Abstract
Purpose:
To measure the effects associated with sequential implementation of electronic medication storage and inventory systems and product verification devices on pharmacy technical accuracy and rates of potential medication dispensing errors in an academic medical center.
Methods:
During four 28-day periods of observation, pharmacists recorded all technical errors identified at the final visual check of pharmaceuticals prior to dispensing. Technical filling errors involving deviations from order-specific selection of product, dosage form, strength, or quantity were documented when dispensing medications using (a) a conventional unit dose (UD) drug distribution system, (b) an electronic storage and inventory system utilizing automated dispensing cabinets (ADCs) within the pharmacy, (c) ADCs combined with barcode (BC) verification, and (d) ADCs and BC verification utilized with changes in product labeling and individualized personnel training in systems application.
Results:
Using a conventional UD system, the overall incidence of technical error was 0.157% (24/15,271). Following implementation of ADCs, the comparative overall incidence of technical error was 0.135% (10/7,379; P = .841). Following implementation of BC scanning, the comparative overall incidence of technical error was 0.137% (27/19,708; P = .729). Subsequent changes in product labeling and intensified staff training in the use of BC systems was associated with a decrease in the rate of technical error to 0.050% (13/26,200; P = .002).
Conclusions:
Pharmacy ADCs and BC systems provide complementary effects that improve technical accuracy and reduce the incidence of potential medication dispensing errors if this technology is used with comprehensive personnel training.
Keywords: barcode technology, electronic inventory, error rate, pharmacy, technician
Clinical pharmacy is the health science discipline devoted to optimization of medication therapy for promotion of wellness and disease prevention.1 Inherent in this professional definition is a strong emphasis on promoting patient safety and minimizing drug misadventures. Dispensing errors are infrequent but important causes of preventable adverse drug events.2,3 Minimization of dispensing errors is of paramount importance in optimizing patient safety.
One of the first patient safety measures to receive widespread adoption by clinically oriented hospital pharmacies is the unit-of-use or unit dose (UD) drug distribution system. Because the UD drug distribution system proved to significantly reduce medication errors as compared to traditional ward- or floor-stock systems,4,5 it has been the standard used in North American hospitals for many years.6
The efficiency of UD drug distribution systems in hospitals has been enhanced by the adoption and deployment of automated dispensing cabinets (ADCs) such as those manufactured and serviced by Omnicell (OmniRx, Savvy; Mountain View, CA), Aesynt (AcuDose-Rx; Cranberry Township, PA), and CareFusion (Pyxis MedStation; San Diego, CA). ADCs enable on-demand, ready access to UD medications in a wide variety of patient care areas with a high degree of built-in safeguards.7, 8 When utilized with careful supervisory oversight, these devices have been shown to decrease medication administration errors.9–12 For this reason, professional pharmacy organizations generally are supportive of implementation and utilization of ADCs in institutional patient care areas.13
ADCs designed for use within the hospital pharmacy are likewise available (eg, NarcStation from Aesynt; Pyxis CIISafe from CareFusion). Pharmacy-based ADCs offer continuous electronic inventory control and segregated storage for pharmaceuticals and supplies. When used in the pharmacy, the effect of these devices on dispensing errors is presently unknown.
Barcode (BC)–assisted medication administration systems reduce medication administration errors.14–18 Similarly, use of BC product verification during selection, preparation, and dispensing of electronically ordered pharmaceuticals has resulted in reduced rates of dispensing errors.19–26 Accordingly, implementation and use of BC technology in dispensing procedures has received enthusiastic professional endorsement.27
The University of Colorado Hospital (UCH) is a 533-bed academic medical center that serves as the primary teaching hospital in the Rocky Mountain region of the United States. This hospital has a pharmacy service operated by a staff of approximately 140 professional and ancillary personnel. The mission of the hospital’s clinical pharmacy program — to improve lives by providing efficient, safe, and effective pharmaceutical care for every patient while fostering research and learning — is supported by a drug distribution system comprised of both traditional and innovative new methodologies. The purpose of this report is to recount the patient safety implications of the stepwise application of ADC and BC technologies in the inpatient drug distribution system at UCH.
Methods
This study was approved by the local ethics committee (Colorado Multiple Institutional Review Board [COMIRB], protocol no. 07-0972) and the UCH Research Review Committee. The objectives of this study were 3-fold. First, we sought to determine the incidence of technical errors committed during the set-up preparation of patient-specific medication order fills and refills. Second, we sought to identify the categorical types of errors committed in setting up medication fills and refills. Third, we sought to compare the accuracy of conventional and electronically directed medication filling procedures by assessing the error rate attributable to pharmacy personnel with varying levels of training and experience working in these differing environments.
This was a prospective observational study. Observational findings were used to assess procedural efficiencies and to sequentially evaluate the effects associated with implementation of automated dispensing tools on technical accuracy within the central hospital pharmacy. The plan of work included a procedural review of work orders for hospitalized patients with recording of specific information relevant to the accuracy of filling medication orders.
Inclusion and Exclusion Criteria
Patients’ records were eligible for inclusion in this study if they contained providers’ orders for prescriptions or over-the-counter medications during any one of four 28-day periods of observation. These periods correspond to observation times before and again after a change in practice site with moves to new hospital facilities and the subsequent stepwise implementation of electronically directed dispensing systems.
Items eligible for inclusion in evaluations of filling accuracy were pharmaceuticals. These included commercially UD packaged oral or enteral solid and liquid medications, large- and small-volume parenterals, locally packaged solids, liquids, and parenterals as well as intravenous (IV) admixtures. Parenteral nutrition fluids and medications utilized within various surgical and procedural areas were excluded.
Observations
Prescription record data were allocated to observational groups differentiated by treatment site (former and current UCH campuses) and drug distribution technologies. Specifically, these groups comprised data recorded during 4 distinct periods of observation:
Period 1; UD, April 19 to May 17, 2007. In the previous hospital facility, inpatient medications were dispensed in response to handwritten provider orders. Following receipt of scanned digital images of written orders, prescriptions were computerized by pharmacist order entry. This facility utilized a conventional UD medication storage system in which medications were contained in open bins arranged alphabetically on multi-tiered shelving. Study data were recorded during completion of new or first-time drug orders and daily patient care area ADC refills or patient-specific loads.
Period 2; UD/ADC, January 21 to February 17, 2008. Following the move to a new hospital facility, prescription orders were computerized in a manner similar to that described above using a conventional pharmacist order entry system. In this facility, however, the central inpatient pharmacy was configured with segregated (non-alphanumerical) medication storage in electronically controlled ADCs (Pyxis MedStation 4000; CareFusion CA) adapted for use within the central inpatient pharmacy.
Period 3; UD/ADC/BC1, February 11 to March 10, 2013. Following a second move to a new location within the newer hospital, prescription orders in this phase of study were processed as computerized orders entered by providers and verified by pharmacists. Orders were completed within the central inpatient pharmacy using the UD/ADC system in conjunction with a BC scan-enabled product verification system (Epic Willow; Epic Systems Corporation, Verona, WI). This phase of study commenced within the fourth month following activation of the BC system.
Period 4; UD/ADC/BC2, June 10 to July 7, 2013. This evaluation period entailed use of the above BC scan-enabled system following product labeling changes and re-training of all involved pharmacy personnel along with full implementation of BC scan-enabled product verification within the clean-room sterile product preparation area.
Study-related Procedures
As in most US hospitals, at UCH a licensed pharmacist checks all prescribed medications for content accuracy prior to dispensing. Typically, the medication to be dispensed is selected by a pharmacy technician or intern. Along with the printed order label, a predetermined number of doses of the medication is placed in a designated location for a pharmacist’s final check before being placed into a labeled container for transport to the patient care area.
During each of the periods of observation, this study used a handwritten tally sheet completed by hospital pharmacists during the final check prior to dispensing of pharmaceuticals. Tally sheets were prominently displayed at each of 4 locations within the pharmacy where pharmacist checking was conducted. The pharmacist was requested to record all technical errors and discrepancies in which the technician’s or intern’s medication set-up deviated in any way from the order specified by computer entry. Similar procedures were used to identify and record deviations in order set-ups for medications dispensed as sterile products (ie, medicated IV fluids).
In each of the various periods of observation, technical responsibilities were performed by certified pharmacy technicians or pharmacy interns. At hiring, these individuals received detailed, hands-on training by both supervisory and front-line technical staff covering all aspects of technician responsibilities. Prior to each phase of the study, additional group training was provided relative to operation of each new distributive technology. This included all aspects of drug product selection and retrieval using ADCs and, in the latter phases of study, use of BC scanners.
To ensure an exact product match, proper application of BC scan-enabled product verification requires that the operator scan both the barcoded drug product label imprinted on each dose of medication as well as the barcoded patient-specific product work label. These steps must be completed prior to compiling the set-up display of the completed medication order for the pharmacist’s final check.
Prior to the final phase of the study in which BC-enabled scanning and product verification were used, individualized instruction and re-training was provided to all technicians. Secondary training emphasized reasons for use of BC scanning and the importance of consistent use of this system to minimize errors and, in turn, to promote patient safety. This instruction was accompanied by work flow changes in which product quantities were clarified by changing the font on the pharmacy product work label. The final study phase also comprised evaluation of numbers and types of technical errors associated with preparation of various IV admixtures in a BC scan-enabled product verification system used in a new clean-room sterile product preparation area. Individualized personnel training was provided regarding effective use of BC systems in this location.
Data Analysis
Numbers, types, and (if known) reasons for drug product selection errors or discrepancies were recorded and subsequently analyzed as a percentage of the total number of medication orders processed. Relative risk (RR) was calculated as incidence of error among orders processed in the newer system divided by incidence of error among orders processed in the former or older system. Incidence rates were compared by construction of 2×2 contingency tables and statistical testing with chi-square or Fisher’s exact probability tests. Analyses were conducted using IBM SPSS Statistics Standard, Version 19 (IBM Corp., Armonk, NY).
Results
Data regarding numbers of oral and injectable UD products dispensed and technical errors or predispensing product discrepancies that were recorded by pharmacists during each of the periods of observation are summarized in Table 1. As shown, the overall incidence of technical errors varied according to study period from 0.157% during the UD phase to 0.135% during the UD/ADC phase and to 0.137% in the initial UD/ADC/BC phase. Although incidence rates declined during the study phases in which ADC and BC technologies were added, differences in overall technical error rates among these phases were small and not significant. As compared with the preceding UD/ADC/BC phase, the final phase of the oral and injectable UD dispensing study in which BC scanning was used showed a decrease in technical error rate from 0.137% to 0.050% (P = .002).
Table 1. Incidence and relative risk (RR) of technical dispensing errors or discrepancies among oral and injectable pharmaceutical products identified during utilization of conventional unit dose (UD), pharmacy automated dispensing cabinet (ADC), and barcode (BC) systems by year and phase of study.
| UD 2007 | UD/ADC 2008 | UD/ADC/BC1 2013 | UD/ADC/BC2 2013 | |
| Items dispensed | 15,271 | 7,379 | 19,708 | 26,200 |
| Discrepancies | 24 | 10 | 27 | 13 |
| Incidence (%) | 0.157 | 0.135 | 0.137 | 0.050 |
| RR vs UD | – | 0.86 | 0.87 | 0.32 |
| P value | – | .841 | .729 | <.001 |
| RR vs UD/ADC | – | – | 1.01 | 0.37 |
| P value | – | – | .998 | .013 |
| RR vs UD/ADC/BC1 | – | – | – | 0.36 |
| P value | – | – | – | .002 |
Note: Incidence rates were compared by construction of 2×2 contingency tables and statistical testing with chi-square or Fisher’s exact probability tests. P < .05 is statistically significant.
The predominant types of technical errors or product discrepancies changed during each phase of the oral and injectable UD dispensing study (Figure 1). Whereas wrong drug product selection errors comprised 75% and 80% of technical errors in the UD and UD/ADC phases of study, respectively, implementation of BC-enabled scanning and product verification was associated with a decrease in these types of errors. Although wrong drug errors seldom or never occurred in the UD/ADC/BC phases of study, quantity errors in which an incorrect number of doses were prepared for dispensing accounted for more than 60% of technical errors in these phases.
Figure 1.
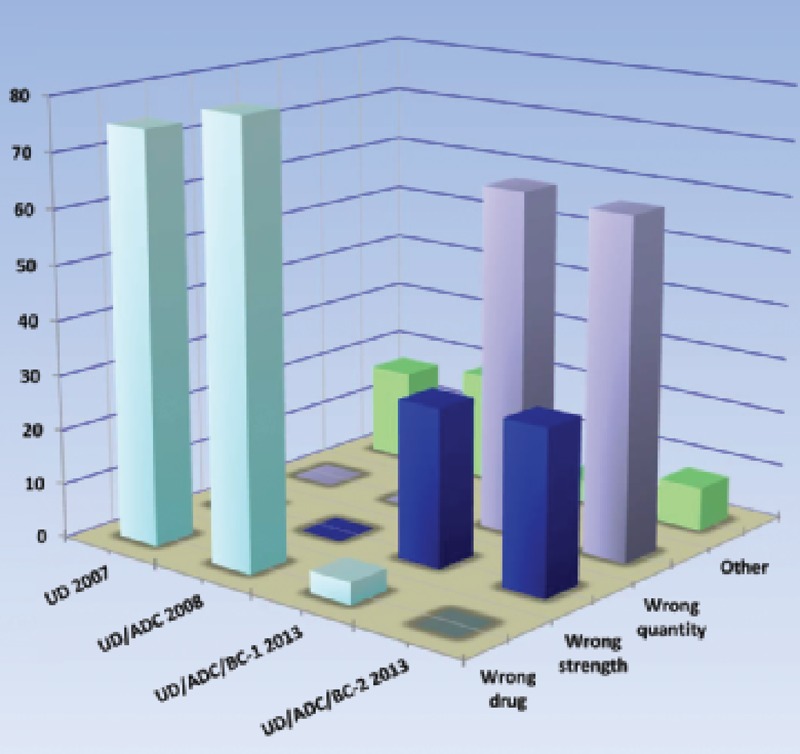
Percentages of various types of potential technical dispensing errors for oral and injectable medications identified during utilization of conventional unit dose (UD), pharmacy automated dispensing cabinet (ADC), and barcode (BC) systems by year of study.
Numbers of IV products dispensed and associated technical errors or product discrepancies in parenteral admixture preparation were recorded during the first period of observation in 2007 and during the final period in 2013 after implementation of ADCs and BC scanning within the clean room. These data are displayed in Table 2. As shown, the overall incidence of technical errors decreased from 0.636% (24/3,776) during the UD phase of study to 0.046% (4/8,658) during the final UD/ADC/BC2 phase (P < .001).
Table 2. Incidence and relative risk (RR) of technical errors or discrepancies among parenteral admixtures identified during utilization of conventional unit dose (UD), pharmacy automated dispensing cabinet (ADC), and barcode (BC) systems by year and phase of study.
| UD 2007 | UD/ADC/BC2 2013 | |
| Items dispensed | 3,776 | 8,658 |
| Discrepancies | 24 | 4 |
| Incidence (%) | 0.636 | 0.046 |
| RR vs UD | — | 0.072 |
| P value | — | <.001 |
Note: Incidence rates were compared by construction of 2×2 contingency tables and statistical testing with chi-square or Fisher’s exact probability tests. P < .05 is statistically significant.
Technical errors involving look alike–sound alike mix-ups and wrong IV drug product selection associated with product storage proximity comprised 84% of errors in the UD phase of the IV study, whereas wrong fluid volume errors accounted for 75% of errors in the UD/ADC/BC2 phase.
Discussion
Repeated assessments of the patient safety implications associated with the sequential implementation of new technologies in the drug distribution system at UCH demonstrated improvements in technical accuracy in certain areas that often came at the expense of increased errors or development of new problems in other areas. Although new technologies generally increased technical accuracy, clear benefit in terms of numbers of errors was realized only after intensified individual training was provided to all technical staff regarding the importance of correct application and consistent use of these systems.
Pharmacy-based Automated Dispensing Cabinets
As compared with a conventional UD drug distribution system, implementation of continuous electronic inventory control through storage of all oral and injectable medications and controlled substances within pharmacy-based ADCs resulted in little change in either the incidence or the type of technical errors detected by pharmacists. The primary reason for this lack of change is believed to lie with the manner in which ADCs typically operate.
In the UD phase, drugs were stored alphabetically by generic name according to strength in plastic or fiberboard storage bins on 9- to 11-tier shelving. This configuration was prone to selection error because of the close storage proximity of medications with sequential names and strengths with corresponding risk for item return mix-ups. These issues were resolved with implementation of ADCs and use of non-alphabetical storage and look alike–sound alike product separation. However, when using the ADC, drug selection is made with a console-mounted touch-screen monitor that displays an alphanumeric listing of all available medications. Due to the close proximity of related line items in the list, touch-screen selection miscues often result in errors that involve picking wrong strengths of drugs or look alike–sound alike medications. These findings are consistent with detailed performance studies in which proximity of multiple similarly named nontarget medications within the specified visual field was shown to significantly decrease selection accuracy.28
Barcode Technology
BC-enabled scanning and product verification offers a logical, proven, and highly recommended means to decrease dispensing errors. In our experience, however, initial implementation of this technology in the oral and injectable UD dispensing study was associated with essentially no change in the incidence of technical errors. Although no numerical difference in incidence occurred, BC-enabled scanning and product verification were associated with a shift in the most common type of error from wrong drug to wrong quantity errors in which the number of doses to be dispensed deviated from the number specified on the pharmacy work label. This finding was attributed in part to a weakness in the BC system, because no alerting or warning is presented if the number of doses scanned deviates from the number of doses ordered.
Although it might be suggested that, from a patient safety point of view, a quantity error is potentially less serious than a wrong drug error, these are indeed errors and they likely will result at least in missing medication issues with potential for confusion, delayed or omitted medication treatment, and interdepartmental friction. These errors might be preventable with greater technical vigilance, but we chose to seek additional means to address the disappointing numerical results arising from recurring wrong quantity errors.
During the BC scan-enabled product verification phase of the study, discrepancies between numbers of doses ordered and numbers of doses filled invariably occurred due to technical inattention to the number of doses required during the current medication fill cycle as printed on the pharmacy work label. To mitigate inattention and lessen the likelihood of error, a 2-part strategy was used. First, the font size of the print line in which numbers of doses to be dispensed appear was increased in size from 9 to 14 points. Second, by tracking the order number of each medication set-up that contained an incorrect number of doses, the number of quantity errors associated with each technician was determined. Subsequently, this was individually reviewed with each technician in a private interview with pharmacy supervisors. This was accompanied by a discussion of the importance of providing an adequate number of doses to complete the current fill cycle from a patient safety perspective along with a general re-training overview of the BC-enabled scanning and product verification process.
The process change and re-training strategy was subsequently associated in the final study phase with a decrease in the number of quantity errors by more than 50%. Comprehensive training and thorough understanding of the importance of full compliance with correct procedures imposed by the BC system appeared to be vitally important in realizing a numerical decrease in potential dispensing errors. Anecdotally, ongoing use of the BC system has increased staff familiarity and trust of the system’s capabilities. It appears that this is associated with a continuing rate of technical error that is comparatively low.
As compared with the first phase, the final study phase was performed after the hospital IV room was moved to a new US Pharmacopoeia (USP) chapter <797> compliant Class A clean-room facility equipped with complete BC-enabled scanning and product verification capability. This change was associated with a significant decline in the incidence of technical errors and a shift in predominant error type from wrong IV drug product selection to wrong volume errors. This change in error type in the latter phase of study was associated at least in part with a system weakness — BC scanning wrong-sized IV fluid containers is not detected and alerted as an error.
Similar to our experience, training factors have been previously identified as an important barrier that must be addressed to enable successful implementation of BC scanning systems for accurate medication dispensing.29 Together, these experiences serve to emphasize the importance of failsafe technical support in enabling clinical pharmacists to fulfill their patient safety obligations.
Limitations
As with similar observational studies, our evaluation has a number of important limitations. Our findings are reflective of experience from a single institution with limited periods of observation. This study was performed with an open, uncontrolled design and a requested assessment of pharmacy technical errors provided at the discretion of individual staff pharmacists. Recording of specific prescription order deviations of interest was performed manually, and no automated means of error detection was available. Other than initial on-the-job training, staff pharmacists were not required to demonstrate understanding and competence in checking the content accuracy of medications to be dispensed.30 As reflected by large differences in numbers of items dispensed, the physical locations, service areas, and patient populations changed prior to each phase of study. Last and perhaps most important, the reliability of conclusions drawn from this evaluation of ADC and BC technology is hindered because this was a “business as usual” experience that occurred over a 7-year span. During this period of time, multiple personnel, facility, communication, and workflow changes occurred that could not be controlled, adjusted, or accounted for in our data analysis. Nonetheless, this assessment of the effects of newer technology on pharmacy technical accuracy offers a perspective taken from typical contemporary hospital practice and, as such, it is generally representative of what may be expected with implementation of various technologies in a broad spectrum of health system pharmacy practice.
The advancement of pharmacy practice hinges on professional ability to provide efficient, cost-effective and, above all else, safe medication treatment. Electronic inventory systems incorporating ADCs and BC scan-enabled product verification provide complementary effects that improve pharmacy technical accuracy and reduce the incidence of potential dispensing errors, provided that these technologies are utilized consistently by conscientious, well-trained personnel.
Acknowledgments
The authors have no conflicts of interest to declare.
References
- 1.American College of Clinical Pharmacy. The definition of clinical pharmacy. Pharmacotherapy. 2008;28:816–817. [DOI] [PubMed] [Google Scholar]
- 2.Beso A, Franklin BD, Barber N.The frequency and potential causes of dispensing errors in a hospital pharmacy. Pharm World Sci. 2005;27:182–190. [DOI] [PubMed] [Google Scholar]
- 3.Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse drug events and potential adverse drug events: Implications for prevention. JAMA. 1995;274:29–34. [PubMed] [Google Scholar]
- 4.Means BJ, Derewicz J, Lamy PP.Medication errors in a multidose and computer-assisted unit dose drug distribution system. Am J Hosp Pharm. 1975;32:186–191. [PubMed] [Google Scholar]
- 5.Schultz SM, White SJ, Latiolais CJ.Medication errors reduced by unit dose. Hospitals. 1973;47(6):106–112. [PubMed] [Google Scholar]
- 6.American Society of Hospital Pharmacists. ASHP statement on unit dose drug distribution. Am J Hosp Pharm. 1975;32:835. [PubMed] [Google Scholar]
- 7.Lee LW, Wellman GS, Birdwell SW, Sherrin TP.Use of an automated medication storage and distribution system. Am J Hosp Pharm. 1992;49:851–855. [PubMed] [Google Scholar]
- 8.Grissinger M, Globus NJ.How technology affects your risk of medication errors. Nursing. 2004;34(1):36–41. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz HO, Brodowy BA.Implementation and evaluation of an automated dispensing system. Am J Health Syst Pharm. 1995;52:823–828. [DOI] [PubMed] [Google Scholar]
- 10.Borel JM, Rascati KL.Effect of an automated, nursing unit-based drug-dispensing device on medication errors. Am J Health Syst Pharm. 1995;52:1875–1879. [DOI] [PubMed] [Google Scholar]
- 11.Skibinski KA, White BA, Lin LI-K, Dong Y, Wu W.Effects of technological interventions on the safety of a medicationuse system. Am J Health Syst Pharm. 2007;64:90–96. [DOI] [PubMed] [Google Scholar]
- 12.Chapuis C, Roustit M, Bal G, et al. Automated dispensing system reduces medication errors in an intensive care setting. Crit Care Med. 2010;38:2275–2281. [DOI] [PubMed] [Google Scholar]
- 13.American Society of Health System Pharmacists. ASHP guidelines on the safe use of automated dispensing devices. Am J Health Syst Pharm. 2010;67:483–490. [DOI] [PubMed] [Google Scholar]
- 14.Paoletti RD, Suess TM, Lesko MG, et al. Using bar-code technology and mediation observation methodology for safer medication administration. Am J Health Syst Pharm. 2007;64:536–543. [DOI] [PubMed] [Google Scholar]
- 15.Helmons PJ, Wargel LN, Daniels CE.Effect of bar-code-assisted medication administration on medication administration errors and accuracy in multiple patient care areas. Am J Health Syst Pharm. 2009;66:1202–1210. [DOI] [PubMed] [Google Scholar]
- 16.Morriss FH, Jr, Abramowitz PW, Nelson SP, et al. Effectiveness of barcode medication administration system in reducing preventable adverse drug events in a neonatal intensive care unit: A prospective cohort study. J Pediatr. 2009;154:363–368. [DOI] [PubMed] [Google Scholar]
- 17.Poon EG, Keohane CA, Yoon CS, et al. Effect of bar-code technology on the safety of medication administration. N Engl J Med. 2010;362:1698–1707. [DOI] [PubMed] [Google Scholar]
- 18.Early C, Riha C, Martin J, Lowdon KW, Harven EM.Scanning for safety: An integrated approach to improved bar-code medication administration. Comput Inform Nurs. 2011;29(4 suppl): TC45–52. [DOI] [PubMed] [Google Scholar]
- 19.Meyer GE, Brandell R, Smith JE, Milewski FJ, Jr, Brucker P, Jr, Coniglio M.Use of bar codes in inpatient drug distribution. Am J Hosp Pharm. 1991;48:953–966. [PubMed] [Google Scholar]
- 20.Ragan R, Bond J, Major K, Kingsford T, Eidem L, Garrelts JC.Improved control of medication use with an integrated bar-code-packaging and distribution system. Am J Health Syst Pharm. 2005;62:1075–1079. [DOI] [PubMed] [Google Scholar]
- 21.Flynn EA, Barker KN.Effect of automated dispensing system on errors in two pharmacies. J Am Pharm Assoc. 2006;46:613–615. [DOI] [PubMed] [Google Scholar]
- 22.Poon EG, Cina JL, Churchill WW, et al. Medication dispensing errors and potential adverse drug events before and after implementing bar code technology in the pharmacy. Ann Intern Med. 2006;145:426–434. [DOI] [PubMed] [Google Scholar]
- 23.Cina J, Fanikos J, Mitton P, McCrea M, Churchill W.Medication errors in a pharmacy-based bar-code-repackaging center. Am J Health Syst Pharm. 2006;63:165–168. [DOI] [PubMed] [Google Scholar]
- 24.O’Neal BC, Worden JC, Couldry RJ.Telepharmacy and bar-code technology in an IV chemotherapy admixture area. Am J Health Syst Pharm. 2009;66:1211–1217. [DOI] [PubMed] [Google Scholar]
- 25.Galbraith W, Shadid J.Compounding and dispensing errors before and after implementing barcode technology in a nuclear pharmacy. Int J Pharm Compd. 2012;16:253–256. [PubMed] [Google Scholar]
- 26.Helmons PJ, Dalton AJ, Daniels CE.Effects of a direct refill program for automated dispensing cabinets on medicationrefill errors. Am J Health Syst Pharm. 2012;69:1659–1664. [DOI] [PubMed] [Google Scholar]
- 27.American Society of Health System Pharmacists. ASHP statement on bar-code verification during inventory, preparation, and dispensing of medications. Am J Health Syst Pharm. 2011;68:442–445. [DOI] [PubMed] [Google Scholar]
- 28.Irwin A, Mearns K, Watson M, Urquhart J.The effect of proximity, tall man lettering, and time pressure on accurate visual perception of drug names. Hum Factors. 2013;55:253–266. [DOI] [PubMed] [Google Scholar]
- 29.Nanji KC, Cina J, Patel N, Churchill W, Gandhi TK, Poon EG.Overcoming barriers to the implementation of a pharmacy bar code scanning system for medication dispensing: A case study. J Am Med Inform Assoc. 2009;16:645–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.James KL, Davies JG, Kinchin I, Patel JP, Whittlesea C.Understanding vs. competency: The case of accuracy checking dispensed medicines in pharmacy. Adv Health Sci Educ Theory Pract. 2010;15:735–747. [DOI] [PubMed] [Google Scholar]


