Abstract
Infection with human T-lymphotropic virus type 1 (HTLV-1) can be associated with hematologic malignancy, inflammatory syndromes, or infectious complications. Herein, we bring attention to HTLV-1 infection complications as we discuss a case of disseminated cryptococcosis in a patient with HTLV-1-associated T cell lymphoma.
Keywords: Cryptococcus neoformans, human T lymphotropic virus 1, HTLV-1
CASE REPORT
An 82-year-old woman, originally from the Caribbean, presented with fever and hemoptysis. She had no known comorbidities and she was not receiving immunosuppressive agents. A computed tomography of her thorax demonstrated extensive right middle lobe consolidation with satellite nodular lesions. She was treated empirically with piperacillin-tazobactam for necrotizing pneumonia with improvement of her symptoms. Ten days later, she was readmitted to the hospital after developing aphasia and confusion. On examination she was afebrile, obtunded, and she quickly became unresponsive. White blood cell count was 5600/mm3 and CD4+ T cell count was 758 cells/mm3. Human immunodeficiency virus (HIV) type 1 and 2 antibody testing in blood was negative. Lumbar puncture demonstrated normal opening pressure, and cerebrospinal fluid analysis showed 105 white blood cells/mm3, 79% lymphocytes and 17% polymorphonuclear cells, and normal protein and glucose levels. Magnetic resonance imaging of her brain did not show any masses, edema, or hemorrhage. An electroencephalogram revealed high theta activity, compatible with nonconvulsive status epilepticus.
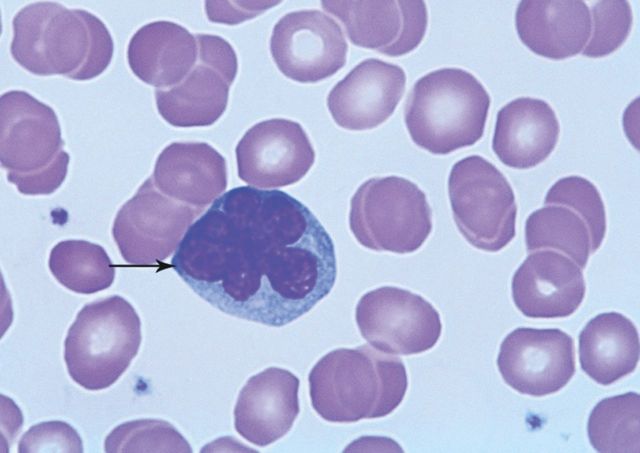
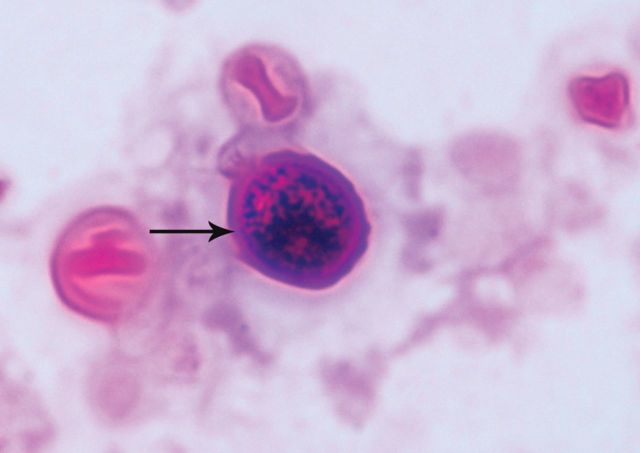
Careful examination of a peripheral blood smear (Figure 1) showed cells with petal-shaped nuclei, known as flower cells, which are frequently, but not exclusively, seen in human T-lymphotropic virus type 1 (HTLV-1) infection or HTLV-1-associated T cell leukemia/lymphoma [1]. Visualization of round yeasts without pseudohyphae on Gram stain from cerebrospinal fluid suggested cryptococcal infection (Figure 2). Serum and cerebrospinal fluid cryptococcal antigens were detected, at titers higher than 1:64; cerebrospinal fluid and bronchoalveolar lavage fluid cultures yielded Cryptococcus neoformans variant neoformans. Human T-lymphotropic virus type 1 antibodies were detected in blood. Flow cytometry immunophenotyping and T cell receptor rearrangement studies from blood were consistent with adult T cell lymphoma. The above results established the diagnosis of disseminated cryptococcosis in the setting of HTLV-1-associated lymphoma. Despite treatment with amphotericin deoxycholate combined with flucytosine, and aggressive supportive care, she had no neurologic recovery and expired after transition to comfort care. Although the reasons for her clinical deterioration despite treatment remain uncertain, it is possible that overwhelming disseminated infection with multiorgan involvement contributed to rapid decline in this immunocompromised host.
Figure 1.
Peripheral blood smear, the arrow is pointing to a flower cell, which is a lymphocyte with petal-shaped nucleus. Flower cells may be seen in the setting of HTLV-1 infection or HTLV-1-associated T cell leukemia/lymphoma.
Figure 2.
Cerebrospinal fluid Gram stain (magnification, x1000). The arrow is indicating an encapsulated yeast. Culture subsequently grew Cryptococcus neoformans.
DISCUSSION
Cryptococcal infection may occur in HIV-infected individuals, organ transplant recipients, or otherwise immunocompromised patients. There are only very rare published reports of invasive cryptococcal disease in patients with HTLV-1-associated T cell leukemia/lymphoma [2]. Overall, cryptococcal disease seems to be a rare complication in HTLV-1-associated leukemia/lymphoma, although a potential association between cryptococcosis and HTLV-1 carrier state has been suggested [3, 4]. Cryptococcus neoformans variant neoformans and predominantly Cryptococcus neoformans variant gattii may also infect seemingly immunocompetent hosts [5]. Clinically, infection with either pathogen manifests similarly [6]. Acquisition occurs via the respiratory route, and pulmonary infection and dissemination to the central nervous system is common. Therefore, in case of pulmonary cryptococcosis in immunosuppressed hosts, it is important to exclude meningitis with lumbar puncture, because the presence of central nervous system disease alters the dose, duration of therapy, and need for intracranial pressure monitoring [7]. In large studies, involving mostly immunocompromised individuals, mortality of cryptococcal meningoencephalitis remains high, up to 20%, despite treatment with antifungal agents [8].
Although Cryptococcus species have a global distribution, HTLV-1 epidemiology has mostly clustered in Japan, sub-Saharan Africa, the Caribbean, and Latin America [9]. Apart from T cell leukemia/lymphoma and inflammatory syndromes, HTLV-1 infection has been associated with infectious complications such as strongyloidiasis, tuberculosis, and leprosy [9]. HTLV-1-associated decrease in type 2 helper T cell response and HTLV-1-associated malignant transformation of T cells are thought to predispose to parasitic infections and abnormal cellular immune responses, respectively [9, 10]. Retroviral coinfection with HTLV and HIV may also lead to increased frequency of HTLV-1-related neurological complications such as myelopathy [11]. Nonetheless, because most HTLV-1-infected individuals remain asymptomatic and T cell counts are normal, there are no established guidelines in monitoring HTLV-1-infected hosts for opportunistic infections. Serological testing, based on epidemiologic suspicion, allows diagnosis and therefore can lead to decreased transmission of the virus, which takes place sexually, as a blood-borne infection, or from mother-to-child through breastfeeding [9]. In addition, knowledge of HTLV-1 infection may raise clinical suspicion for coinfection with another pathogen when HTLV-1-infected individuals seek care [12].
Note
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1.Santos JB, Farre L, Batista Eda S, et al. The importance of flower cells for the early diagnosis of acute adult T-cell leukemia/lymphoma with skin involvement. Acta Oncol. 2010;49:265–7. doi: 10.3109/02841860903428192. [DOI] [PubMed] [Google Scholar]
- 2.Rhew DC, Gaultier CR, Daar ES, et al. Infections in patients with chronic adult T-cell leukemia/lymphoma: case report and review. Clin Infect Dis. 1995;21:1014–6. doi: 10.1093/clinids/21.4.1014. [DOI] [PubMed] [Google Scholar]
- 3.Kohno S, Koga H, Kaku M, et al. Prevalence of HTLV-I antibody in pulmonary cryptococcosis. Tohoku J Exp Med. 1992;167:13–8. doi: 10.1620/tjem.167.13. [DOI] [PubMed] [Google Scholar]
- 4.Debourgogne A, Iriart X, Blanchet D, et al. Characteristics and specificities of Cryptococcus infections in French Guiana, 1998–2008. Med Mycol. 2011;49:864–71. doi: 10.3109/13693786.2011.584198. [DOI] [PubMed] [Google Scholar]
- 5.Kronstad JW, Attarian R, Cadieux B, et al. Expanding fungal pathogenesis: Cryptococcus breaks out of the opportunistic box. Nat Rev Microbiol. 2011;9:193–203. doi: 10.1038/nrmicro2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morgan J, McCarthy KM, Gould S, et al. Cryptococcus gattii infection: characteristics and epidemiology of cases identified in a South African province with high HIV seroprevalence, 2002–2004. Clin Infect Dis. 2006;43:1077–80. doi: 10.1086/507897. [DOI] [PubMed] [Google Scholar]
- 7.Perfect JR, Dismukes WE, Dromer F, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:291–322. doi: 10.1086/649858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dromer F, Mathoulin-Pelissier S, Launay O, Lortholary O. Determinants of disease presentation and outcome during cryptococcosis: the CryptoA/D study. PLoS Med. 2007;4:e21. doi: 10.1371/journal.pmed.0040021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verdonck K, Gonzalez E, Van Dooren S, et al. Human T-lymphotropic virus 1: recent knowledge about an ancient infection. Lancet Infect Dis. 2007;7:266–81. doi: 10.1016/S1473-3099(07)70081-6. [DOI] [PubMed] [Google Scholar]
- 10.Porto AF, Neva FA, Bittencourt H, et al. HTLV-1 decreases Th2 type of immune response in patients with strongyloidiasis. Parasite Immunol. 2001;23:503–7. doi: 10.1046/j.1365-3024.2001.00407.x. [DOI] [PubMed] [Google Scholar]
- 11.Beilke MA, Theall KP, O'Brien M, et al. Clinical outcomes and disease progression among patients coinfected with HIV and human T lymphotropic virus types 1 and 2. Clin Infect Dis. 2004;39:256–63. doi: 10.1086/422146. [DOI] [PubMed] [Google Scholar]
- 12.Xavier RJ, Gala MK, Bronzo BK, Kelly PJ. Case records of the Massachusetts General Hospital. Case 23-2012. A 59-year-old man with abdominal pain and weight loss. N Engl J Med. 2012;367:363–73. doi: 10.1056/NEJMcpc1109275. [DOI] [PubMed] [Google Scholar]