The following text summarises the National Institute for Health and Clinical Excellence (NICE) clinical guidelines (CG 147)1 on the diagnosis and management of lower limb peripheral arterial disease (PAD). With the increasing prevalence of obesity, hypertension, and dyslipidaemia, the more severe cardiovascular complications of such disorders are becoming increasingly common, including PAD. There is, therefore, a need to establish the most efficient and effective methods of diagnosis, treatment, and long-term management to tackle this issue.
Population based studies have found that approximately 20% of people over 60-years-old have some degree of PAD, presenting predominantly with symptoms of intermittent claudication.2 Approximately 20% of these will progress to develop more severe symptoms1 with the risk of critical limb ischaemia, irreversible damage, and the possible need for surgical intervention and eventually even amputation. Therefore, PAD and its sequalae are going to be encountered by virtually every healthcare professional, and a sufficient understanding of the pathology, its diagnosis, and management is crucial.
These guidelines (CG 147) target healthcare professionals responsible for diagnosing and initiating treatment in people with suspected or diagnosed PAD. It addresses methods of diagnosis, information requirements, and lifestyle advice for the prevention of cardiovascular disease secondary to PAD, management of intermittent claudication and critical limb ischaemia, and the role of amputation in severe PAD. In particular, it discusses the progression of management from non-invasive lifestyle advice and exercise, to pharmacotherapy, minimally invasive procedures such as angioplasty and stenting, and finally surgical procedures such as bypass and amputation.
Overall Recommendations
Prompt diagnosis of PAD is crucial in reducing the risk of complications and adverse events, such as critical limb ischaemia, and the need for limb amputation. The hierarchy of management for the main symptom of intermittent claudication begins with lifestyle interventions aimed at improving walking distance and reducing cardiovascular risk, in particular by undertaking supervised exercise. Vasoactive drugs can be administered if exercise leads to insufficient benefit, followed by angioplasty with or without stenting, and bypass surgery depending on comorbidity and overall risk vs. benefit. Endovascular intervention and bypass are also used in the management of critical limb ischaemia. Sufficient pain control is necessary for ischaemic pain in critical limb ischaemia, preferably by reperfusion of the limb, or by using analgesic medications if this isn’t feasible or is unsuccessful. Amputation may be considered in those with severe chronic limb ischaemia with rest pain, tissue ulceration, gangrene, or infection. However, treatment in all patients with chronic limb ischaemia should be on the guidance of the vascular multidisciplinary team.
Information Requirements for People with Peripheral Arterial Disease
Individuals with PAD require relevant information (oral and written) regarding their condition, treatment and disease progression, to guide and support them in making informed decisions about available therapeutic interventions and to enable their understanding of the disease progression. Based on four qualitative studies (n = 131),3–6 NICE recommends that information on the cause, severity, associated risks, risk factors, pain management, treatment options, and psychosocial support should be available at diagnosis and subsequently as requested.
Secondary Prevention of Cardiovascular Disease in People with PAD
PAD is strongly associated with cardiovascular disease, sharing its modifiable and non-modifiable risk facts - the severity of which is a prognostic indicator of cardiovascular risk. However, even asymptomatic individuals with PAD are at a higher risk of further cardiovascular events such as stroke and myocardial infarction. Therefore, the main focus of treatment is that of reducing cardiovascular risk by targeting established risk factors.
Smoking
Smoking is the most the most important risk factor for PAD development. The excess cardiovascular risk is halved within one year of cessation and is the same as non-smokers within five years in those who give up.1 Smoking cessation advice when combined with nicotine replacement therapy improves cessation rates to approximately 30%.1
Diabetes
The incidence and prevalence of PAD increases in diabetics; often complicated with a later presentation, more extensive disease, greater risk of infection, and need for amputation.7,8 There are no studies assessing the effect of glycaemic control and PAD but there is evidence that glycaemic control influences cardiovascular disease progression.9
Dyslipidaemia
There is substantial evidence establishing the benefits of lowering cholesterol with PAD. In the Heart Protection Study,10 PAD patients with total cholesterol >3.5 mmol/L taking simvastatin had a 17.6% reduction in cardiovascular events compared with placebo. Patients with PAD should be considered for statin therapy that may reduce cholesterol levels, as well as causing stabilisation and regression of existing atheromatous plaques at high doses.
Hypertension
High blood pressure is associated with a three-fold increase in PAD and overall cardiovascular risk. Anti-hypertensive treatment, such as ACE inhibitors, have been found to have significant benefit on cardiovascular deaths.11 It is recommended that people with PAD and hypertension should be considered for ACE inhibitor therapy unless they have concomitant contra-indications for such therapy. However, there is not enough evidence for ACE inhibitor use in non-hypertensive patients.
Anti-platelet agents
Antithrombotic Trialists’ collaboration meta-analysis8 found antiplatelet therapy reduced cardiovascular risk by 23% in people with PAD, with 75 mg of aspirin as effective as high doses. Clopidigrel should be used in those with contraindications for non-steroidal anti-inflammatory drug use or aspirin resistance, which has been found to have a relative risk reduction of 8.7% compared with aspirin.
Weight management and exercise
There is proven cardiovascular risk benefit with appropriate weight management and exercise regimens, with additional benefits on intermittent claudication and on other cardiovascular risk factors such as on blood pressure and lipid levels.
Diagnosis
Those people with symptoms suggestive of PAD, diabetes, non-healing leg or feet wounds, unexplained leg pain, those being considered for leg or foot intervention, or those using compression hosiery should be assessed for PAD. Diagnosis is initially made based on a history of leg pain on exertion, with or without additional foot and leg symptoms such as rest pain, ulcers, and tissue loss. It can also be an incidental finding in asymptomatic people attending for a general examination or diabetic foot screening. Accurate diagnosis is crucial to allow timely specialist referral and improve patient outcome, and can be diagnosed via the patient history of intermittent claudication and of symptoms of critical limb ischaemia, leg and feet examination, peripheral pulse examination, the ankle brachial pressure index (ABPI; Fig. 1; <0.9 is an indicator of PAD) and some imaging modalities not discussed in these guidelines.
Fig. 1.
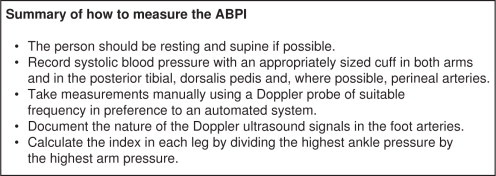
Summary of how to measure the ankle brachial pressure index (ABPI). Information obtained from NICE guidelines on peripheral arterial disease (GC 147).1
Imaging for Revascularisation
The extent of disease and location of any stenosis or occlusion in the legs will determine the treatment pathway for revascularisation. Available modalities include duplex ultrasound scanning (DUS), magnetic resonance angiography (MRA), computed tomography angiography (CTA), and digital subtraction angiography (DSA). DUS and MRA offer the least invasive options and avoid the use of ionising radiation. DUS also offers the advantage of functional assessment of arterial stenosis but is the most operator dependent. The recommendations for assessing revascularisation treatment are to offer DUS as first-line imaging, followed by contrast-enhanced MRA if needed, and CTA if MRA is contraindicated.
Management of Intermittent Claudication
Intermittent claudication is a tight, cramp-like pain the calf muscles, thigh or buttock, which comes on exertion and relieved by resting, and is due to diminished circulation. The most appropriate treatment for intermittent claudication is based on the impact of the symptoms and their person's quality of life, and may include exercise, pharmacotherapy, endovascular interventions, or bypass surgery.
Role of exercise
Exercise has been shown to be beneficial with established cardiovascular disease and can improve walking distance with intermittent claudication.12 Supervised exercise should be offered to all with intermittent claudication, consisting of two hours of supervised exercise a week for a three-month period, and people encouraged to exercise to the point of maximal pain. However, it is acknowledged that even though this is cost effective, there is geographical variability in terms of access to services.
Role of naftidrofurul oxalate
There are a number of vasoactive drugs for intermittent claudication, with evidence that these can increase walking distance in those with PAD.13 The NICE technology appraisal (TA 223) on “Cilostazol, naftidrofuryl oxalate, pentoxifylline and inositol nicotinate for the treatment of IC in people with PAD”13 recommended naftidrofuryl oxalate as the preferred treatment. However, it is still unclear how effective this is when compared to other treatments such as exercise and angioplasty when patients are suitable for more than one option. Also, there is no evidence as to whether there is an identifiable subgroup of people with intermittent claudication that are likely to benefit from drug therapy. It is recommended that clinicians consider naftidrofuryl oxalate for treating people with intermittent claudication, starting with the least costly preparation, only when supervised exercise has been unsatisfactory and the patient prefers not to be referred for endovascular intervention or surgery. Patients taking this medication should be reviewed after 3–6 months, and therapy discontinued if there has been no symptomatic benefit.
Endovascular techniques
Angioplasty with or without stenting can be indicated if there is insufficient symptom control after cardiovascular risk prevention methods have been implemented. Angioplasty is now minimally invasive, but is limited in that in may cause insufficient vessel dilatation or it may lead to complications such as dissection or embolisation. Angioplasty is recommended only after the benefits of modifying risk factors has been reinforced, supervised exercise has not led to satisfactory improvement, and imaging has confirmed that angioplasty is a suitable option for revascularisation.
Stenting can also be used to improve the results of angioplasty, increasing the diameter of the treated artery and preventing or treating complications. It may also alter the risk of long-term re-stenosis and re-occlusion. Stenting can be either primary or secondary (with angioplasty), with primary stenting only recommended for complete aorto-iliac occlusive disease. Based on one randomised controlled trial, it is also recommended that bare metal stents be used over drug-eluting stents when stenting for intermittent claudication.14 There is no strong evidence of a difference in clinical outcomes between bare metal and drug-eluting stents, however using bare metal stents is more cost effective.
Bypass surgery
Bypass surgery can be considered to improve limb circulation if the person is either not suitable for other treatment or has not responded. Autologous vein sampling is less likely to cause infection or serious adverse reaction than prostheses, but such suitable veins may not be available. The valves in the vein mean that the vein either needs to be completely removed and reversed, thereby needing a longer incision, or needs to have a procedure to destroy the valves with subsequent risk of endothelial damage and complications such as restenosis. It is recommended that bypass surgery be offered for treating people with severe lifestyle-limiting intermittent claudication, only when angioplasty has been unsuccessful or is unsuitable, and imaging has confirmed that bypass surgery is appropriate for the person. Based on two randomised controlled trials, it is recommended that an autologous vein be used whenever possible for people with intermittent claudication having infra-inguinal bypass surgery.15,16
Management of Critical Limb Ischaemia
People with critical limb ischaemia face enormous cardiovascular risk, with a 50% mortality rate within the first year of diagnosis. These tend to be older patients with significant comorbidity, which also need to be optimised to reduce this risk. Such patients require prompt referral to specialist services for revascularisation assessment. People with critical limb ischaemia should be encouraged to manage their cardiovascular disease via secondary prevention, as previously discussed. Options for revascularisation include angioplasty or bypass surgery, similarly to that of intermittent claudication. Amputation may need to be considered if revascularisation is not possible or not successful. All people with critical limb ischaemia need to be assessed by a vascular multidisciplinary team, who should be heavily involved in all treatment decision-making.
Angioplasty compared to bypass surgery
It is recommended that either angioplasty or bypass surgery be offered for those requiring revascularisation, depending on their comorbidities, pattern of disease, availability of a suitable vein, and patient preference. There is no clear guidance to determine whether angioplasty or bypass surgery should be employed for revascularisation in critical limb ischaemia, and hence all cases should be considered on an individual basis.
Angioplasty with selective stenting compared to primary stenting
It is recommended that primary stent placement should not be offered when for treating people with chronic limb ischaemia caused by aorto-iliac disease (except complete occlusion) or femoro-popliteal disease, due to the extra cost of routinely employing stents.
Bare metal compared to drug-eluting stents
The use of bare metal stents, rather than drug-eluting stents, when stenting is recommended for treating people with critical limb ischaemia. This is based only on economic benefits, with no clinical evidence for any difference in clinical benefit.
Autologous vein compared to prosthetic bypass
It is recommended than autologous veins are used whenever possible for people with critical limb ischaemia having infra-inguinal bypass surgery. However, there is no clearly established benefit when compared to prosthetic grafts. This recommendation is, therefore, based on the superiority of autologous vein grafts in terms of amputation rate and a non-significant trend in re-intervention rates.
Management of Ischaemic Pain in Critical Limb Ischaemia
Severe and persistent pain is one of the associated features of critical limb ischaemia due to poor tissue perfusion and subsequent tissue loss and ulceration. The preferred therapeutic intervention is that which will improve tissue perfusion either endovascularly or surgically. However, if such intervention is unsuccessful, analgesics can be administered. It is recommended that initially, paracetamol and opioids be offered depending on the severity of pain, along with laxatives and anti-emetics to manage any adverse effects of strong opioids. People should be referred to a specialist pain management service if their pain is not adequately controlled, they are requiring on-going high doses of opioids, or the pain persists after revascularisation or amputation.
Major Amputation for Critical Limb Ischaemia
Amputations are offered in PAD patients with severe critical limb ischaemia, often when associated with ischaemic rest pain and/or tissue loss (ulceration and gangrene) and infection that cannot be medically controlled. A multidisciplinary team of vascular specialists must also deem that the blood supply to the leg cannot be restored via angioplasty or bypass. Rarely, emergency amputations are undertaken due to overwhelming infection. However, for the majority of cases they are only performed after a full discussion of the risks and benefits of all treatment options with the patient and family. It is recommended that major amputations are not offered to people with critical limb ischaemia unless all options for revascularisation have been considered by a vascular multidisciplinary team. This is deemed a key priority for implementation to prevent people having amputations for a disease that could be treated if all possible options for management were considered by a multidisciplinary team.
Conclusions
After discussing the treatment options with the patient, management of PAD should firstly focus on lifestyle interventions, before the vascular multidisciplinary team are involved who need to be crucially involved in interventional therapy, namely the need for angioplasty or bypass surgery. Prompt diagnosis of PAD is crucial in reducing the risk of complications and adverse events such as critical limb ischaemia. Amputation may be considered in those with severe chronic limb ischaemia with rest pain, tissue ulceration, gangrene, or infection. However, treatment in all patients with chronic limb ischaemia should be on the guidance of the vascular multidisciplinary team.
Ethical approval
No ethical approval required for this study.
Conflicts of interest
No conflicts of interest have been declared by the author.
Author contributions
Single author manuscript.
Funding
No funding source declared by the author.
Footnotes
Provenance and Peer Review
Commissioned and Editorial Review
References
- 1.National Institute for Health and Clinical Excellence. Lower limb pripheral arterial disease: diagnosis and management. NICE Clinical Guideline 147. 2012 [online]. http://www.nice.org.uk/nicemedia/live/13856/60426/60426.pdf. (Accessed 5 Dec 2012).
- 2.Fowkes F.G.R., Housley E., Cawood E.H.H., Macintyre C.C.A., Ruckley C.V., Prescott R.J. Edinburgh artery study: Prevalence of asymptomatic and symptomatic peripheral arterial disease in the general population. International Journal of Epidemiology. 1991;20:384–392. doi: 10.1093/ije/20.2.384. [DOI] [PubMed] [Google Scholar]
- 3.Gibson J.M.E., Kenrick M. Pain and powerlessness: The experience of living with peripheral vascular disease. Journal of Advanced Nursing. 1998;27:737–745. doi: 10.1046/j.1365-2648.1998.00599.x. [DOI] [PubMed] [Google Scholar]
- 4.Leech J.E. Psychosocial and physiologic needs of patients with arterial occlusive disease during the preoperative phase of hospitalization. Heart & lung : the journal of critical care. 1982;11:442–449. [PubMed] [Google Scholar]
- 5.Treat-Jacobson D., Halverson S.L., Ratchford A., Regensteiner J.G., Lindquist R., Hirsch A.T. A patient-derived perspective of health-related quality of life with peripheral arterial disease. Journal of Nursing Scholarship. 2002;34:55–60. doi: 10.1111/j.1547-5069.2002.00055.x. [DOI] [PubMed] [Google Scholar]
- 6.Wann-Hansson C., Hallberg I.R., Klevsgard R., Andersson E. Patients’ experiences of living with peripheral arterial disease awaiting intervention: A qualitative study. International Journal of Nursing Studies. 2005;42:851–862. doi: 10.1016/j.ijnurstu.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 7.Orchard T.J., Strandness D.E. Assessment of peripheral vascular disease in diabetes. Report and recommendations of an international workshop sponsored by the American Diabetes Association and the American Heart Association September 18–20, 1992; New Orleans, Louisiana; 1993. pp. 819–828. Circulation;88. [DOI] [PubMed] [Google Scholar]
- 8.Antithrombotic Trialist’ Collaboration Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324:71–86. doi: 10.1136/bmj.324.7329.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stratton I.M., Adler A.I., Neil H.A.W. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo controlled trial. Lancet. 2002;360:7–22. doi: 10.1016/S0140-6736(02)09327-3. [DOI] [PubMed] [Google Scholar]
- 11.Yusuf S., Sleight P., Pogue J., Davies R., Dagenais G. Effects of an angiotensin-converting–enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. New England Journal of Medicine. 2000;342:145–153. doi: 10.1056/NEJM200001203420301. [DOI] [PubMed] [Google Scholar]
- 12.National Collaborating Centre for Primary Care. Clinical guidelines and evidence review for lipid modification: Cardiovascular risk assessment and the primary and secondary prevention of cardiovascular disease. National Collaborating Centre for Primary Care and Royal College of General Practitioners. 2008 [online]. http://publications.nice.org.uk/lipid-modification-cg67. (Accessed 5 Dec 2012).
- 13.Squires H., Simpson E., Meng Y., Harnan S., Stevens J., Wong R. Cilostazol, nadtidrofuryl oxalate, pentoxifylline and inositol nicotinate for the treatment of intermittent claudication in people with peripheral arterial disease. Health Technology Assessment. 2010 doi: 10.3310/hta15400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dake M.D., Ansel G.M., Jaff M.R. Paclitaxel-eluting stents show superiority to balloon angioplasty and bare metal stents in femoropopliteal disease. Circulation: Cardiovascular Interventions. 2011;4:495–504. doi: 10.1161/CIRCINTERVENTIONS.111.962324. [DOI] [PubMed] [Google Scholar]
- 15.Klinkert P., Schepers A., Burger D.H.C., Bockel JHv, Breslau P.J. Vein versus polytetrafluoroethylene in above-knee femoropopliteal bypass grafting: Five-year results of a randomized controlled trial. Journal of Vascular Surgery. 2003;37:149–155. doi: 10.1067/mva.2002.86. [DOI] [PubMed] [Google Scholar]
- 16.Burger D.H.C., Kappetein A.P., van Bockel J.H., Breslau P.J. A prospective randomized trial comparing vein with polytetrafluoroethylene in above-knee femoropopliteal bypass grafting. Journal of Vascular Surgery. 2000;32:278–283. doi: 10.1067/mva.2000.106496. [DOI] [PubMed] [Google Scholar]


