85.1 (384) | 1.000 |
| 2–5 days | 11.3 (102) | 12.4 (56) | 10.2 (46) | 0.344 |
| >6 days | 3.7 (33) | 2.7 (12) | 4.7 (21) | 0.155 |
| LOS in hours (median/IQR) | ||||
| LOS for all patients | 6 (4–11) | 7 (5–13) | 4 (3–8) | <0.001 |
| LOS in 0–1-day groupa | 5 (4–8) | 7 (4–9) | 4 (2–6) | <0.001 |
| Major bleedings in % (n) | 0.4 (4) | 0.2 (1) | 0.7 (3) | 0.573 |
Secondary endpoints in all patients and in the respective study groups.
aThe LOS for patients discharged after MI exclusion was analysed in all patients who were discharged the same day, or the day after presentation to the ED in order to include patients who were admitted to the CPU for ACS evaluation.
Of the copeptin-negative patients in the copeptin group, 80.7% (296/367) were discharged from the ED, as opposed to 11.6% (41/353) of copeptin negative patients in the standard group (P < 0.001; Supplementary material online, Table S2). The LOS for patients discharged after MI exclusion was analysed in all patients who were discharged the same day, or the day after presentation to the ED in order to also include patients who were admitted to the CPU for ACS evaluation. Median LOS was significantly shorter in the copeptin group (4 (IQR 2–6) h) than in the standard group (7 (IQR 4–9) h, P < 0.001).
The PCI/CA ratio was higher in the copeptin group (47.3%) when compared with the standard group (36.6%), without reaching statistical significance (P = 0.307; Table 3).
Discussion
The current study provides evidence that with appropriate clinical selection of low-to-intermediate risk patients with suspected ACS, the combination of negative troponin and negative copeptin at presentation on the basis of a thorough clinical evaluation helps identify patients who can safely be discharged into outpatient care. The MACE proportion at 30 days did not differ between the two groups confirming non-inferiority of the new process. Secondary endpoint analysis shows that the new process is effective with a reduced length of hospital stay and a higher proportion of discharges directly from the ED.
Standard process and promises of high sensitivity cardiac troponin
The standard clinical process for the acute diagnostic assessment of suspected ACS is described in current guidelines.21 These guidelines focus on troponin measured with hs assays and on delta changes, as a number of observational studies have shown that the new assay generation might enable rule-in and rule-out of AMI earlier than conventional assays.22–24 The exact definition of relevant troponin changes is an important and yet unsolved issue. Recent publications show conflicting delta values25,26 and, additionally, minor delta changes may also occur in patients with AMI.27 Additionally, hs assays identify a high number of patients with elevated troponin results without AMI, making interpretation of test results challenging. There are no interventional studies, which prospectively tested whether fast rule-out strategies with serial hsTn alone are effective and safe.
The new process
The current process of evaluating patients with suspected ACS is regarded as safe.21 Any new process has got to prove that patient safety is not decreased by applying the new process and that it holds advantages beyond safety.
The biomarker strategy of a combined copeptin-troponin rule-out of AMI has been analysed in a number of retrospective observational biomarker studies,5,7,8 but this is the first interventional RCT evaluating the safety of early discharge. Clinicians may use the new strategy for a fast track which reserves space and resources for more severely ill patients. In addition, unnecessary treatment with anti-platelet and anti-thrombotic medications can be avoided, reducing the risk of bleeding complications. The shorter LOS potentially reduces risks of hospitalization, stress, and anxiety.
Safety issues of the new process
Previous copeptin studies have faced criticism because the NPV is not 100% and some people may argue that it is not safe to implement a strategy which seems to ‘fail’ in some patients. The combined endpoint in our study was mainly driven by PCIs performed during the index hospital stay, whereas severe events like AMI and death were rare and occurred in-hospital only. Most probably, those PCIs were not triggered only by ‘urgency’ but also by ‘occasion’.
The component ‘urgent PCI’ was added to the combined endpoint as we did not want to oversee PCIs after discharge which may have prevented MIs or deaths and therefore could have masked risks in the discharged group. The event rate in copeptin-negative patients discharged was in fact very low (0.6%). Life-threatening events were not detected in copeptin-negative patients.
In our study, 81.4% of patients in the copeptin group were copeptin and troponin negative. In 71 cases, the treating physician decided to overrule the negative marker result and to admit the patient to the CPU. This is an acceptable rate of overruling as the clinical responsibility needs to be in the hands of the attending physician and a ‘traditional’ and known process is usually favoured. Of the 14 copeptin-negative patients with MACE, 12 were not discharged despite their negative biomarker result. Of these, two patients were diagnosed with an NSTEMI during the initial hospital stay, but did not profit from a coronary intervention. The two copeptin-negative patients with MACE who were discharged had (i) an unplanned PCI and (ii) CABG surgery in the 30-day FU period. This is not surprising as copeptin is not a marker of coronary artery disease and the initial discharge was safe for both patients. Nevertheless, it should be highlighted that the patients in this study were scheduled for a cardiology outpatient visit within three working days and therefore a diagnostic workup was facilitated.
Limitations
A rapid rule-out of AMI with the combined biomarker testing from a single blood draw at admission is bound to cause concerns in some physicians who are used to 20 years of serial biomarker (troponin) measurements. Our study was performed in the EDs under routine conditions and by the routine ED physicians. Considering this, the number of cross-overs in our study (n = 71) should be judged as low; the majority of copeptin-negative patients were discharged early. It needs to be emphasized that any biomarker strategy must be embedded in a process of thorough physician work-up and clinical judgement.
A total number of 19 patients (2.1%, Figure 1) were lost to FU, which is an acceptable rate but may still have influenced the results of the trial. Notably, even the worst-case scenario sensitivity analysis, assuming a negative outcome for all patients lost to FU in the copeptin group, did not change the primary result of our study.
Due to the high number of cross-overs in the copeptin-negative study group (n = 71), the results of the PP analysis, which suggests superiority of the copeptin-guided process, should be interpreted with caution.
The non-inferiority margin in this study (5%) was based on an anticipated event rate of 10%. This estimate was the result of a review of own data and historical studies.17–19 The actually observed event rate in our study, however, was 5.2% and was thus lower than expected. This lower event rate could be explained by the fact that the availability of cardiac catheterization laboratories has increased significantly during recent years and most hospitals use invasive diagnostic strategies in chest pain patients very liberally. Thus, it would be possible that a number of patients with intermediate risk (who would have been eligible to participate) were not included because discharge was not considered.28 The low observed event rate renders the non-inferiority margin relatively wide (relative to the event rate) and thus impacts the relevance of the statistical results which therefore need further confirmation by other clinical trials or registries before they can be regarded as clinically directive.
Conclusion
As for all new interventional strategies or therapies, it will be of major interest to evaluate the safety and effectiveness of this strategy under routine conditions and in a larger number of patients. The introduction of registries at sites who implement the new strategy will show whether the new concept is really safe or—as some fear—will be abused by busy ED physicians. The current study provides evidence that on the basis of a thorough clinical work-up and single combined testing of troponin and copeptin at presentation to rule-out AMI, early discharge of low-to-intermediate risk patients with suspected ACS seems to be safe, has the potential to shorten LOS in the ED, and may therefore benefit the patient. However, as a consequence of the relatively wide non-inferiority margin, our results need to be confirmed in larger clinical trials or registries, before a clinical directive can be propagated.
Supplementary material
Supplementary material is available at European Heart Journal online.
Funding
This work was supported by Thermo Scientific BRAHMS GmbH, but is an investigator initiated trial. Funding to pay the Open Access publication charges for this article was provided by BRAHMS GmbH.
Conflict of interest: With respect to this trial, M.M., J.S., A.S., and J.v.R. received research grants from ThermoScientific-BRAHMS GmbH; C.H. has received speaker honoraria and is member of the advisory board for ThermoScientific-BRAHMS GmbH; S.B. has received research funding, honoraria for lectures and consulting, and is as a member of Advisory Boards for ThermoScientific-BRAHMS GmbH; C.M. has received research support, speaker honoraria, and consultancy fees from ThermoScientific-BRAHMS GmbH; J.O.V. is employed at ThermoScientific-BRAHMS GmbH; E.G. has received honoraria for lectures and consultancy fees from ThermoScientific-BRAHMS GmbH; K.H., H.K., C.L., R.M., P.P., and M.T. have no conflict of interest to declare.
Supplementary Material
Acknowledgements
We thank Martin Stockburger and Malte Schröder for the MACE adjudication and Christian Müller (Berlin) for the manuscript review. We thank Sabine Hertel from Thermo Scientific BRAHMS GmbH for supporting the statistical analysis. We thank the staff at the respective study sites for their collaboration in this trial.
References
- 1.Mockel M, Searle J, Muller R, Slagman A, Storchmann H, Oestereich P, Wyrwich W, Ale-Abaei A, Vollert JO, Koch M, Somasundaram R. Chief complaints in medical emergencies: do they relate to underlying disease and outcome? The Charite Emergency Medicine Study (CHARITEM) Eur J Emerg Med. 2013;20:103–108. doi: 10.1097/MEJ.0b013e328351e609. [DOI] [PubMed] [Google Scholar]
- 2.Goodacre S, Nicholl J, Dixon S, Cross E, Angelini K, Arnold J, Revill S, Locker T, Capewell SJ, Quinney D, Campbell S, Morris F. Randomised controlled trial and economic evaluation of a chest pain observation unit compared with routine care. BMJ. 2004;328:254. doi: 10.1136/bmj.37956.664236.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pope JH, Aufderheide TP, Ruthazer R, Woolard RH, Feldman JA, Beshansky JR, Griffith JL, Selker HP. Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med. 2000;342:1163–1170. doi: 10.1056/NEJM200004203421603. [DOI] [PubMed] [Google Scholar]
- 4.Morgenthaler NG, Struck J, Alonso C, Bergmann A. Assay for the measurement of copeptin, a stable peptide derived from the precursor of vasopressin. Clin Chem. 2006;52:112–119. doi: 10.1373/clinchem.2005.060038. [DOI] [PubMed] [Google Scholar]
- 5.Keller T, Tzikas S, Zeller T, Czyz E, Lillpopp L, Ojeda FM, Roth A, Bickel C, Baldus S, Sinning CR, Wild PS, Lubos E, Peetz D, Kunde J, Hartmann O, Bergmann A, Post F, Lackner KJ, Genth-Zotz S, Nicaud V, Tiret L, Munzel TF, Blankenberg S. Copeptin improves early diagnosis of acute myocardial infarction. J Am Coll Cardiol. 2010;55:2096–2106. doi: 10.1016/j.jacc.2010.01.029. [DOI] [PubMed] [Google Scholar]
- 6.Gu YL, Voors AA, Zijlstra F, Hillege HL, Struck J, Masson S, Vago T, Anker SD, van den Heuvel AF, van Veldhuisen DJ, de Smet BJ. Comparison of the temporal release pattern of copeptin with conventional biomarkers in acute myocardial infarction. Clin Res Cardiol. 2011;100:1069–1076. doi: 10.1007/s00392-011-0343-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reichlin T, Hochholzer W, Stelzig C, Laule K, Freidank H, Morgenthaler NG, Bergmann A, Potocki M, Noveanu M, Breidthardt T, Christ A, Boldanova T, Merki R, Schaub N, Bingisser R, Christ M, Mueller C. Incremental value of copeptin for rapid rule out of acute myocardial infarction. J Am Coll Cardiol. 2009;54:60–68. doi: 10.1016/j.jacc.2009.01.076. [DOI] [PubMed] [Google Scholar]
- 8.Maisel A, Mueller C, Neath SX, Christenson RH, Morgenthaler NG, McCord J, Nowak RM, Vilke G, Daniels LB, Hollander JE, Apple FS, Cannon C, Nagurney JT, Schreiber D, deFilippi C, Hogan C, Diercks DB, Stein JC, Headden G, Limkakeng J, Anand I, Wu AHB, Papassotiriou J, Hartmann O, Ebmeyer S, Clopton P, Jaffe AS, Peacock WF. Copeptin helps in the early detection of patients with acute myocardial infarction: primary results of the CHOPIN Trial (Copeptin Helps in the early detection Of Patients with acute myocardial INfarction) J Am Coll Cardiol. 2013;62:150–160. doi: 10.1016/j.jacc.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 9.Mockel M. Copeptin adds to high-sensitivity troponin T in rapid rule out of acute myocardial infarction. Clin Chem. 2012;58:306–307. doi: 10.1373/clinchem.2011.171058. [DOI] [PubMed] [Google Scholar]
- 10.Ray P, Charpentier S, Chenevier-Gobeaux C, Reichlin T, Twerenbold R, Claessens YE, Jourdain P, Riou B, Mueller C. Combined copeptin and troponin to rule out myocardial infarction in patients with chest pain and a history of coronary artery disease. Am J Emerg Med. 2012;30:440–448. doi: 10.1016/j.ajem.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 11.Giannitsis E, Kehayova T, Vafaie M, Katus HA. Combined testing of high-sensitivity troponin T and copeptin on presentation at prespecified cutoffs improves rapid rule-out of non-ST-segment elevation myocardial infarction. Clin Chem. 2011;57:1452–1455. doi: 10.1373/clinchem.2010.161265. [DOI] [PubMed] [Google Scholar]
- 12.Karakas M, Januzzi JL, Jr., Meyer J, Lee H, Schlett CL, Truong QA, Rottbauer W, Bamberg F, Dasdemir S, Hoffmann U, Koenig W. Copeptin does not add diagnostic information to high-sensitivity troponin T in low- to intermediate-risk patients with acute chest pain: results from the rule out myocardial infarction by computed tomography (ROMICAT) study. Clin Chem. 2011;57:1137–1145. doi: 10.1373/clinchem.2010.160192. [DOI] [PubMed] [Google Scholar]
- 13.Llorens P, Sanchez M, Herrero P, Martin-Sanchez FJ, Pinera P, Miro O. The utility of copeptin in the emergency department for non-ST-elevation myocardial infarction rapid rule out: COPED-MIRRO study. Eur J Emerg Med. 2013 doi: 10.1097/MEJ.0b013e3283632f8b. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 14.Eggers KM, Venge P, Lindahl B. High-sensitive cardiac troponin T outperforms novel diagnostic biomarkers in patients with acute chest pain. Clin Chim Acta. 2012;413:1135–1140. doi: 10.1016/j.cca.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 15.Collinson P, Gaze D, Goodacre S. Comparison of contemporary troponin assays with the novel biomarkers, heart fatty acid binding protein and copeptin, for the early confirmation or exclusion of myocardial infarction in patients presenting to the emergency department with chest pain. Heart. 2014;100:140–145. doi: 10.1136/heartjnl-2013-304716. [DOI] [PubMed] [Google Scholar]
- 16.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Thygesen K The Writing Group on behalf of the Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction, Authors/Task Force Members Chairpersons. Third universal definition of myocardial infarction. Eur Heart J. 2012;33:2551–2567. [Google Scholar]
- 17.Manini AF, Gisondi MA, van der Vlugt TM, Schreiber DH. Adverse cardiac events in emergency department patients with chest pain six months after a negative inpatient evaluation for acute coronary syndrome. Acad Emerg Med. 2002;9:896–902. doi: 10.1111/j.1553-2712.2002.tb02190.x. [DOI] [PubMed] [Google Scholar]
- 18.Searle J, Shih J, Muller R, Vollert JO, Muller C, Danne O, Datwyler S, Mockel M. The role of myeloperoxidase (MPO) for prognostic evaluation in sensitive cardiac troponin I negative chest pain patients in the emergency department. Eur Heart J Acute Cardiovasc Care. 2013;2:203–210. doi: 10.1177/2048872613484688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mockel M, Muller R, Vollert J, Muller C, Danne O, Gareis R, Stork T, Dietz R, Koenig W. Lipoprotein-associated phospholipase A2 for early risk stratification in patients with suspected acute coronary syndrome: a multi-marker approach: the North Wuerttemberg and Berlin Infarction Study-II (NOBIS-II) Clin Res Cardiol. 2007;96:604–612. doi: 10.1007/s00392-007-0540-x. [DOI] [PubMed] [Google Scholar]
- 20.Wilson EB. Probable inference, the law of succession, and statistical inference. J Am Stat Assoc. 1927;22:209–212. [Google Scholar]
- 21.Hamm CW, Bassand JP. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2011;32:2999–3054. doi: 10.1093/eurheartj/ehr236. [DOI] [PubMed] [Google Scholar]
- 22.Keller T, Zeller T, Peetz D, Tzikas S, Roth A, Czyz E, Bickel C, Baldus S, Warnholtz A, Frohlich M, Sinning CR, Eleftheriadis MS, Wild PS, Schnabel RB, Lubos E, Jachmann N, Genth-Zotz S, Post F, Nicaud V, Tiret L, Lackner KJ, Munzel TF, Blankenberg S. Sensitive troponin I assay in early diagnosis of acute myocardial infarction. N Engl J Med. 2009;361:868–877. doi: 10.1056/NEJMoa0903515. [DOI] [PubMed] [Google Scholar]
- 23.Reichlin T, Hochholzer W, Bassetti S, Steuer S, Stelzig C, Hartwiger S, Biedert S, Schaub N, Buerge C, Potocki M, Noveanu M, Breidthardt T, Twerenbold R, Winkler K, Bingisser R, Mueller C. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med. 2009;361:858–867. doi: 10.1056/NEJMoa0900428. [DOI] [PubMed] [Google Scholar]
- 24.Giannitsis E, Becker M, Kurz K, Hess G, Zdunek D, Katus HA. High-sensitivity cardiac troponin T for early prediction of evolving non-ST-segment elevation myocardial infarction in patients with suspected acute coronary syndrome and negative troponin results on admission. Clin Chem. 2010;56:642–650. doi: 10.1373/clinchem.2009.134460. [DOI] [PubMed] [Google Scholar]
- 25.Keller T, Zeller T, Ojeda F, Tzikas S, Lillpopp L, Sinning C, Wild P, Genth-Zotz S, Warnholtz A, Giannitsis E, Mockel M, Bickel C, Peetz D, Lackner K, Baldus S, Munzel T, Blankenberg S. Serial changes in highly sensitive troponin I assay and early diagnosis of myocardial infarction. JAMA. 2011;306:2684–2693. doi: 10.1001/jama.2011.1896. [DOI] [PubMed] [Google Scholar]
- 26.Reichlin T, Schindler C, Drexler B, Twerenbold R, Reiter M, Zellweger C, Moehring B, Ziller R, Hoeller R, Rubini GM, Haaf P, Potocki M, Wildi K, Balmelli C, Freese M, Stelzig C, Freidank H, Osswald S, Mueller C. One-hour rule-out and rule-in of acute myocardial infarction using high-sensitivity cardiac troponin T. Arch Intern Med. 2012;172:1211–1218. doi: 10.1001/archinternmed.2012.3698. [DOI] [PubMed] [Google Scholar]
- 27.Hammarsten O. Small changes in cardiac troponin levels are common in patients with myocardial infarction: diagnostic implications. Conf Pap Med. 2013;2013:1–5. [Google Scholar]
- 28.Dissmann W, de Ridder M. The soft science of German cardiology. Lancet. 2002;359:2027–2029. doi: 10.1016/S0140-6736(02)08825-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.