Abstract
Background: Childhood obesity is highly prevalent, is associated with both short- and long-term adverse outcomes, disproportionately affects racial/ethnic minority and economically deprived children, and represents a major threat to public health. Among the most promising approaches for its prevention and management are multilevel, multisector strategies.
Methods/Design: The Massachusetts Childhood Obesity Research Demonstration (MA-CORD) Study was a comprehensive, systematic intervention to prevent and reduce childhood obesity among low-income children ages 2–12 years in two selected cities in Massachusetts. Building on the Obesity Chronic Care Model, MA-CORD expanded a state public health department community-level obesity prevention initiative that incorporated evidence-based interventions in primary healthcare, the Women, Infants, and Children program, early care and education, schools/afterschool programs, as well as community-wide programs to improve food, beverage, physical activity (PA), and messaging environments. The study used a combination of pre– and post–time series and quasi-experimental designs to examine the extent to which the intervention resulted in changes in BMI, individual-level lifestyle behaviors, satisfaction with healthcare services, and quality of life among children, as well as changes in health policies, programs, and environments in the two intervention cities, compared to a comparison city. The intervention period was 2 years.
Conclusions: MA-CORD will determine the extent to which a multisetting, multilevel intervention that integrates activities in primary care with broader public health interventions in schools, early care and education, and the community at large can improve children's dietary and PA behaviors and ultimately reduce obesity in low-income children.
Introduction
Obesity represents a major threat to public health and results in significant excess burden of chronic diseases, adverse quality of life, and health and societal costs.1–4 Though obesity rates in the United States may have plateaued in some population subgroups, overall rates remain stubbornly high and racial/ethnic and socioeconomic disparities appear to be increasing.5,6 Many factors contribute to the intractability of obesity and related racial, ethnic, and socioeconomic disparities, ranging from the social, built, and economic environments to individual behaviors and physiology. Given the complexity and interconnectedness of etiologic factors of obesity, proposed solutions will need to be similarly broad and include sustainable, cost-effective, multisector strategies that support change at the individual, system, and community levels.7–9
The Massachusetts Childhood Obesity Research Demonstration (MA-CORD) Study was designed to implement and test an integrated approach across multiple sectors and levels to prevent and treat obesity among low-income children. MA-CORD was designed in the context of a comprehensive, state-wide wellness initiative launched by the Massachusetts Department of Public Health (MDPH), Mass in Motion.
MA-CORD was funded by the CDC in response to the legislative mandate in the reauthorization of the Children's Health Insurance Program and appropriations through the Affordable Care Act.10 Dooyema and colleagues have previously published on the CORD framework and innovation, which includes a description of the additional demonstration grantees in Texas and California.10 This article will summarize the conceptual framework, design, and methods of MA-CORD. A companion article focuses on the specific evaluation plan and baseline results.11
Conceptual Framework
Our intervention drew upon the recommendations from the Institute of Medicine of integrating primary care with public health programs to improve the health of populations.12 The two overarching models for MA-CORD were the chronic care model (CCM) originally developed by Wagner and colleagues13 and the energy gap model (EGM) for children that quantifies associations of changes in energy intake and expenditure with weight change.9,14–16 The CCM informed our approach to changing primary care and the healthcare system by identifying the essential elements of a healthcare system that encourage high-quality care of chronic conditions: the community; the health system; family and self-management support; delivery system design; decision support; and clinical information systems. MA-CORD implemented changes to each element of the CCM to improve childhood obesity screening and management across clinical and community settings as well as among families.
Community and environmental interventions were chosen based on their potential to reduce the childhood energy gap and ability to be incorporated into the initiatives already underway through existing Mass in Motion projects. Wang and colleagues15 have proposed the EGM for children, which suggests that changes averaging 64 kcal/day could meet the 2020 Healthy People goal for children ages 2–19 years. The energy gap approach helps to identify dietary and physical activity (PA) behaviors that can alter energy balance. In addition, all of our intervention approaches build on social cognitive theory to identify and target critical social and environmental factors underlying the performance of specific health-related behaviors in different settings where children spend their days.17–24
Methods
Overview of Study Design
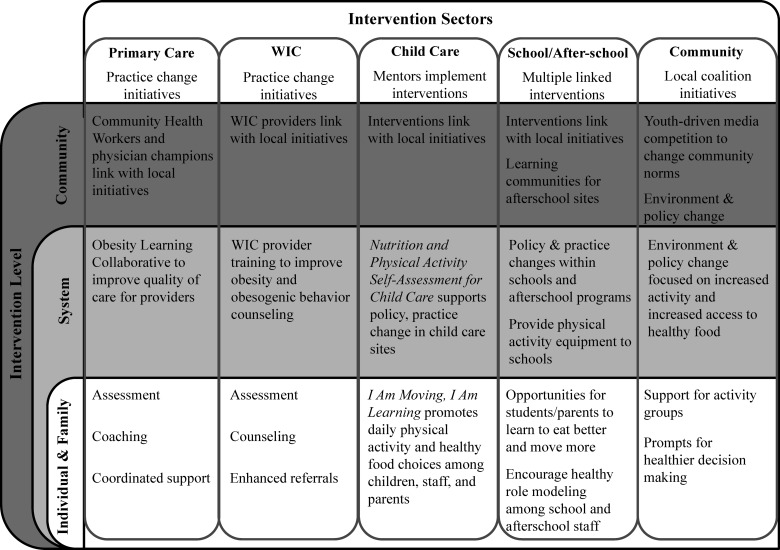
MA-CORD was a multisector, multilevel whole-of-community intervention in Fitchburg and New Bedford, Massachusetts, that incorporated evidence-based interventions across multiple sectors and at multiple levels (Fig. 1). The overall aim of the study was to examine the extent to which the comprehensive, systematic intervention reduced childhood obesity among underserved children. Evidence-based interventions were incorporated in (1) pediatric primary care, (2) the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC); (3) early care and education, (4) public elementary and middle schools and afterschool programs, and (5) policy change and community-wide programs to improve food, beverage, PA, and messaging environments among predominantly low-income children ages 2–12 years. The study used a combination of pre– and post–time series and quasi-experimental designs to examine the extent to which the interventions resulted in changes in BMI, individual-level lifestyle behaviors, satisfaction with healthcare services, and quality of life among children, as well as changes in health policies, programs, and environments in the two intervention cities, compared to a comparison city. The intervention period was 2 years. The study protocol was approved by the human subjects committees of the MDPH, Harvard School of Public Health, Massachusetts General Hospital, and Harvard Pilgrim Health Care Institute.
Figure 1.
Massachusetts Childhood Obesity Research Demonstration (MA-CORD) Study overview. WIC, The Special Supplemental Nutrition Program for Women, Infants, and Children.
Building Upon a State-wide Initiative
In 2009, the MDPH launched Mass in Motion, a community-based, multifaceted initiative to address the growing public health threat posed by obesity and its numerous adverse health consequences. The Mass in Motion initiative included: (1) an executive order requiring implementation of strict nutrition guidelines in state food procurement; (2) the development of regulations requiring BMI measurement of all school children in grades 1, 4, 7, and 10 and the sharing of this information with local and state policy makers; (3) the development of regulations for strong nutrition standards for competitive foods in public schools; (4) the establishment of a Mass in Motion website25; (5) support and training for more than 60 worksite wellness programs; (6) a joint program with the Department of Early Education and Care to promote PA and healthy eating in child care settings; and (7) Mass in Motion Municipal Wellness grants to 51 communities representing 30% of the state's population to support multisector coalitions to decrease obesity and related chronic diseases.
Eligibility for MA-CORD
Intervention communities and settings
In the Spring of 2011, the MDPH published a request of interest to communities in the Commonwealth (of Massachusetts) for participation in MA-CORD. To be eligible for consideration, municipalities had to be participants in the Mass in Motion initiative,25 have existing coalitions already working on obesity prevention initiatives, and have the support of leaders from the multiple sectors in which interventions were planned. Nine Mass in Motion communities submitted applications, and two communities were selected. Whereas all nine met the requests for applications26 criteria for low income and existing capacity for obesity prevention, Fitchburg and New Bedford scored especially high on a range of relevant criteria, including coalition participation, the availability of trained community health workers, previous successes in planning and implementation of community-based initiatives, and participation in existing obesity prevention initiatives. Both communities received $50,000 Mass in Motion Wellness grants that allowed MA-CORD to leverage the community- and state-wide infrastructure for assessment, planning, and implementation of the community-wide childhood obesity prevention initiatives in the two study communities.
Fitchburg is located in north-central Massachusetts and is home to 40,000 residents. New Bedford is in southeast Massachusetts with 95,000 residents. Both communities have higher percentages of low-income residents than the state as a whole and childhood obesity rates substantially higher than the state-wide average. Population and environmental characteristics of the two communities are shown in Table 1.
Table 1.
Key Preintervention Characteristics of the MA-CORD Study Communities
| Sociodemographic characteristics | Massachusetts | Fitchburga | New Bedford | Comparison |
|---|---|---|---|---|
| Total populationb | 6,436,940 | 40,514 | 94,502 | 106,519 |
| Race/ethnicity | ||||
| % white aloneb | 76.1 | 68.2 | 67.9 | 52.8 |
| % black or African American aloneb | 6.0 | 1.1 | 5.2 | 6.0 |
| % Hispanic or Latino (any race)b | 9.6 | 21.6 | 16.7 | 17.3 |
| Per capita incomec | $35,485 | $22,949 | $21,343 | $23,793 |
| % families with children whose incomes are less than the Federal Poverty levelc | 12.0 | 23.5 | 27.1 | 19.9 |
| Primary care | ||||
| No. of CHCs | 36 | 1 | 1 | 1 |
| No. of CHCs patients <18 years oldd | 137,993 | 6919 | 4861 | 7361 |
| % of CHCs patients enrolled in MassHealth (Medicaid)d | 41.9 | 47.9 | 52.0 | 62.9 |
| % of CHCs patients ≤200% federal poverty leveld | 90.2 | 84.5 | 97.3 | 93.7 |
| Women, Infants, and Children program | ||||
| % of 2- to 5-year-old children overweight/obesee | 33.0 | 32.8 | 33.6 | 22.8 |
| Number of 2- to 5-year-old children enrollede | 61,551 | 838 | 2037 | 2381 |
| Early care and education | ||||
| Number of licensed child care slotsf | 229,312 | 1548 | 3298 | 3727 |
| Public elementary and middle schools | ||||
| Number of elementary schoolsg | 1152 | 4 | 20 | 14 |
| Number of middle schoolsg | 319 | 3 | 3 | 7 |
| Pre-K to fifth grade enrollment, 2012–2013g | 450,633 | 2559 | 7392 | 7447 |
| Grade 6–7 enrollment, 2012–2013g | 143,600 | 743 | 1696 | 3303 |
| % of students in grades 1, 4, 7, and 10 with a BMI ≥85th percentile, 2010–2011h | 32.4 | 40.9 | 39.9 | 35.9 |
Data only available for Community Health Connections, Inc., which includes one health center in Fitchburg and two in the surrounding area of Fitchburg.
2010 U.S. Census.
2008–2012 American Community Survey 5-year estimates.
Health Resources and Services Administration, UDS Summary Report, 2011.
CDC, Pediatric Nutrition Surveillance 2011 report.
Massachusetts Department of Early Education and Care, 2010.
Massachusetts Department of Elementary and Secondary Education, 2012–2013.
Massachusetts Department of Public Health, The Status of Childhood Weight in Massachusetts, 2009–2011.
MA-CORD, Massachusetts Childhood Obesity Research Demonstration; CHCs, federally qualified community health centers.
Comparison community
Based on similar population demographics of the intervention communities, a third Massachusetts community participating in Mass in Motion was selected as a comparison in order to collect individual-level BMI and behavioral information from children who attend a large, federally qualified community health center, WIC, and public elementary and middle schools. As with other communities in the state, the comparison community could continue to plan and carry out health and wellness programs, but it was not expected to have an intensive multilevel intervention such as MA-CORD. Aggregate BMI of children in grades 1, 4, and 7 in the two MA-CORD communities was also compared with those of children across the 311 school districts in Massachusetts in which school-based BMI screening is mandated.
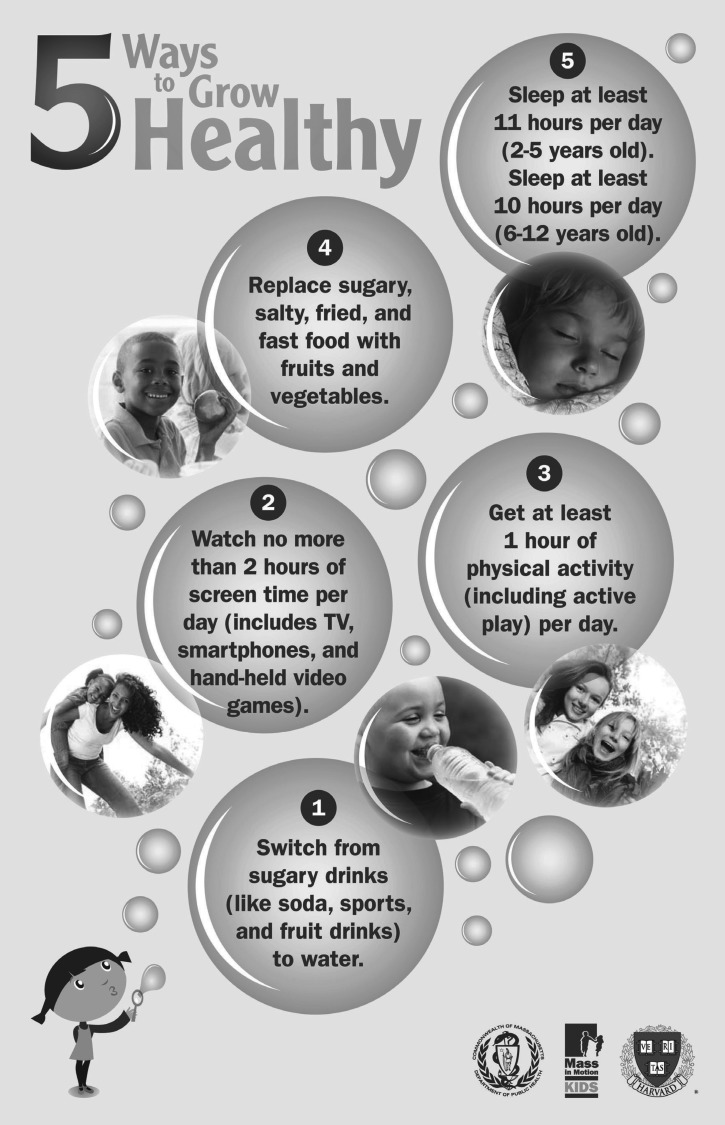
MA-CORD Behavioral Targets
In addition to system-level intervention targets, MA-CORD focused on five individual- and family-level behaviors that are evidence based and potentially actionable (Fig. 2). The behaviors represent domains of screen time,27,28 beverage and diet quality,29 PA,30 and sleep,31–33 which have been shown to have strong influences on child weight regulation and energy imbalance. These include: (1) decreases in screen time and television (TV) sets in bedrooms; (2) decreases in consumption of sugar-sweetened beverages; (3) replacement of nutrient-poor foods with fruits and vegetables; (4) increases in moderate and vigorous PA; and (5) increases in sleep duration and improvement in sleep quality.
Figure 2.
Individual- and family-level behaviors targeted in Massachusetts Childhood Obesity Research Demonstration (MA-CORD). TV, television.
Descriptions of System-Level Interventions by Sector
Clinic intervention
Evidence-based interventions were implemented in both cities' federally qualified community health centers (CHCs).19,34,35 Intervention components aimed to improve primary and secondary prevention of childhood obesity and implemented changes at four levels: clinician; parent-family; organizational; and environmental (Table 2). Additionally, training and educational materials were provided to other pediatric clinicians in the two communities. The clinical intervention components included: (1) advanced training on clinical quality improvement and obesity prevention, assessment, and management; (2) computerized, point-of-care decision support tools for clinicians; (3) implementation of multidisciplinary weight management programs within the CHCs (e.g., healthy weight clinics; HWCs); (4) integrating community health workers (CHWs) into the primary care and HWC teams; and (5) health center environmental changes to support behavior change modification.
Table 2.
MA-CORD Intervention Activities in the Community Health Centers in Fitchburg and New Bedford, Massachusetts
| Clinician | Parent/family | Organizational | Environmental |
|---|---|---|---|
| • Computerized, point-of-care decision support tools to increase BMI screening and obesity-related counseling for all children • Computerized, point-of-care decision support alerts to identify children with a BMI ≥85th percentile and improve adherence to expert committee guidelines on pediatric obesity management • Advanced training on obesity care and motivational interviewing through a modified Breakthrough Series™ Learning Collaborative • Be Our Voice™ Advocacy training to amplify clinicians' knowledge of, and involvement in, local public health approaches for childhood obesity prevention |
• Parent self-assessments of child's behavior risk factors • Consistent messages on targeted behaviors through posters, educational materials, and health center signage • Coordinated support by CHWs to increase confidence in obesity-related behavior change • CHW referral of patients to local resources for physical activity and social support services • Interactive coaching by CHWs for children with BMI ≥85th percentile |
• Modified Breakthrough Series™ Learning Collaborative to improve obesity-related quality of care in the health center • Identification of physician champion, clinical team, and CHW to support practice changes, outreach to community, and participation in local Mass in Motion coalition • Healthy weight clinics with multidisciplinary team for in-house obesity management • Train medical assistants on accurate height and weight measurements |
• Posters in waiting rooms to promote behavioral goals • Social marketing campaign throughout clinical setting to promote obesity-related behavioral targets • Promotion of the use of stairwells within the clinical environment using point-of-decision signage • Highlight healthy choices in health center vending machines • Removal of sugar-sweetened beverages from health center vending machines |
MA-CORD, Massachusetts Childhood Obesity Research Demonstration; CHWs, community health workers.
Clinician training
Teams from local pediatric practices and community organizations serving Fitchburg and New Bedford received advanced training on obesity prevention, assessment, and management through a combination of a modified Breakthrough Series™ Collaborative36 and individualized team coaching to assist with implementation of evidence-based practices within the context of each participating organization. Participants included a physician champion, clinical staff such as nurses or medical assistants, administrative leaders, CHWs, and representatives from Mass in Motion coalitions. Training included: (1) quality improvement language and methods; (2) methods of encouraging health behavior change, including motivational interviewing; (3) best practices in treating childhood obesity; and (4) Be Our Voice™37 Advocacy training, which engages and trains clinicians to be advocates of children in the fight against childhood obesity. Full-day live learning sessions were held every 6 months supplemented by monthly interactive webinars and individualized coaching.
Point-of-care decision support tools
To support evidence-based management of pediatric obesity, existing electronic health records in each health center were modified to deploy a computerized, point-of-care, decision support alert to pediatricians at the time of a well-child care visit for a child with a BMI ≥85th percentile shown to be effective in improving quality of care for overweight children.38,39 The alert contained links to the child's growth chart and a link to a prepopulated, standardized note specific for obesity that included the ability to (1) document and code for BMI percentile and weight status diagnosis; (2) document and code for nutrition and PA counseling; (3) place referrals to the on-site HWC for weight management support; and (4) place orders for obesity-related laboratory studies, if appropriate.
Healthy weight clinics
In each health center, weight management support through multidisciplinary HWCs were developed (Fitchburg) and expanded (New Bedford).35 Each clinic was staffed by a physician champion, a nutritionist, and a CHW who met with each patient and family in tandem during a single clinical encounter. Primary care providers referred eligible patients (BMI ≥85th percentile, ages 2–18) to this specially trained, primary care team. Patients participating in the HWCs engaged in dietary and PA assessment, goal setting, and were connected to community resources to support healthy lifestyles. MA-CORD aimed for patients to be followed in the HWC monthly for a total of 6 months.
Community health workers
As part of MA-CORD, each health center employed a full-time CHW as a member of the primary care and multidisciplinary obesity management teams. The CHWs (1) served as members of the HWC, counseling patients referred to the program; (2) participated in the health centers' quality improvement efforts; (3) served as “wellness navigators” connecting children and families with community resources for increasing PA and eating healthier; and (4) were liaisons to local Mass in Motion coalition activities in the broader community. They also cataloged local community resources to refer patients to, and conducted parent education and training sessions on, the MA-CORD target behaviors, in collaboration with research team staff.
Environmental changes
To improve the healthfulness of the clinical environment and support staff and families' lifestyle modification, MA-CORD worked with health center administrators and the CHWs to implement clinical environmental changes. Subsequent to an environmental assessment, MA-CORD developed a menu of options in which the center could improve. These included signage related to the MA-CORD target behaviors and promotion of water, access to healthy food options within the health center building, and walking challenges.
Women, Infants, and Children
MA-CORD collaborated with the local WIC programs in the intervention communities (one program in each community) to implement evidence-based activities.19,40 Intervention activities included: (1) training of 20 WIC nutritionists and nutrition assistants in best practices on assessment and counseling for childhood obesity prevention; (2) development of an obesity counseling toolkit for WIC providers; (3) encouraging direct referrals from WIC to HWCs; and (4) linking WIC providers to activities in other sectors.
The full-day childhood obesity prevention training for WIC nutritionists and nutrition assistants included: (1) a primer on best practices in childhood obesity prevention; (2) evidence on MA-CORD behavioral targets; (3) a refresher on participant-centered interviewing techniques; (4) an overview of practical approaches to counseling on obesity risk factors; (5) small-group sessions to improve motivational-interviewing skills; and (6) a review of existing WIC education materials to ensure that messaging aligned with MA-CORD. The full-day training was supplemented with an on-site, 2-hour train-the-trainer program focused on sleep and screen time, areas previously identified as high priority in a state-wide WIC needs assessment. Trainings were based on two early childhood obesity prevention interventions that had demonstrated efficacy.19,40 After completion of the train-the-trainer program, WIC trainers delivered the on-site trainings to all local WIC staff in the intervention communities.
Early Child Care and Education
Early care and education providers were trained as “mentors” to assist in engaging six licensed child care centers in each intervention community with a goal to reach approximately 1500 children, linking to an existing joint program established by the MDPH and the Massachusetts Department of Early Education and Care. Before the intervention, mentors received training focused on the five MA-CORD behaviors and two evidence-based interventions to be implemented in the early care and education sector: I Am Moving, I Am Learning (IM/IL)41 and Nutrition and Physical Activity Self-Assessment for Child Care (NAP SACC).42 As with interventions across all the other sectors, community-level change was achieved by linking early care and education centers with other MA-CORD activities. In addition, mentors and child care directors were included in the Mass in Motion coalitions to link them to community-level activities.
IM/IL focuses on individual change through staff training to increase the duration and quality of moderate-to-vigorous PA offered and to promote healthy food choices in early child care settings. An accompanying parent education component of IM/IL also aims to address family-level behaviors.41 NAP SACC is designed to influence individual- and system-level change by enhancing policies, practices, and environments in child care using an organizational assessment of 14 areas of nutrition and PA (including screen time) policy, practices, and environments to identify the strengths and limitations of the early care and education facility. Subsequent to the self-assessment, a mentor works with the early care and education staff to set goals for change and develop plans for follow-up actions to improve practice, through staff training and targeted technical assistance.43,44
Elementary and Middle Schools
Intervention components in each city's public elementary and middle schools aimed to improve the MA-CORD target behaviors among students and make sustainable changes to school wellness programs. The school intervention targeted changes at four levels: student; teacher; organizational; and environmental (Table 3). Intervention components included: (1) evidence-based health education curricula; (2) teacher training and resources on the curricula; (3) establishment of school wellness champions and school district coordinators for MA-CORD; and (4) provision of PA supplies.
Table 3.
MA-CORD Intervention Activities in Public Elementary and Middle Schools
| Student | Teacher | Organizational | Environmental |
|---|---|---|---|
| • Evidence-based curricula—Eat Well Keep Moving and Planet Health—to equip students with knowledge and skills related to the MA-CORD targeted behaviors • Consistent messages on targeted behaviors through posters and educational materials |
• Teacher training and provision of materials for implementing the Eat Well Keep Moving and Planet Health curricula | • Implementation of evidence-based health education curricula with integration of lessons into core subject areas such as math, increasing likelihood of sustainability • Establishment of a district coordinator and at least one staff member per school as the school's wellness champion to support implementation of wellness activities and serve as liaisons to MA-CORD |
• Provision of physical activity supplies to each school to promote increased time in moderate-to-vigorous physical activity • MA-CORD posters and educational materials • Media competition |
MA-CORD, Massachusetts Childhood Obesity Research Demonstration.
The evidence-based curricula—Eat Well Keep Moving24,45 (grades 4–5) and Planet Health17,46 (grades 6–7)—employ lesson plans designed for use by teachers in various disciplines to encourage learning about nutrition, PA, and screen time while building skills in language arts, math, science, and social studies. Planet Health also features Power Down, a 2-week classroom or school-wide campaign to reduce screen time. Teachers in grades 4–7 were trained in the curricula with a focus on delivery of lessons most relevant to the five MA-CORD behaviors. A particular strength of the curricula is that they have been adapted to existing curriculum frameworks. Consequently, once teachers and administrators learn how to implement and integrate lessons into existing practice, there is a greater likelihood for long-term sustainability.
To promote school-wide wellness activities related to the MA-CORD behaviors, the school intervention also included establishing a school district coordinator for MA-CORD in each city and at least one school wellness champion in each school who could link MA-CORD activities with each school's existing wellness plan. District coordinators and school wellness champions received technical assistance through MA-CORD to ensure that wellness activities were carried out and that purchased PA supplies were distributed to schools. They also played a primary role in coordinating the media competition, an intervention with cross-sector linkages between schools and the community described below under Community Activities.
Afterschool Programs
MA-CORD worked with approximately six afterschool programs in each city to implement changes at five levels: student; family; staff; organizational; and environmental/policy. As with the other sectors, representatives from these programs were also part of the local Mass in Motion coalition. Intervention components included: (1) a curriculum to help children develop healthy habits afterschool; (2) a multifaceted organizational change initiative; and (3) learning communities for afterschool programs (Table 4).
Table 4.
MA-CORD Intervention Activities in Afterschool Programs
| Student | Family | Program staff | Organizational | Environmental/policy |
|---|---|---|---|---|
| • Evidence-based Food and Fun curriculum to promote MA-CORD target behaviors • Consistent messages on targeted behaviors through posters and educational materials |
• Food and Fun and OSNAP Initiative parent educational materials on healthy habits • OSNAP guidance and templates for communicating policies to families |
• Staff resources and tools to implement Food and Fun and OSNAP • Learning communities to facilitate communication and problem solving and train directors and staff on developing action plans, setting goals, writing policies, implementing activity breaks, healthy celebrations and fundraising, and staff role modeling |
• Implementation of evidence-based curriculum and organizational change initiative • Practice assessments and development of action plans • Practice changes, such as serving fruits and vegetables at snack |
• Policy self-assessments • Policy writing resources • Development and/or improvement of written policies • Environmental changes, such as availability of cups for water |
MA-CORD, Massachusetts Childhood Obesity Research Demonstration; OSNAP, Out of School Nutrition and Physical Activity Initiative.
MA-CORD afterschool programs implemented Food and Fun Afterschool (FFA), a curriculum for afterschool program staff to use with children ages 5–12 years. FFA includes 11 units with subactivities, parent communications about behaviors at home, and resources for program change.20 Second, the intervention included the Out of School Time Nutrition and Physical Activity (OSNAP) Initiative, which offers resources, skill building, and supports for afterschool programs to make practice, policy, and environmental changes around PA opportunities, foods/beverages, and screen time through program assessments and action planning.47 OSNAP has been shown to be effective at increasing servings of water during afterschool snacks and decreasing calories from beverages.18,48 To train staff and reinforce new concepts acquired through MA-CORD, a series of three learning communities were offered to foster cross-site communication, skill building, and problem solving.
Community Activities
Mass in Motion coalitions in each community incorporated policy, systems and environmental change strategies, activity groups, and media communications designed to reach all of the approximately 18,000 children ages 2–12 in the two cities, as well as their families. The community interventions were adapted for each city by its Mass in Motion municipal wellness coalition, building on existing initiatives and the particular assets and challenges faced by that community. The interventions were intended to change community norms, policies, practices, and aspects of the environment to support and sustain healthy living during the period of the project and be sustainable over the long term.
One key component of the community-level intervention was the use of media. MA-CORD supported a student media competition in the two cities, using a youth empowerment approach. The media competition was implemented to increase awareness of MA-CORD while promoting the target behaviors in each community. Students from elementary and middle school classes and afterschool programs were invited to submit videos, song/rap lyrics, or artwork and were judged on integration of MA-CORD goals, creativity, originality, clarity of message, and utility. Gift cards or prizes were provided to the winning schools, teachers, and students. The competition, including the winning entries, was publicized to the full community on the school district websites and through the Mass in Motion coalitions' communication channels. A student media competition was employed because empowering youth to develop and implement media efforts has positive outcomes, including increased self-efficacy and the development of a stronger sense of responsibility to others, among youth through the production of knowledge that impacts policy and action in their communities.49
A text messaging campaign was implemented to spread the MA-CORD brand and messaging on a larger community scale. The campaign was promoted through purchased advertising space and time in various media channels, including small billboards and transit ads, and handouts for use in community settings. MA-CORD also partnered with the local parks and recreation departments in each community to implement a “summer passport” program in which kids completed activities to earn a small prize.
Another example of a community-level strategy employed by the Mass in Motion coalitions was Safe Routes to School.50 Mass in Motion coalitions worked with local school officials, municipal leaders, community organizations, and a representative of the Massachusetts Department of Transportation's Safe Routes to School program to conduct School Route Analyses and Walkability and Bikeability surveys of the primary routes. The goal was to create a list of short- and long-term improvements—including traffic calming, the creation of traffic-separated cycle tracks, and other “complete streets” attributes—that make parents feel it is safer for their children to walk or bike to school.
Evaluation
MA-CORD will be evaluated using a combination of pre– and post–time series and quasi-experimental designs after the completion of the 2-year intervention in September 2014. A detailed summary of the evaluation of MA-CORD is outlined in Davison and colleagues11 and is summarized briefly below. The MA-CORD evaluation will utilize data from multiple surveillance systems (i.e., electronic health, WIC, and public elementary and middle school records) coupled with supplemental longitudinal survey data for a subsample of individuals from each of those systems. This approach combines the strengths of internal validity gained from a within-person design with those of generalizability gained from surveillance data while making efficient use of pre-existing data-gathering systems and minimizing respondent burden in the intervention and comparison communities.
Within the intervention communities, primary outcome data measuring BMI and the five target behaviors are being collected in the CHC, HWC, WIC, and public elementary and middle schools. Cost-effective analyses are also planned, and supplemental funding will allow for qualitative and quantitative process evaluation to be conducted across sectors. The primary outcome measures include children's BMI, the five behaviors targeted by MA-CORD, children's health-related quality of life, and parent's satisfaction with healthcare services.
Discussion
MA-CORD's innovation is demonstrated through its high level of community coordination and use of multiple interventions that have demonstrated efficacy across various sectors. Further, by using consistent messaging and materials, all sector-wide activities were focused on the same five behavioral targets, which have strong evidence for association with childhood obesity. Emerging evidence indicates that effective and sustainable improvement in population health can be achieved through better integration and partnerships between primary care and community/public health programs.12 Substantial evidence also suggests that single-sector interventions alone may be limited in their effectiveness in reducing childhood obesity. Sustainable changes to shift children's growth trajectories will require coordinated, multisector approaches, such as those being tested in MA-CORD, to impact environmental influences on obesity.10 Such efforts should ideally include cost-effective policy and programmatic interventions across multiple sectors that are feasible and sustainable.9
A major strength of the MA-CORD project was the key role the state's department of public health played in developing the multisector intervention with a specific focus on both sustainability and replicability through existing mechanisms. For example, elements of the WIC intervention found to be effective can be replicated statewide immediately after the study through department policy directives. Similarly, community-level initiatives identified as beneficial can be incorporated into the work plans of the other 49 Mass in Motion communities. The explicit linking of MA-CORD with MDPH strategic priorities ensures the sustainability of its findings.
As with all studies, MA-CORD has limitations. First, given the nature of a multilevel, multisector community intervention, it did not use a randomized or blinded design. Whereas the study was designed to produce fidelity to the evidence-based clinical, school, afterschool, and child care interventions across the two intervention sites, the community-level policy change activities reflected the specific needs and assets of the intervention communities and therefore were not identical. One comparison community was selected as a representative community that matched the community characteristics of Fitchburg and New Bedford as closely as possible. No comparison community could be a perfect match. There was also limited control over what wellness interventions were undertaken by the comparison community during the study period. Further, though we only collected longitudinal behavioral data from one community to serve as a comparison, we were able to compare BMI results with school districts across the state. Despite these limitations, MA-CORD reflects best practice in the design and evaluation of multilevel interventions and will add significantly to the knowledge base in addressing childhood obesity.
Conclusions
MA-CORD implemented a multisector, multilevel intervention to prevent or reduce obesity among underserved children ages 2–12 years in Massachusetts. The study was informed by conceptual frameworks that guide healthcare system changes and aim to reduce the childhood energy gap. If successful, MA-CORD will provide new and sustainable approaches for accelerating the adoption of obesity prevention best practices in clinical and public health systems that serve a socioeconomically diverse population of children.
Contributor Information
Collaborators: the MA-CORD Study Group
Acknowledgments
The authors thank the families, institutions, faculty, research staff, and students that are participating in the MA-CORD study. The following investigators and institutions constitute the MA-CORD Study Group: Massachusetts Department of Public Health: Thomas Land, PhD; Commissioner Cheryl Bartlett, RN; Lea Susan Ojamaa, MPH; Craig Andrade, DrPH; Jo-Ann Kwass, MS; Jaime Corliss, MPH; James Buszkiewicz, MPH; Judy Hause, MPH; Rachel Colchamiro, MPH, RD; Peggy Leung-Strle, MS, RD; Suzanne Crowther, MPH; Donna Salloom. Massachusetts Department of Early Education and Care: Anne Hemmer, RD, MS. Fitchburg Mass in Motion: Mary Giannetti, MS, RD; Pamela Rivers, RN, MPH. New Bedford Mass in Motion: Pauline Hamel, EdD; Kim Ferreira, MS; Sarah Clermont, MPH; Karen Regan, RN, MSN. Massachusetts General Hospital for Children/Harvard Medical School: Elsie M. Taveras, MD, MPH; Meghan Perkins, MPH; Jennifer Woo Baidal, MD, MPH; Lauren Fiechtner, MD, MPH; Courtney Cunningham MPH; Savannah Vicente; Gabriella De Paz. Harvard School of Public Health: Kristen Davison, PhD; Steven Gortmaker, PhD; Walter Willett, MD, DrPH; Lilian Cheung, DSc; Steven Miller; Catherine Giles, MPH; Becky Franckle, MPH; Claudia Gehre, MPH; Rachel Blaine, MPH, RD; Shaniece Criss, MPH. National Initiative for Children's Healthcare Quality: Lauren Smith, MD, MPH; Shikha Anand, MD, MPH; Charles Homer, MD, MPH; Lexi Abel, MPH. MORE Advertising: Megan Palamé, MA. Harvard Pilgrim Health Care Institute: Martin Kuldorff, PhD; Matthew Gillman, MD, SM. University of California, Berkeley: Jennifer Falbe, PhD. Centers for Disease Control and Prevention: Carrie A. Dooyema, MPH, MSN, RN; Brook Belay, MD, MPH; Jennifer L. Foltz, MD, MPH; Nancy Williams, MSPH; Heidi M. Blanck, PhD. University of Houston Evaluation Center: Daniel O'Connor, PhD; Paras Mehta, PhD.
This study was supported by the CDC, National Center for Chronic Disease Prevention and Health Promotion (award no.: U18DP003370). This work is solely the responsibility of the authors and does not represent official views of the CDC. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the listed funding sources. Funding support for S.C. was also provided by predoctoral training grants from the Initiative to Maximize Student Diversity Award (grant no.: GM055353-13), the Maternal and Child Health Bureau (grant no.: T03MC07648), and the National Institutes of Health (grant no.: 3R25CA057711).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Freedman DS, Khan LK, Dietz WH, et al. . Relationship of childhood obesity to coronary heart disease risk factors in adulthood: The Bogalusa Heart Study. Pediatrics 2001;108:712–718 [DOI] [PubMed] [Google Scholar]
- 2.Must A, Strauss RS. Risks and consequences of childhood and adolescent obesity. Int J Obes Relat Metab Disord 1999;23(Suppl 2):S2–S11 [DOI] [PubMed] [Google Scholar]
- 3.Dietz WH. Overweight and precursors of type 2 diabetes mellitus in children and adolescents. J Pediatr 2001;138:453–454 [DOI] [PubMed] [Google Scholar]
- 4.Taveras EM, Rifas-Shiman SL, Camargo CA Jr., et al. . Higher adiposity in infancy associated with recurrent wheeze in a prospective cohort of children. J Allergy Clin Immunol 2008;121:1161–1166e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Madsen KA, Weedn AE, Crawford PB. Disparities in peaks, plateaus, and declines in prevalence of high BMI among adolescents. Pediatrics 2010;126:434–442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olds T, Maher C, Zumin S, et al. . Evidence that the prevalence of childhood overweight is plateauing: Data from nine countries. Int J Pediatr Obes 2011;6:342–360 [DOI] [PubMed] [Google Scholar]
- 7.Institute of Medicine. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. National Academies Press: Washington, DC, 2012 [PubMed] [Google Scholar]
- 8.Foltz JL, May AL, Belay B, et al. . Population-level intervention strategies and examples for obesity prevention in children. Annu Rev Nutr 2012;32:391–415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gortmaker SL, Swinburn BA, Levy D, et al. . Changing the future of obesity: science, policy, and action. Lancet 2011;378:838–847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dooyema CA, Belay B, Foltz JL, et al. . The childhood obesity research demonstration project: A comprehensive community approach to reduce childhood obesity. Child Obes 2013;9:454–459 [DOI] [PubMed] [Google Scholar]
- 11.Davison KK, Falbe J, Taveras EM, et al. . Evaluation overview for the Massachusetts Childhood Obesity Research Demonstration (CORD) study. Child Obes 2015;11:23–36. doi: 10.1089/chi.2014.0059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Institute of Medicine. Primary Care and Public Health: Exploring Integration to Improve Population Health. National Academies Press: Washington, DC, 2012 [PubMed] [Google Scholar]
- 13.Wagner EH. Chronic disease management: What will it take to improve care for chronic illness? Eff Clin Pract 1998;1:2–4 [PubMed] [Google Scholar]
- 14.Wang YC, Gortmaker SL, Sobol AM, et al. . Estimating the energy gap among US children: A counterfactual approach. Pediatrics 2006;118:e1721–e1733 [DOI] [PubMed] [Google Scholar]
- 15.Wang YC, Orleans CT, Gortmaker SL. Reaching the healthy people goals for reducing childhood obesity: Closing the energy gap. Am J Prev Med 2012;42:437–444 [DOI] [PubMed] [Google Scholar]
- 16.Hall KD, Butte NF, Swinburn BA, et al. . Dynamics of childhood growth and obesity: Development and validation of a quantitative mathematical model. Lancet Diabetes Endocrinol 2013;1:97–105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gortmaker SL, Peterson K, Wiecha J, et al. . Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med 1999;153:409–418 [DOI] [PubMed] [Google Scholar]
- 18.Mozaffarian RS, Wiecha JL, Roth BA, et al. . Impact of an organizational intervention designed to improve snack and beverage quality in YMCA after-school programs. Am J Public Health 2010;100:925–932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taveras EM, Gortmaker SL, Hohman KH, et al. . Randomized controlled trial to improve primary care to prevent and manage childhood obesity: The High Five for Kids study. Arch Pediatr Adolesc Med 2011;165:714–722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gortmaker SL, Lee RM, Mozaffarian RS, et al. . Effect of an after-school intervention on increases in children's physical activity. Med Sci Sports Exerc 2012;44:450–457 [DOI] [PubMed] [Google Scholar]
- 21.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice-Hall: Englewood Cliff, NJ, 1986 [Google Scholar]
- 22.Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev 1977;84:191–215 [DOI] [PubMed] [Google Scholar]
- 23.Bandura A. Self-Efficacy Mechanism in Psychological Activation and Health-Promoting Behavior. Raven: New York, 1991 [Google Scholar]
- 24.Gortmaker SL, Cheung LW, Peterson KE, et al. . Impact of a school-based interdisciplinary intervention on diet and physical activity among urban primary school children: Eat well and keep moving. Arch Pediatr Adolesc Med 1999;153:975–983 [DOI] [PubMed] [Google Scholar]
- 25.Massachusetts Department of Public Health, Commonwealth of Massachusetts. Mass in Motion. Available at http://www.mass.gov/eohhs/gov/departments/dph/programs/community-health/mass-in-motion Last accessed May27, 2014
- 26.US Department of Health and Human Services Affordable Care Act (ACA): Childhood obesity research demonstration funding opportunity announcement. Available at http://www.grants.gov/web/grants/view-opportunity.html?oppId=65553 Last accessed May21, 2014
- 27.Epstein LH, Roemmich JN, Robinson JL, et al. . A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children. Arch Pediatr Adolesc Med 2008;162:239–245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Robinson TN. Reducing children's television viewing to prevent obesity: A randomized controlled trial. JAMA 1999;282:1561–1567 [DOI] [PubMed] [Google Scholar]
- 29.Ebbeling CB, Swain JF, Feldman HA, et al. . Effects of dietary composition on energy expenditure during weight-loss maintenance. JAMA 2012;307:2627–2634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mitchell JA, Pate RR, Espana-Romero V, et al. . Moderate-to-vigorous physical activity is associated with decreases in body mass index from ages 9 to 15 years. Obesity (Silver Spring) 2013;21:E280–E293 [DOI] [PubMed] [Google Scholar]
- 31.Taveras EM, Rifas-Shiman SL, Oken E, et al. . Short sleep duration in infancy and risk of childhood overweight. Arch Pediatr Adolesc Med 2008;162:305–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bell JF, Zimmerman FJ. Shortened nighttime sleep duration in early life and subsequent childhood obesity. Arch Pediatr Adolesc Med 2010;164:840–845 [DOI] [PubMed] [Google Scholar]
- 33.Lumeng JC, Somashekar D, Appugliese D, et al. . Shorter sleep duration is associated with increased risk for being overweight at ages 9 to 12 years. Pediatrics 2007;120:1020–1029 [DOI] [PubMed] [Google Scholar]
- 34.Taveras EM, Marshall R, Horan CM, et al. . Rationale and design of the STAR randomized controlled trial to accelerate adoption of childhood obesity comparative effectiveness research. Contemp Clin Trials 2013;34:101–108 [DOI] [PubMed] [Google Scholar]
- 35.Anand SG, Adams WG, Zuckerman BS. Specialized care of overweight children in community health centers. Health Aff (Millwood) 2010;29:712–717 [DOI] [PubMed] [Google Scholar]
- 36.Langley GL, Nolan KM, Nolan TW, et al. . The Improvement Guide: A Practical Approach to Enhancing Organizational Performance, 2nd ed. Jossey-Bass: San Francisco, CA, 2009 [Google Scholar]
- 37.McPherson ME, Mirkin R, Heatherley PN, et al. . Educating health care professionals in advocacy for childhood obesity prevention in their communities: Integrating public health and primary care in the Be Our Voice project. Am J Public Health 2012;102:e37–e43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ayash CR, Simon SR, Marshall R, et al. . Evaluating the impact of point-of-care decision support tools in improving diagnosis of obese children in primary care. Obesity (Silver Spring) 2013;21:576–582 [DOI] [PubMed] [Google Scholar]
- 39.Taveras EM, Marshall R, Horan CM, et al. . Improving children's obesity-related health care quality: Process outcomes of a cluster-randomized controlled trial. Obesity (Silver Spring) 2013;22:27–31 [DOI] [PubMed] [Google Scholar]
- 40.Haines J, McDonald J, O'Brien A, et al. . Healthy Habits, Happy Homes: Randomized trial to improve household routines for obesity prevention among preschool-aged children. JAMA Pediatr 2013;167:1072–1079 [DOI] [PubMed] [Google Scholar]
- 41.Fox MK, Hallgren K, Boller K, et al. . Administration for Children and Familites. Efforts to meet children's physical activity and nutritional needs: Findings from the I Am Moving, I Am Learning Implementation Evaluation. US Department of Health and Human Services: Washington, DC, 2010 [Google Scholar]
- 42.Benjamin SE, Ammerman A, Sommers J, et al. . Nutrition and physical activity self-assessment for child care (NAP SACC): Results from a pilot intervention. J Nutr Educ Behav 2007;39:142–149 [DOI] [PubMed] [Google Scholar]
- 43.Ward DS, Benjamin SE, Ammerman AS, et al. . Nutrition and physical activity in child care: Results from an environmental intervention. Am J Prev Med 2008;35:352–356 [DOI] [PubMed] [Google Scholar]
- 44.Drummond RL, Staten LK, Sanford MR, et al. . A pebble in the pond: The ripple effect of an obesity prevention intervention targeting the child care environment. Health Promot Pract 2009;10(2 Suppl):156S–167S [DOI] [PubMed] [Google Scholar]
- 45.The President and Fellows of Harvard College Eat Well and Keep Moving. Available at http://www.hsph.harvard.edu/prc/projects/eat-well-keep-moving Last accessed May27, 2014
- 46.The President and Fellows of Harvard College Planet Health. Available at http://www.hsph.harvard.edu/prc/projects/planet Last accessed May27, 2014
- 47.The President and Fellows of Harvard College OSNAP. Available at http://osnap.org Last accessed May27, 2014
- 48.Giles CM, Kenney EL, Gortmaker SL, et al. . Increasing water availability during afterschool snack: Evidence, strategies, and partnerships from a group randomized trial. Am J Prev Med 2012;43(3 Suppl 2):S136–S142 [DOI] [PubMed] [Google Scholar]
- 49.Wong NT, Zimmerman MA, Parker EA. A typology of youth participation and empowerment for child and adolescent health promotion. Am J Community Psychol 2010;46:100–114 [DOI] [PubMed] [Google Scholar]
- 50.Boarnet MG, Day K, Anderson C, et al. . California's Safe Routes to School program: Impacts on walking, bicycling, and pedestrian safety. J Am Plann Assoc 2005;71:301–317 [Google Scholar]