Abstract
Many factors influence the outcomes of reverse shoulder arthroplasty (RSA). The purpose of this study was to compare the clinical and functional outcomes of RSA depending on the surgical approach, type of prosthesis, and indication for surgery through a comprehensive, systematic review.
A literature search was conducted (1985 to June 2012) using PubMed, CINAHL, EBSCO–SPORTDiscus, and Cochrane Central Register of Controlled Trials. Levels I–IV evidence, in-vivo human studies (written in English with minimum of 2 years of follow-up and sample size of 10 patients) reporting clinical and/or functional outcomes after RSA were included. The outcomes were analyzed depending on the surgical approach, type of prosthesis (with medialized or lateralized center of rotation), or indication for surgery.
A total of 35 studies were included involving 2049 patients (mean [SD] percentage of females, age, and follow-up of 71.6% [13.4], 71.5 years [3.7], and 43.1 months [18.8], respectively). Studies using deltopectoral approach with lateralized prostheses demonstrated greater improvement in external rotation compared with medialized prostheses with the same approach (mean 22.9° and 5°, respectively). In general, RSA for cuff tear arthropathy demonstrated higher improvements in Constant and American Shoulder and Elbow Society scores, and range of motion compared with revision of anatomic prosthesis, failed rotator cuff repair, and fracture sequelae.
Lateralized prostheses provided more improvement in external rotation compared to medialized prostheses. Indications of RSA for cuff tear arthropathy demonstrated higher improvements in the outcomes compared with other indications. RSA demonstrated high patient's satisfaction regardless of the type of prosthesis or indication for surgery.
Level of Evidence:
Level IV.
Keywords: Outcomes, reverse shoulder arthroplasty, systematic review
INTRODUCTION
Degenerative joint disease of the shoulder is common worldwide. The definitive treatment option is joint replacement.[1] However, outcomes of anatomic arthroplasty with an osteoarthritic rotator-cuff-deficient shoulder have been limited.[2,3,4] The reverse shoulder arthroplasty (RSA) is a potential solution for shoulder osteoarthritis with deficient rotator cuff.[5,6,7,8,9,10,11] Indications for RSA are expanding.[12,13,14] Theoretical advantages of RSA are an increased lever arm of the deltoid muscle through a medialized center of rotation of the prosthesis (increasing deltoid efficiency), increased prosthetic stabilization through humeral lengthening (increasing deltoid tension), and decreased mechanical torque at the glenoid component (decreasing glenoid loosening).[14,15,16]
There are a huge number of factors influencing the outcomes of RSA.[12,13,15,17,18] These factors are related to the indication for surgery, surgeon's experience, characteristics of the implant, characteristics of the surgical technique, type of approach, or postoperative rehabilitation, among others. Unfortunately, the analysis of outcomes of RSA depending on the type of prosthesis, type of approach, and indication for surgery has not been well reported to date.
The purpose of this study was to compare the clinical and functional outcomes of RSA depending on the surgical approach, type of prosthesis, and indication for surgery through a comprehensive, systematic review of the literature. It was hypothesized that the clinical outcomes would be modified depending on these factors.
MATERIALS AND METHODS
The methodology for this study was reported following the PRISMA statement for systematic review and meta-analysis.[19] All human studies reporting clinical and/or functional outcomes in patients treated with primary or revision RSA were assessed for eligibility. Studies were included if they had a level of evidence between I and IV, were written in English, had a minimum of 2 years of follow-up and had a minimum sample size of 10 patients. Studies reporting complications only, nonoriginal articles, or studies with insufficient outcome data were excluded from this study.
The literature search was based on the PubMed database from 1985 to June 2012. The authors are not aware of any relevant publication related to RSA before 1985, so the search was limited to this period. The keywords and search strategy employed in this study included the following: (Reverse OR inverse) AND shoulder AND (arthroplasty OR replacement OR prosthesis), limited to human studies published in the above-mentioned period. Complementary databases were used to avoid missing an important article for this study. Thus, CINAHL, EBSCO-SPORTDiscus, and the Cochrane Central Register of Controlled Trials were also used to search for relevant publications in the same period. A literature search was performed by one of the authors. Articles of potential interest were reviewed in detail (full text) by two authors and a decision was made regarding inclusion or exclusion. Clinical and functional outcomes were extracted from all included studies in a systematic way using a table template by one author, which was then verified by another author. In cases of disagreement between both authors with regard to study inclusion or data extraction, one of the senior authors made the final decision. A reference list of all included articles was reviewed to search for potential studies not previously identified.
Mean, standard deviation (SD), and range were extracted (whenever provided) in the preoperative and postoperative periods for the following variables: Constant score, American Shoulder and Elbow Society (ASES) score, Simple Shoulder Test, range of motion (ROM), and satisfaction. Furthermore, relevant information regarding level of evidence, type of prosthesis (either with medialized or lateralized center of rotation), type of approach (either deltopectoral or superolateral), indication for RSA, sample size, percentage of females in the sample, follow-up, and age of patients was extracted from all studies.
Descriptive statistics was used to summarize all collected information from the studies. Statistical analyses were performed with SPSS v21 (SPSS Inc., Chicago, IL, USA).
RESULTS
The PubMed search yielded 329 citations, from which 174 were clinical studies in humans that were reviewed in further detail. About 32 met inclusion criteria and additional database searches and review of the reference list from included articles yielded a final number of 35 articles included in the descriptive analysis of clinical outcomes [Figure 1].[5,10,11,17,18,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46] From all 174 articles assessed for eligibility, the senior author had to review four of them because of disagreement between the two authors conducting the systematic review. These two authors had no disagreement on data extraction for the 35 included studies.
Figure 1.
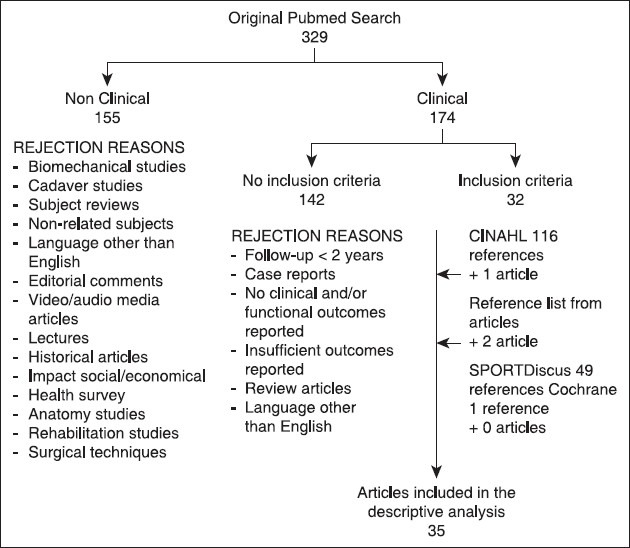
Literature search flow chart
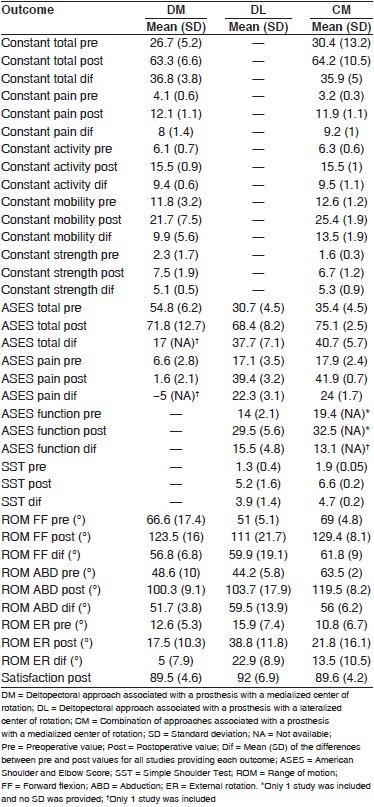
The 35 included studies were grouped depending on the approach and type of prosthesis: Deltopectoral approach associated with prosthesis with a medialized center of rotation (DM group; n = 18 studies), lateralized (DL group; n = 8 studies), and a combination of approaches associated with a medialized prosthesis (CM group; n = 9 studies). The latter group was created because the authors employed different approaches, but clinical outcomes were not specified depending on the type of approach (all these studies employed a prosthesis with a medialized center of rotation). Prostheses with a medialized center of rotation included in this study were the following: Delta III (DePuy, France), Delta Xtend (DePuy, Warsaw, IN, USA), Aequalis (Tornier, France), SMR Modular Shoulder System (Systema Multiplana Randelli, Lima-LTO, San Daniele de Friuli, Italy), and Exactech (Gainesville, FL, USA). Prostheses with a more lateralized center of rotation included in this study were the following: Reverse Shoulder Prosthesis (DJO Surgical, Austin, Texas), and Arrow Anatomical Shoulder System (Mulhouse, France). The 35 studies included a total sample of 2049 patients with a mean (SD) percentage of females of 71.6% (13.4), age of 71.5 years (3.7), and follow-up of 43.1 months (18.8); the respective data separately in groups was, DM, 1085 patients, 73.4% (10.2), 72.4 years (3.1), and 38.1 months (8.2). DL, 241 patients, 69.7% (12.5), 70.1 years (1.7), and 40 months (7.6) and CM group, 723 patients, 73.1% (7.5), 73 years (2.8), and 50.6 months (33.9). Table 1 summarizes the clinical outcomes depending on the approach and type of prosthesis.
Table 1.
Clinical outcomes depending on the type of approach-type of prosthesis
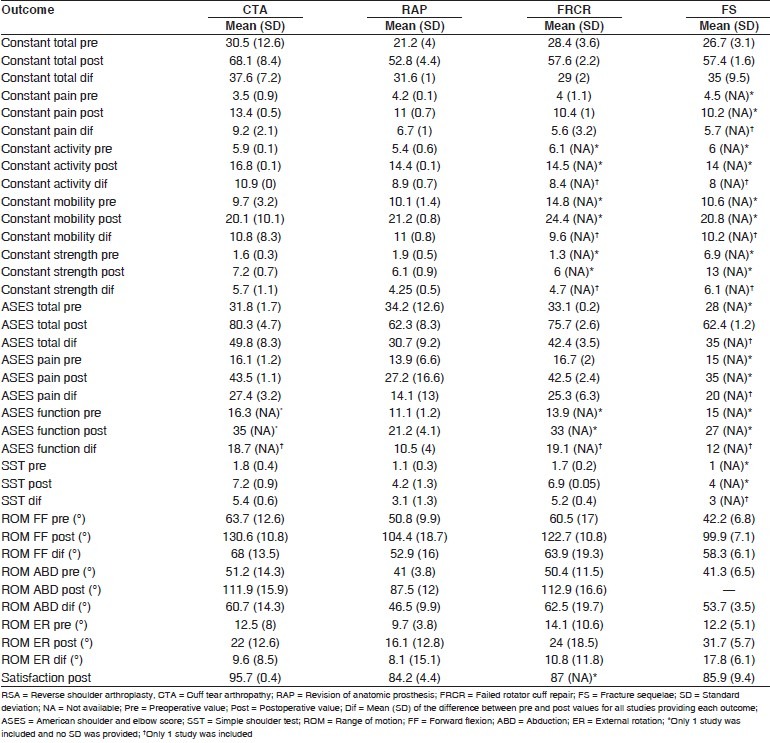
In the analysis of clinical outcomes depending on the indication for RSA, not all 35 studies could be included because results were not always specified by indication. The number of studies included (total subjects involved) by indications for RSA were cuff tear arthropathy 12 (581); revision of anatomic prosthesis 10 (263); failed rotator cuff repair 5 (150); fracture sequelae 4 (82); rheumatoid arthritis 3 (52); massive cuff tear 2 (68); primary osteoarthritis with degenerative cuff tear 2 (51); posttraumatic osteoarthritis 2 (59); and revision of reverse prosthesis 1 (14). Indications of RSA for tumors and acute fractures were not included due to limited data. Mean (SD) for percentage of females, age, and follow-up depending on indications was the following: Cuff tear arthropathy 74% (12), 72.5 years (3.4), and 34.6 months (8), respectively; revision of anatomic prosthesis 66.5% (11.7), 68.2 years (2.7), and 38.2 months (6.6); failed rotator cuff repair 69% (19.8), 69.8 years (3.6), and 39.6 months (11.8); fracture sequelae 70% (8.1), 73.2 years (5.3), and 37.6 months (8.2); and rheumatoid arthritis 87.6% (9.8), 68.2 years (2.9), and 56 months (22.2), respectively. For massive cuff tear, primary osteoarthritis with degenerative rotator cuff, and posttraumatic osteoarthritis only the mean (range) follow-up was provided: 34 months (range 24-118), 38 months (range 24-81), and 42 months (range 24-97), respectively. For revision of reverse prosthesis, percentage of females, and mean (SD) of age and follow-up were 28%, 70.6 years (8.7), and 33 months (11.2), respectively. Table 2 summarizes the clinical outcomes depending on the most common indication for RSA in the included studies.
Table 2.
Clinical outcomes depending on the most common indications for RSA
DISCUSSION
The purpose of this study was to compare the clinical and functional outcomes of RSA depending on the type of prosthesis (with either medialized or lateralized center of rotation), type of approach, and indication for surgery. The principal finding of this study was that both types of prostheses clearly improved the outcomes, but lateralized prostheses had more pre-to-postoperative differences (improvement) for ASES total and pain scores and external rotation compared with medialized prostheses. In addition, outcomes depending on each indication considerably improved, but those corresponding to revision of anatomic prosthesis, failed rotator cuff repair, and fracture sequelae demonstrated lower improvements compared to cuff tear arthropathy. The postoperative patient's satisfaction with surgery was very high (overall mean of 90%) in both types of prostheses and for all indications for surgery.
To the best of our knowledge, this is the first systematic review aimed to investigate the clinical and functional outcomes of RSA depending on the type of prosthesis, type of approach, and an indication for surgery. Khan et al. conducted a comprehensive, systematic review aimed to investigate the outcomes of RSA depending for cuff tear arthropathy, massive cuff tear, and rheumatoid arthritis.[12] However, the authors only included Delta II prostheses and the review included studies up to 2010. The present investigation found many references in the last 2 years and in addition, different type of prostheses, more indications, and a higher number of studies were analyzed. Based on the present study and on the existing literature, RSA is an excellent surgical solution with great improvements in clinical outcomes for cuff tear arthropathy,[5,10,11,12,13,17,22,23,30,36,39,42,47] massive cuff tear,[12,13] 42 failed rotator cuff repair,[11,20,22,36,37] rheumatoid arthritis,[12,27,44,45] fracture sequelae,[5,33,34,43] revision of anatomic prosthesis,[5,11,13,22,28,31,32,35,41,42] and revision of reverse prosthesis.[26] In addition, both types of prostheses demonstrated excellent improvements in the postoperative period with regard to all outcomes. The fact that prostheses with lateralized center of rotation had greater improvement in ASES and external rotation have to be interpreted with caution, as this study had some limitations. First and foremost, a pooled analysis of the results (meta-analysis with inferential statistics) was not possible for methodological reasons, as nearly all studies did not report the SD in the outcomes and an accurate meta-analysis could not be, therefore, conducted. In addition, most of the studies did not disclose the outcomes depending on the indications for surgery, so this parameter had to be considered separately to avoid a significant decrease in the number of studies included in the comparisons of outcomes. Thus, only the type of prosthesis and type of approach could be analyzed altogether. Second, as almost all included studies were case series, the comparison of outcomes depending on the type of prosthesis, approach, and an indication was indirect in nature with a greater potential influence of uncontrolled variables. Third, the influence of several factors potentially influencing the outcomes could not be assessed because of limited information, heterogeneity of studies, and small number of studies included for some comparisons (which would decrease even more the available data if more subgroups were done). Finally, it must be mentioned that the ASES score in medialized prosthesis was only reported by one study,[28] which may decrease the value of the comparison of this parameter between medialized and lateralized prostheses.
It must be first recognized that there are a considerable number of potential factors not controlled in this analysis that may have a potential influence on the outcomes: Different surgeon's experience,[13] different rehabilitation protocols (given the multicentric nature of this study), type (eccentric or concentric) and size of glenosphere,[17,18] location and orientation of the glenosphere and humeral components (inferiorly placed glenosphere, anteversion/retroversion, of the humeral component)[15] degree of fatty infiltration of the teres minor muscle,[5,38] degree of bone stock,[29] soft tissue tensioning,[15] status of the subscapularis muscle, humeral osteotomy angle, or previous surgery.[7,11,36] In addition, no attempt was made to analyze data based on differences in humeral components, medialized versus lateralized, high neck angle versus low neck angle, sit-on-top versus sit inside, and cemented versus uncemented. In the present study, the influence of the type of approach on the outcomes of RSA could not be well determined. Some studies used a combination of approaches, and the outcomes were not specified depending on whether the approach was deltopectoral or superolateral. Therefore, some studies were grouped as CM[10,20,21,22,23,24,25,29,46,48] to refer to studies using a combination of approaches (and a medialized prosthesis). In some ways, differences between groups DM and CM may be explained by differences in the type of approach, as a type of prosthesis in both groups has a medialized center of rotation. However, considering that the CM has a combination of approaches rather than a unique superolateral approach, no clear conclusions can be drawn regarding its influence on the outcomes of RSA. There are some studies that have found that the surgical approach does not have an influence on the outcomes of RSA.[10,40,46] Clearly, further research is needed in this aspect to better elucidate the influence of the type of approach on the outcomes of RSA. Well-designed level I- or II-evidence comparative studies are needed before clear conclusions can be established. Nonetheless, the clinical relevance of this research question (influence of the type of approach) may be questioned, as some surgeons may be forced to adopt a certain approach based on the surgical history of the patient or the characteristics of the patient's disorder itself.
The type of prosthesis (with a medialized or lateralized center of rotation) seems to have a much more relevant influence on the outcomes of RSA. Given that many studies only employed the deltopectoral approach, the type of prosthesis was more easily isolated. Thus, the comparison between DM and DL may show the influence of the center of rotation on the outcomes. Essentially, both groups demonstrated great improvements in outcomes in the postoperative period. Unfortunately, no studies employing a lateralized center of rotation reported the Constant score, so no comparisons were possible between DM and DL for this parameter. In addition, the ASES score was only reported by one study in the DM group[28] so no accurate conclusions can be drawn for this parameter. In contrast, all studies reported the ROM. The only clinically relevant difference in ROM was for external rotation. Specifically, the DL group demonstrated greater improvements in external rotation compared to the DM group. The reasons for lower improvement in external rotation in medialized prostheses have been suggested by Boileau et al.,[5,15] and Grammont and Baulot.[8] A medialized center of rotation may imply that the humeral cup impinges the posterior neck of the scapula when the arm is at the side.[5,15] In addition, as the posterior deltoid theoretically provides some external rotation when coupled with some abduction,[8] the medialization of the center of rotation may decrease the efficacy of the posterior deltoid to assist in the external rotation.[15] Also, the status of the teres minor may influence the degree of external rotation,[5,38] but this variable was not controlled in the vast majority of studies. Boileau et al. conducted an interesting study in which the center of rotation of a medialized prosthesis was lateralized by placing a bone autograft from the humeral head between the base plate and the scapula.[21] This bony lateralization of the center of rotation demonstrated good integration and the authors found 53° of external rotation and a Constant score of 66. Unfortunately, this was a case series and comparisons with medialized prostheses were only conducted based on the existing literature. The disadvantage of metallic, as opposed to bony, lateralization may be the higher torque or shear force applied to the glenoid component, which may lead to a higher rate of glenoid loosening and screw breakage witnessed.[15,49] Therefore, bony lateralization was suggested to provide a benefit to external rotation without the potentially disastrous consequences of metallic lateralization.[21] In a similar way, Valenti et al. reported the outcomes of a lateralized prosthesis and concluded that less medialization of RSA improves external rotation, thus facilitating activities of daily living of older patients.[39] However, the authors did not compare the outcomes with a sample of patients undergoing RSA with a medialized prosthesis, so their conclusion was again based on a comparison with the existing literature. No level I- or II-evidence studies aimed to compare the outcomes of RSA depending on the type of prosthesis were found in the literature.
Most common indications for RSA were cuff tear arthropathy, revision of anatomic prosthesis, failed rotator cuff repair and fracture sequelae. This study shows that the indication for surgery may have an impact on the outcomes of RSA, which is in accordance with the existing literature.[5,7,11,13,22,23,36,37,42] The present study did not specifically assess the influence of primary versus revision surgery. Some authors found that patients with no previous surgery undergoing RSA had higher postoperative scores in ASES (total, pain, and function) and Constant (total and pain) compared to patients with previous surgery.[7,11,22] However, other authors observed no significant differences in the improvement or postoperative values of Constant score, ASES, Simple Shoulder Test, Visual Analogue Scale for pain and function, Oxford Shoulder score, University of California in Los Angeles (UCLA) Shoulder scale, and ROM between patients with and without previous surgery.[10,36,37] For specific indications, the present study demonstrated that cuff tear arthropathy had higher improvements in Constant score (total, pain, and activity), ASES score (total, pain, and function), Simple Shoulder Test, forward flexion, and abduction compared to revision of anatomic prosthesis. Although there were no inferential statistics in the present study, these results are both in agreement and disagreement with previous studies. Boileau et al. found that patients with cuff tear arthropathy had significantly higher improvements in Constant score compared with patients undergoing revision of the prosthesis.[5] The authors found a higher improvement (no P value provided) in ASES score and external rotation in cuff tear arthropathy compared with revision of prosthesis, but no differences (no P value provided) in forward flexion. Regarding the Constant score, Wall et al. found that cuff tear arthropathy and primary osteoarthritis with degenerative rotator cuff had a higher postoperative Constant score (no P value provided) compared to revision of anatomic prosthesis, massive cuff tear, and posttraumatic osteoarthritis.[42] In fact, revision of anatomic prosthesis and posttraumatic osteoarthritis had significantly worse postoperative Constant score compared to the other indications. Regarding ROM, Wall et al. found that patients with cuff tear arthropathy and posttraumatic osteoarthritis had higher improvements (no P value provided) in external rotation compared to revision of prosthesis, massive cuff tear, and primary osteoarthritis with degenerative rotator cuff. For forward flexion, cuff tear arthropathy and revision of anatomic prosthesis had the highest improvement (no P value provided) compared with massive cuff tear, posttraumatic osteoarthritis, and primary osteoarthritis with degenerative rotator cuff.[42] Favard et al. reported a case series in which patients underwent hemiarthroplasty, anatomic total shoulder arthroplasty, or RSA and outcomes were analyzed depending on the indication for surgery.[23] The authors found that the primary osteoarthritis with degenerative rotator cuff and cuff tear arthropathy had a significantly higher improvement of the Constant score compared to rheumatoid arthritis and avascular necrosis. Unfortunately, the number of RSA in the groups of primary osteoarthritis with degenerative rotator cuff, rheumatoid arthritis, and avascular necrosis was 2, 6, and 0, respectively. Therefore, the significant differences are likely explained by anatomic prostheses instead of RSA. Similarly, Walch et al. found that cuff tear arthropathy, primary osteoarthritis with degenerative rotator cuff, and massive cuff tear had significantly higher improvement of the Constant score compared with the revision of the prosthesis and posttraumatic osteoarthritis.[13]
Based on the present study, several recommendations for further research may be elaborated. There is a clear need for future studies specifically comparing the use of medialized and lateralized RSA, as the present comparison was indirect in nature given that no comparative studies of this parameter have been published to date. Further clarification is needed to know to which extent there are significant differences in functional outcomes as well as in external rotation between both models. It is probable that differences on the implanted humeral side may have profound outcome implications, yet there has been no focus on this side of the joint in RSA outcome studies. In addition, the exact impact of the type of approach on the outcomes needs to be better delineated. In any further study utilizing more than one approach and type of prosthesis, the analysis of outcomes needs to be specified depending on both parameters. Furthermore, as the results of RSA may differ depending on the indications for surgery, disclosure of outcomes for indications is also warranted. Finally, there are two methodological recommendations regarding the presentation of studies to facilitate further meta-analyses. First, it is important from a methodological and statistical point of view to report the SD in all parameters collected. Second, further studies would have to use similar outcome-measurement tools. Most studies employing prostheses with medialized center of rotation used the Constant score, whereas studies utilizing lateralized prostheses used the ASES score. Other investigations employed the Simple Shoulder Test, the Oxford Shoulder score, or the UCLA Shoulder scale. This heterogeneity of outcome-measurement tools makes inter-study comparisons highly difficult. Only ROM is systematically provided in the published studies, but more homogeneity is required to facilitate further meta-analyses.
CONCLUSIONS
Both types of prostheses (with medialized and lateralized center of rotation) clearly improved all the reported outcomes, but lateralized prostheses had more improvement in external rotation compared to medialized prostheses. All outcomes of RSA implanted for all types of indications significantly improved in the postoperative period, but those corresponding to revision of anatomic prosthesis, failed rotator cuff repair, and fracture sequelae demonstrated lower improvements compared with cuff tear arthropaty. The RSA is a surgical procedure with high patient satisfaction regardless of the type of prosthesis or the indication for surgery.
DISCLOSURE STATEMENT
There is no conflict of interest or financial aid from any organization regarding the material discussed in the manuscript. Prof. Thomas W. Wright, M.D. is a consultant for Exactech, Inc., Gainesville, Florida, and receives royalties and Institutional research support on products cited to this article.
ACKNOWLEDGMENT
The authors would like to thank Sergi Mojal, PhD, for his methodological and statistical contributions.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Singh JA, Sperling J, Buchbinder R, McMaken K. Surgery for shoulder osteoarthritis: A Cochrane systematic review. J Rheumatol. 2011;38:598–605. doi: 10.3899/jrheum.101008. [DOI] [PubMed] [Google Scholar]
- 2.Cofield RH. Total shoulder arthroplasty with the Neer prosthesis. J Bone Joint Surg Am. 1984;66:899–906. doi: 10.2106/00004623-198466060-00010. [DOI] [PubMed] [Google Scholar]
- 3.Neer CS, 2nd, Craig EV, Fukuda H. Cuff-tear arthropathy. J Bone Joint Surg Am. 1983;65:1232–44. [PubMed] [Google Scholar]
- 4.Neer CS, 2nd, Watson KC, Stanton FJ. Recent experience in total shoulder replacement. J Bone Joint Surg Am. 1982;64:319–37. [PubMed] [Google Scholar]
- 5.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer award 2005: The grammont reverse shoulder prosthesis: Results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006;15:527–40. doi: 10.1016/j.jse.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Boulahia A, Edwards TB, Walch G, Baratta RV. Early results of a reverse design prosthesis in the treatment of arthritis of the shoulder in elderly patients with a large rotator cuff tear. Orthopedics. 2002;25:129–33. doi: 10.3928/0147-7447-20020201-16. [DOI] [PubMed] [Google Scholar]
- 7.Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, Vasey M. The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients. J Bone Joint Surg Am. 2005;87:1697–705. doi: 10.2106/JBJS.D.02813. [DOI] [PubMed] [Google Scholar]
- 8.Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics. 1993;16:65–8. doi: 10.3928/0147-7447-19930101-11. [DOI] [PubMed] [Google Scholar]
- 9.Grammont PM, Trouilloud P, Laffay J, Deries X. Study of the performance of a new shoulder prosthesis. Rhumatologie. 1987;39:407–18. [Google Scholar]
- 10.Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86:388–95. doi: 10.1302/0301-620x.86b3.14024. [DOI] [PubMed] [Google Scholar]
- 11.Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87:1476–86. doi: 10.2106/JBJS.D.02342. [DOI] [PubMed] [Google Scholar]
- 12.Khan WS, Longo UG, Ahrens PM, Denaro V, Maffulli N. A systematic review of the reverse shoulder replacement in rotator cuff arthropathy, rotator cuff tears, and rheumatoid arthritis. Sports Med Arthrosc. 2011;19:366–79. doi: 10.1097/JSA.0b013e318224e44e. [DOI] [PubMed] [Google Scholar]
- 13.Walch G, Bacle G, Lädermann A, Nové-Josserand L, Smithers CJ. Do the indications, results, and complications of reverse shoulder arthroplasty change with surgeon's experience? J Shoulder Elbow Surg. 2012;21:1470–7. doi: 10.1016/j.jse.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 14.Zumstein MA, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: A systematic review. J Shoulder Elbow Surg. 2011;20:146–57. doi: 10.1016/j.jse.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 15.Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: Design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005;14:147S–61. doi: 10.1016/j.jse.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 16.Walker M, Brooks J, Willis M, Frankle M. How reverse shoulder arthroplasty works. Clin Orthop Relat Res. 2011;469:2440–51. doi: 10.1007/s11999-011-1892-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Biase CF, Delcogliano M, Borroni M, Castagna A. Reverse total shoulder arthroplasty: Radiological and clinical result using an eccentric glenosphere. Musculoskelet Surg. 2012;96(Suppl 1):S27–34. doi: 10.1007/s12306-012-0193-4. [DOI] [PubMed] [Google Scholar]
- 18.Mizuno N, Denard PJ, Raiss P, Walch G. The clinical and radiographical results of reverse total shoulder arthroplasty with eccentric glenosphere. Int Orthop. 2012;36:1647–53. doi: 10.1007/s00264-012-1539-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med. 2009;151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 20.Boileau P, Gonzalez JF, Chuinard C, Bicknell R, Walch G. Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg. 2009;18:600–6. doi: 10.1016/j.jse.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 21.Boileau P, Moineau G, Roussanne Y, O'Shea K. Bony increased-offset reversed shoulder arthroplasty: Minimizing scapular impingement while maximizing glenoid fixation. Clin Orthop Relat Res. 2011;469:2558–67. doi: 10.1007/s11999-011-1775-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cuff D, Pupello D, Virani N, Levy J, Frankle M. Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency. J Bone Joint Surg Am. 2008;90:1244–51. doi: 10.2106/JBJS.G.00775. [DOI] [PubMed] [Google Scholar]
- 23.Favard L, Katz D, Colmar M, Benkalfate T, Thomazeau H, Emily S. Total shoulder arthroplasty-arthroplasty for glenohumeral arthropathies: Results and complications after a minimum follow-up of 8 years according to the type of arthroplasty and etiology. Orthop Traumatol Surg Res. 2012;98:S41–7. doi: 10.1016/j.otsr.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 24.Favard L, Levigne C, Nerot C, Gerber C, De Wilde L, Mole D. Reverse prostheses in arthropathies with cuff tear: Are survivorship and function maintained over time? Clin Orthop Relat Res. 2011;469:2469–75. doi: 10.1007/s11999-011-1833-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grassi FA, Murena L, Valli F, Alberio R. Six-year experience with the Delta III reverse shoulder prosthesis. J Orthop Surg (Hong Kong) 2009;17:151–6. doi: 10.1177/230949900901700205. [DOI] [PubMed] [Google Scholar]
- 26.Holcomb JO, Cuff D, Petersen SA, Pupello DR, Frankle MA. Revision reverse shoulder arthroplasty for glenoid baseplate failure after primary reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18:717–23. doi: 10.1016/j.jse.2008.11.017. [DOI] [PubMed] [Google Scholar]
- 27.Holcomb JO, Hebert DJ, Mighell MA, Dunning PE, Pupello DR, Pliner MD, et al. Reverse shoulder arthroplasty in patients with rheumatoid arthritis. J Shoulder Elbow Surg. 2010;19:1076–84. doi: 10.1016/j.jse.2009.11.049. [DOI] [PubMed] [Google Scholar]
- 28.Kelly JD, 2nd, Zhao JX, Hobgood ER, Norris TR. Clinical results of revision shoulder arthroplasty using the reverse prosthesis. J Shoulder Elbow Surg. 2012;21:1516–25. doi: 10.1016/j.jse.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 29.Klein SM, Dunning P, Mulieri P, Pupello D, Downes K, Frankle MA. Effects of acquired glenoid bone defects on surgical technique and clinical outcomes in reverse shoulder arthroplasty. J Bone Joint Surg Am. 2010;92:1144–54. doi: 10.2106/JBJS.I.00778. [DOI] [PubMed] [Google Scholar]
- 30.Leung B, Horodyski M, Struk AM, Wright TW. Functional outcome of hemiarthroplasty compared with reverse total shoulder arthroplasty in the treatment of rotator cuff tear arthropathy. J Shoulder Elbow Surg. 2012;21:319–23. doi: 10.1016/j.jse.2011.05.023. [DOI] [PubMed] [Google Scholar]
- 31.Levy J, Frankle M, Mighell M, Pupello D. The use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty for proximal humeral fracture. J Bone Joint Surg Am. 2007;89:292–300. doi: 10.2106/JBJS.E.01310. [DOI] [PubMed] [Google Scholar]
- 32.Levy JC, Virani N, Pupello D, Frankle M. Use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty in patients with glenohumeral arthritis and rotator cuff deficiency. J Bone Joint Surg Br. 2007;89:189–95. doi: 10.1302/0301-620X.89B2.18161. [DOI] [PubMed] [Google Scholar]
- 33.Martinez AA, Bejarano C, Carbonel I, Iglesias D, Gil-Alvaroba J, Herrera A. The treatment of proximal humerus nonunions in older patients with the reverse shoulder arthroplasty. Injury. 2012;43(Suppl 2):S3–6. doi: 10.1016/S0020-1383(13)70172-4. [DOI] [PubMed] [Google Scholar]
- 34.Martinez AA, Calvo A, Bejarano C, Carbonel I, Herrera A. The use of the Lima reverse shoulder arthroplasty for the treatment of fracture sequelae of the proximal humerus. J Orthop Sci. 2012;17:141–7. doi: 10.1007/s00776-011-0185-5. [DOI] [PubMed] [Google Scholar]
- 35.Melis B, Bonnevialle N, Neyton L, Lévigne C, Favard L, Walch G, et al. Glenoid loosening and failure in anatomical total shoulder arthroplasty: Is revision with a reverse shoulder arthroplasty a reliable option? J Shoulder Elbow Surg. 2012;21:342–9. doi: 10.1016/j.jse.2011.05.021. [DOI] [PubMed] [Google Scholar]
- 36.Mulieri P, Dunning P, Klein S, Pupello D, Frankle M. Reverse shoulder arthroplasty for the treatment of irreparable rotator cuff tear without glenohumeral arthritis. J Bone Joint Surg Am. 2010;92:2544–56. doi: 10.2106/JBJS.I.00912. [DOI] [PubMed] [Google Scholar]
- 37.Sadoghi P, Vavken P, Leithner A, Hochreiter J, Weber G, Pietschmann MF, et al. Impact of previous rotator cuff repair on the outcome of reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2011;20:1138–46. doi: 10.1016/j.jse.2011.01.013. [DOI] [PubMed] [Google Scholar]
- 38.Simovitch RW, Helmy N, Zumstein MA, Gerber C. Impact of fatty infiltration of the teres minor muscle on the outcome of reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2007;89:934–9. doi: 10.2106/JBJS.F.01075. [DOI] [PubMed] [Google Scholar]
- 39.Valenti P, Sauzières P, Katz D, Kalouche I, Kilinc AS. Do less medialized reverse shoulder prostheses increase motion and reduce notching? Clin Orthop Relat Res. 2011;469:2550–7. doi: 10.1007/s11999-011-1844-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Walch G, Mottier F, Wall B, Boileau P, Molé D, Favard L. Acromial insufficiency in reverse shoulder arthroplasties. J Shoulder Elbow Surg. 2009;18:495–502. doi: 10.1016/j.jse.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 41.Walker M, Willis MP, Brooks JP, Pupello D, Mulieri PJ, Frankle MA. The use of the reverse shoulder arthroplasty for treatment of failed total shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21:514–22. doi: 10.1016/j.jse.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 42.Wall B, Nové-Josserand L, O'Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: A review of results according to etiology. J Bone Joint Surg Am. 2007;89:1476–85. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- 43.Willis M, Min W, Brooks JP, Mulieri P, Walker M, Pupello D, et al. Proximal humeral malunion treated with reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21:507–13. doi: 10.1016/j.jse.2011.01.042. [DOI] [PubMed] [Google Scholar]
- 44.Woodruff MJ, Cohen AP, Bradley JG. Arthroplasty of the shoulder in rheumatoid arthritis with rotator cuff dysfunction. Int Orthop. 2003;27:7–10. doi: 10.1007/s00264-002-0406-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Young AA, Smith MM, Bacle G, Moraga C, Walch G. Early results of reverse shoulder arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg Am. 2011;93:1915–23. doi: 10.2106/JBJS.J.00300. [DOI] [PubMed] [Google Scholar]
- 46.Young SW, Everts NM, Ball CM, Astley TM, Poon PC. The SMR reverse shoulder prosthesis in the treatment of cuff-deficient shoulder conditions. J Shoulder Elbow Surg. 2009;18:622–6. doi: 10.1016/j.jse.2009.01.017. [DOI] [PubMed] [Google Scholar]
- 47.Sadoghi P, Leithner A, Vavken P, Hölzer A, Hochreiter J, Weber G, et al. Infraglenoidal scapular notching in reverse total shoulder replacement: A prospective series of 60 cases and systematic review of the literature. BMC Musculoskelet Disord. 2011;12:101. doi: 10.1186/1471-2474-12-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Melis B, DeFranco M, Lädermann A, Molé D, Favard L, Nérot C, et al. An evaluation of the radiological changes around the Grammont reverse geometry shoulder arthroplasty after eight to 12 years. J Bone Joint Surg Br. 2011;93:1240–6. doi: 10.1302/0301-620X.93B9.25926. [DOI] [PubMed] [Google Scholar]
- 49.Harman M, Frankle M, Vasey M, Banks S. Initial glenoid component fixation in “reverse” total shoulder arthroplasty: A biomechanical evaluation. J Shoulder Elbow Surg. 2005;14:162S–67. doi: 10.1016/j.jse.2004.09.030. [DOI] [PubMed] [Google Scholar]


