A primary developmental task during infancy and early childhood involves the development of self-regulatory capacities. The influence of parenting on this process is key. Infants and young children are highly dependent on their caretakers for regulatory support. Initially regulation is facilitated primarily by the parent and, over time, the infant gradually learns to participate in co-regulatory dyadic processes that lead to the capacity for self-regulation (Beebe, 2011; Beeghly, Fuertes, Liu, Delonis, & Tronick, 2011). Mothers with a history of child maltreatment are at increased risk for psychopathology and exposure to traumatic stress during adulthood, which may impair their ability to support the healthy development of regulatory capacities in their young children. Utilizing a multi-method approach, the current study uses a sample of women with a history of maltreatment to evaluate the influence of a mother’s childhood abuse and neglect and associated adult psychopathology on her parenting behaviors, and to examine whether each of these factors predicts infants’ physiological reactivity and behavioral/emotional regulation following exposure to a social stressor (maternal Still-Face Procedure, SFP; Tronick, Als, Adamson, Wise, & Brazelton, 1978) at 7-months of age.
Infant Biobehavioral Reactivity and Regulation
The capacity for self-regulation underlies psychosocial health, while deficits in regulation are foundational in the development and expression of psychopathology (Tronick & Beeghly, 2011). Regulatory capacities encompass the complex interplay of emotional, physiological, and behavioral components. Successful regulation following exposure to stress involves the ability to modify the intensity and duration of arousal and affective states to avoid excessive stimulation or disorganization, modulate affective expressions, and organize behavior (American Psychiatric Association, 2000). Early regulatory deficits are thought to be strong predictors of individual differences in self-regulatory problems in later childhood which, when chronic, may lead to later behavioral and emotional problems. Consistent with this hypothesis, studies show that high behavioral reactivity and poor regulation in infancy are linked to later distress, defiance, and avoidance (For review see Calkins & Degnan, 2006).
Behavioral and emotional regulation can be defined as the intrinsic and extrinsic processes underlying the management of emotional arousal and adaptive behavioral responses (Calkins, 1994; Gross, 2009; Thompson, 1994). Undoubtedly, emotion regulation involves the management of temperamentally based differences in individual reactivity (Bosquet Enlow et al., 2011; Rueda & Rothbart, 2009); that is, differential capacities for emotion regulation are influenced by individual variability in the intensity and valence of physiological and emotional responses to stimuli. Behavioral and emotional levels of reactivity and regulation are typically measured via parent report or via direct observation in infancy.
Physiological reactivity can be measured using cortisol, a biological marker of the hypothalamic-pituitary-adrenal (HPA) axis stress response. Although psychological stressors eliciting fear, anger, or frustration do not reliably stimulate cortisol secretion in young children who have been studied from 6 months of age through toddlerhood (Jansen, Beijers, Riksen-Walraven, & de Weerth, 2010), well documented individual differences in cortisol reactivity exist, and increased cortisol levels following stressors may constitute a marker of neurodevelopmental risk (Haley & Stansbury, 2003; Jansen et al., 2010; Mesman et al., 2009). Cortisol levels may also influence the development of regulatory capacities and emotional and behavioral disturbances during childhood (Granger, Stansbury, & Henker, 1994; Granger, Weisz, McCracken, & Ikeda, 1996). On the other hand, hypoactivation of the HPA axis can be indicative of psychological problems among adults (Heim et al., 2009), but the lack of mobilization of the cortisol response appears to be normative and adaptive among infants (Jansen et al., 2010).
A well validated assessment of infant reactivity and regulatory capacities is the “Still-Face” paradigm (SFP; Mesman, van IJzendoorn, & Bakermans-Kranenburg, 2009; Tronick et al., 1978), which induces robust increases in infant negative affect, a decrease in positive affect, and social disengagement from the mother (Haley & Stansbury, 2003; Mesman et al., 2009). After a Still-Face episode, when mothers re-engage in normal social play with their babies, infants typically exhibit a carry-over of negative affect, as well as a partial rebound of positive affect and social engagement with the mother (Mesman et al., 2009). In terms of physiological responses, increases in cortisol levels are documented among 27% of infants after the SFP (Grant et al., 2009).
The Development of Regulatory Capacities within a Relational Context
The behavioral and physiological manifestations of reactivity and regulation are shaped by both biological predispositions and early environmental influences (Cole, Zahn-Waxler, Fox, Usher, & Welsh, 1996; Rueda & Rothbart, 2009), especially early mother-child interactions (Eisenberg et al., 2010; Loman & Gunnar, 2010). In early childhood, the caregiving environment interacts with individual predispositions and broader environmental risk factors to shape child development (Sameroff et al., 2007). Infants first learn regulatory skills in the context of the parent-infant relationship, through the repeated experience of being calmed and soothed by the parent (Schore, 2003). Research supports strong links between maternal characteristics (maternal mental health) and behaviors (parenting) and infant biobehavioral regulation (e.g., (Feldman et al., 2009; Field, Diego, & Hernandez-Reif, 2009).
Maternal positive parenting refers to a constellation of maternal behaviors (e.g., behavioral and affective sensitivity, engagement, warmth, and positive affect) that are associated with less infant negative affect during stressful situations and more positive affect and social behaviors after the stressor (Braungart-Rieker, Garwood, Powers, & Wang, 2001; Kogan & Carter, 1996; Weinberg, Tronick, Cohn, & Olson, 1999). Importantly, infants’ ability to re-engage in dyadic play and re-bound from the stress of the Still-Face predicts infants’ secure attachment status at 12 months, an important marker of positive infant development (Braungart-Rieker et al., 2001). In contrast, parent–child interactions characterized by low levels of sensitive/responsive parenting are associated with increased emotional reactivity, more negative mood and increased fearfulness during infancy and early childhood (Edhborg, Seimyr, Lundh, & Widström, 2000; Pauli-Pott, Mertesacker, & Beckmann, 2004).
The development of the HPA axis response is also highly influenced by the social environment (Gunnar & Donzella, 2002). Responsive maternal parenting can buffer infants from high levels of physiological arousal. Greater maternal sensitivity predicts less infant cortisol reactivity to psychosocial stress (Feldman et al., 2009; Gunnar, Larson, Hertsgaard, Harris, & Brodersen, 1992) and lower resting cortisol levels (Blair et al., 2008), which adaptively minimizes the deleterious neurotoxic effects of chronic brain tissue exposure to cortisol (Charmandari, Tsigos, & Chrousos, 2005).
Importantly, a history of childhood maltreatment (i.e., physical, sexual, and psychological abuse, as well as emotional and physical neglect) impacts multiple domains of psychosocial functioning during adulthood, and victims have increased risk for PTSD and depressive symptomatology (Beitchman, Zucker, Hood, & DaCosta, 1992; Feerick & Snow, 2005; Gladstone et al., 2004), high rates of re-traumatization (Arata, 2002; Barnes, Noll, Putnam, & Trickett, 2009; Desai, Arias, Thompson, & Basile, 2002), and increased risk of single parenthood and poverty (Lipman, MacMillan, & Boyle, 2001), which may all influence parenting behaviors. Indeed, women with histories of childhood sexual abuse report more negative views of their parenting capacities, and engage in parenting practices that are both more physically punishing and more permissive (Banyard, 1997; Cole, Woolger, Power, & Smith, 1992; Obel et al., 2005; Robinson, Mandleco, Olsen, & Hart, 1995).
Maternal psychopathology during the postpartum period can also interfere with mothers’ capacity to care for her infant. Although individual differences are marked, depressed women as a group tend to be less responsive and attentive, more withdrawn, intrusive and negative in their interactions with their infants, and report more negative perceptions of their child (Connell & Goodman, 2002; Feng, Shaw, Skuban, & Lane, 2007; Gelfand & Teti, 1990; Hammen, Burge, & Adrian, 1991; Constance Hammen, Shih, & Brennan, 2004; Reissland, Shepherd, & Herrera, 2005). Consequently, infants and young children of depressed women are more likely than children of non-depressed women to show increased levels of negative affect or reactivity (Huot, Brennan, Stowe, Plotsky, & Walker, 2004),deficits in fear regulation (Davis et al., 2004; Feldman et al., 2009), and heightened cortisol reactivity after a stress-induction task (Brennan et al., 2008; Feldman et al., 2009).
The effect of maternal PTSD on parenting and infant reactivity and regulation is less well understood. Some research suggests that traumatized women experiencing PTSD symptoms engage in less sensitive parenting than their non-traumatized counterparts (Levendosky & Graham-Bermann, 2001), potentially due to heightened fear responses to trauma-related triggers, which result in frequent frightened or frightening behaviors during interactions with their children (Cassidy & Mohr, 2001). Maternal PTSD symptoms are associated with infants’ heighted emotional reactivity during the SFP (i.e., hard-crying during the Still-Face episode) and greater difficulty in regulation and recovery following the stressor (i.e., hard crying after the Still-Face episode) (Bosquet Enlow et al., 2011). Although only a handful of studies has evaluated the link between maternal PTSD and offspring physiological reactivity, results show increased cortisol reactivity to a fear-induction task among infants of women with concurrent PTSD symptoms, secondary to a history of child abuse (Brand et al., 2010). However, these studies do not account for the influence of maternal parenting or evaluate the independent effects of maternal childhood maltreatment, psychopathology, and maternal parenting on infant outcomes.
In the current study, we evaluate these associations using a sample of mothers with a high rate of childhood maltreatment. The current study fills an important gap in the literature by examining the independent contributions of mothers’ history of childhood maltreatment, and postpartum maternal psychopathology to observer-rated parenting behaviors. In addition we assessed the influence of poverty and single parenthood, both of which are associated with maternal history of childhood maltreatment, as well as maternal positive parenting behaviors on infants’ emotional reactivity during stressful experiences (i.e., distress exhibited during a social stressor, the maternal Still-Face), physiological reactivity to stressors (i.e., stress-related cortisol levels), and emotional regulation following the stressor (i.e., a rebound of positive engagement with mother and positive affect during the SFP Reunion episode). Our findings shed light on specific mechanisms that may result in biobehavioral dysregulation among infants of mothers with histories of childhood maltreatment and suggest promising avenues for future research.
Hypotheses
Women’s history of childhood maltreatment will predict higher levels of depressive and PTSD symptoms at 7 months postpartum.
Women’s history of childhood maltreatment, demographic risk factors, and higher depressive and PTSD symptoms will predict lower levels of maternal positive parenting at 7 months postpartum.
Maternal psychopathology and positive parenting at 7 months will predict infants’ distress levels during a stressor episode and their behavioral and physiological recovery after the stressor. Specifically, mothers with higher levels of concurrent depressive or PTSD symptoms and lower levels of positive parenting at 7 months postpartum will have infants who display more behavioral reactivity during the Still-Face episode, and who show greater behavioral and physiological evidence of stress or distress following it.
Method
Participants
This research uses data collected through an ongoing longitudinal study (N=268) that evaluates the effects of a history of childhood maltreatment on mothers’ postpartum psychosocial adaptation and parenting, and whether these factors predict children’s behavioral and physiological outcomes (MACY study; NIMH K23 MH080147). Participants were recruited either from a pregnancy survey of the effects of PTSD on childbearing via three prenatal care clinics (n = 155; for a comprehensive description, see Seng, Low, Sperlich, Ronis, & Liberzon, 2009) or through community advertisement (n =113). Recruitment via the first method involved direct invitation of women at their first prenatal visit. Recruitment through the second method involved flyers posted in antenatal and primary care clinics, informal and state-funded (e.g., WIC, Maternal-Infant Health Programs) resource centers for pregnant and postpartum women, baby clothing and toy stores, and perinatal mental health clinics within the same community. Mothers were eligible to participate if they were at least 18 years of age at intake, were English-speaking, were pregnant or had a healthy baby between 0 and 6 months of age who was not born more than 6 weeks prematurely, had no history of schizophrenia or bipolar disorder, and endorsed no problems with alcohol or drugs during the past 3 months. Interested women completed an initial telephone survey to determine eligibility, which included the Childhood Trauma Questionnaire (CTQ, Bernstein & Fink, 1998), a measure of childhood maltreatment experiences. Women who met eligibility criteria were invited to participate in the study, and provided oral assent for participation. During the first in-person assessment (at 7 months) mothers provided written consent for participation.
Analyses in the current study were based on data collected from a subset of 153 mother-infant dyads (52% with male infants) that completed the 7-month home assessment. Ninety-four women came from the pregnancy survey and 59 came from the community recruitment. Community recruits had lower income and higher levels of childhood maltreatment, depression, and PTSD symptoms, but did not differ in regards to infant outcomes. At intake, mothers’ age ranged from 18 to 45 years (M = 29.06, SD = 5.67). Fifty-six percent of the mothers self-reported their race/ethnicity as Caucasian, 22% as African American, 13% as multiracial, 4% as Hispanic, and 5% as “other”. Seventy-seven percent of the mothers were married or living with a partner whereas 23% were single and/or not living with a partner. The sample varied in educational and socioeconomic status (SES): Fifteen percent of the mothers had completed a high-school degree or less education, 30% completed some college, 31% completed a bachelor’s degree and 24% had attained post graduate education (masters or doctoral degree). The median annual family income was $45,000–49,999 with a range from below $15,000 to $150,000 yearly. Seventy-six percent of mothers had a history of childhood maltreatment and many women experienced multiple forms of abuse, including emotional abuse (60%) emotional neglect (50%), physical abuse (35%), physical neglect (31%), and sexual abuse (43%). Participating women were classified as maltreated and with a history of PTSD (50%), maltreated without a history of PTSD (27%), and non-maltreated without a history of PTSD (23%).
Procedure
All participants completed the screening questionnaire when their infants were about 4 months old and agreed to complete two home-assessments when their baby was 7 months old. If the participant had concerns about the home assessments, we offered to conduct the assessments at the university-based playroom. During the first home visit mothers signed a written consent to participate with their infants in the study, completed interviews and interactive tasks, and were left with a packet of self-report questionnaires to complete, which was retrieved at the second home visit (approximately 1–2 weeks later). A small percentage of dyads (12%) did not complete the SFP during the first home visit, but completed it during the 2nd home visit. Preliminary bivariate analyses showed that salivary cortisol reactivity was not different for infants who completed the SFP on the first versus the second home visit. The examiners who conducted the home visits were all trained bachelor’s- or master’s-level study team members.
Measures
Dependent variables: Infant outcomes
The primary dependent variables in this analysis were infants’ behavioral and affective responses during the Still-Face episode and the Reunion episode of the Still-Face Paradigm (SFP; Tronick et al., 1978) and infants’ physiological responses (cortisol reactivity) following the SFP. The SFP is a widely used, well validated observational paradigm designed to evaluate individual differences on maternal and infant behavioral and physiological responses before and after a social interactive challenge (a maternal still-face). In the current study, the SFP was videotaped in the home setting when infants were about 7 months old (M = 6.14 months, SD = .71, range = 5 to 8). Prior research has demonstrated the feasibility of conducting the SFP in the home environment with infants at this age (Meijssen et al., 2010; Neu & Robinson, 2010). During the SFP, the baby was seated in an infant car seat on the floor facing the mother. A mirror was placed behind the dyad to allow for optimal camera views of each partner. The SPF comprised three successive 2-minute episodes: a) a “normal” dyadic play episode (Play 1), during which the mother was asked to play with her infant in an en face position in a normal manner, followed by b) a maternal still-face episode (Still-Face), during which the mother was instructed to hold a neutral/unresponsive face while looking at her infant and to refrain from touching or talking to the infant, followed by c) a re-engagement episode (Reunion) during which the mother resumes her normal social play with the infant. No toys or pacifiers were allowed during the SFP.
Coding of infant behavior
Infants’ behavior during each episode of the SFP was scored from videotapes by a trained, reliable coder masked to maternal trauma history and other study variables using relevant scales from the MACY Infant-Parent Coding System (MIPCS; Earls, Muzik, & Beeghly, 2009). The MIPCS includes 14 maternal, 10 infant, and 4 dyadic rating scales (all described as 5-point Likert scales) that assess multiple dimensions of mother-infant interactive behavior relevant to attachment formation as guided by attachment theory and related literature (e.g., Ainsworth, Blehar, Waters, & Wall, 1978; Crittenden, 1981; Lyons-Ruth, Bronfman, & Parsons, 1999; Lyons-Ruth, Zoll, Connell, & Grunebaum, 1986; Main & Hesse, 1990). With a few exceptions, MIPCS scales were adapted from those used in several extant scoring systems (e.g., Marjorie Beeghly, 2006; Clark & Seifer, 1985; Dayton et al., 2010; Egeland & Hiester, 1995; R Feldman, 1998). Infants’ level of distress during the Still-Face episode was scored using the MIPCS Infant Negative Affect scale (M = 1.24, SD = 1.03, range = 0 to 3) and used as a covariate to control for individual differences in infant reactivity prior to the Reunion episode (Rueda & Rothbart, 2009). A composite variable reflecting infants’ positive “recovery” from stress during the Reunion episode was derived using Principal-Components Factor Analysis. The Positive Recovery score (M = 2.56, SD = 0.84, range = 1.00 to 4.67) is the sum of three inter-related infant scales: Responsivity/Compliance, Social Engagement, and Positive Affect. The standardized Cronbach’s alpha for this variable was .86.
Inter-coder reliability with the primary coder was assessed for each infant scale described above using intra-class correlations (ICC) on 40 randomly selected videotapes that were independently scored by a trained coder masked to maternal trauma history and background variables. Each scale had good to excellent inter-coder reliability: Infant Responsivity/Compliance (ICC= .91), Infant Social Engagement (ICC = .89), Infant Positive Affect (ICC= .95), and Infant Negative Affect (ICC = .94).
Infant salivary cortisol
Repeated saliva samples were collected from the infant before (baseline) and after the SFP. The baseline was collected 15 minutes into the home visit, after the consent form was explained and signed, and before any interactive tasks had begun. Consistent with established protocols (Granger et al., 2007), cortisol was collected again 20, 40 and 60 minutes following the SFP. Mothers were asked to place a cotton roll, securely attached to a strand of floss, in their infant’s mouth until it was saturated with saliva. It was then removed and placed in a Salivette Tube (Sarstedt, Sevelen, Switzerland). Saliva samples were centrifuged at 7000 rpm for 10 minutes, and stored at −20C until assayed. Samples were assayed using one of three techniques based on lab and equipment availability: ELISA (40%), RIA (21%) or Immulite (39%). All samples from the same infant were assayed in the same batch to minimize inter-assay variation. Inter- and intra-assay coefficients of variation were consistently below 10%. Following the assays, cortisol data were cleaned. Samples with values above 3mg/dl, which indicate likely errors, were deleted, as were samples whose cortisol values fell three or more standard deviations above or below the assay means. In the samples retained, cortisol values ranged from .01 to 1.36 mg/dl.
Several variables were recorded as potential covariates in cortisol analyses. Given known diurnal fluctuations in resting cortisol levels among older children and adults, sample collection time was recorded. Infants’ birth weight, health at the time of the 7-month visit, and the time at which infants were last fed and last slept that day were also recorded.
Classification of infant cortisol response
Following Schuetze, Lopez, Granger, and Eiden (2008), infants who displayed a cortisol increase >= 10% from baseline at 20- or 40-minutes post-SFP were classified as ‘Responders’ (Schuetze et al., 2008). Infants who did not increase by at least 10% after the SFP were classified as ‘Non-Responders’. This classification system was adopted based on the inter- and intra-assay variability coefficients (>10%), such that difference scores higher than 10% represent an increase unlikely to be due by chance. Using this methodology, cortisol responder status has reliably discriminated individual and environmental characteristics in previous research, including higher prenatal tobacco exposure (Schuetze et al., 2008), more negative emotional reactivity during frightening and frustrating tasks among infants (Fortunato, 2009) and more avoidance during social interactions among toddlers (Corbett, Schupp, Simon, Ryan, & Mendoza, 2010). Within our sample, 48% of infants were classified as responders and 52% as non-responders. The percentage of children classified in each group was not significantly different across assay techniques.
To validate this classification method within our sample, we also examined the trajectories of change in cortisol levels. Twenty-three percent of infants showed a >= 10% increase from baseline to post-SST (at 20- or 40-minutes), 45% showed a >= 10% decrease from baseline to post-SST (at 20- or 40-minutes), and 22% showed an unstable pattern, such that they displayed increased cortisol levels at one post-SST time point and decreased cortisol levels at another post-SST time point (e.g., decreasing >= 10% from baseline to 20 minutes, and increasing >=10% from baseline to 40 minutes). Preliminary comparison of these three groups using ANOVA revealed that infants who showed the decreasing pattern of cortisol differed from those who increased or were unstable, showing more positive affect during the SFP reunion and higher levels of maternal positive parenting. Responder and unstable infants did not differ in their environmental or individual characteristics, suggesting that cortisol increase is the key element that distinguishes infants. Thus, the responder (1) vs. non-responder (0) classification will be used in all statistical analyses.
Independent variables: Maternal parenting and risk factors
Maternal positive parenting
Multiple dimensions of maternal parenting behavior were scored from videotapes of mother-infant interaction during two different tasks: a 5-minute free play task and a 6-minute teaching task. The free play task was completed twice (one during each home visit), and an average score was computed to reflect how dyads typically interact under non-challenging circumstances. A standard set of age-appropriate toys provided by the study team was arranged on a quilt on the floor, and mothers were invited to play with their infant as they normally would. Following one of the two free play sessions, dyads participated in two consecutive teaching tasks (each lasting about 3 minutes). In the first task, mothers were instructed to teach their infant how to put colorful plastic blocks into a bucket. In the second task, mothers were instructed to teach their infant how to stack a set of nesting cups and then knock them down. Both teaching tasks were designed to be beyond the infants’ developmental capacities and were used to provide an assessment of maternal parenting under more challenging circumstances. Laboratory free play tasks have been demonstrated to have moderate ecological (Goossens & Melhuish, 1996), concurrent (Clark, 1999) and predictive validity (Aoki, Zenah, Heller, & Bakshi, 2002) for both maternal and infant coded behaviors.
Maternal behavior was scored by a trained, reliable coder using the maternal ratings included in the MIPCS (described above). Maternal ratings in the two teaching tasks were significantly correlated and averaged for analytic purposes. Inter-coder reliability for each maternal rating scale was assessed using intra-class correlations (ICC). Trained coders masked to maternal trauma history and other study variables independently scored 40 randomly selected videotapes. The ICCs for the maternal scales were generally well above .80, with one exception (see below), denoting very good inter-coder agreement: Maternal Behavioral Sensitivity (ICC free play = .85; ICC teaching tasks = .86); Maternal Engagement (ICC free play = .86; ICC teaching tasks = .71); Maternal Warmth (ICC free play = .84; ICC teaching tasks = .91); Maternal Affective Sensitivity (ICC free play = .86; ICC teaching tasks = .85; and Maternal Positive Affect, ICC free play = .93; ICC teaching tasks = .85).
Following a conceptually driven data reduction analysis (principal-components factor analysis), “Positive Parenting” composite scores were computed for the free play task and the teaching task, by averaging scores from the five interrelated maternal rating scales. The standardized Cronbach’s alpha for the Positive Parenting composite during free play was .92, and scores ranged from 1.63 to 4.58 (M = 3.76, SD = .65). The standardized Cronbach’s alpha for the positive parenting score during the teaching tasks was .92 and scores ranged from 1.46 to 4.54 (M = 3.14, SD = .74).
Maternal child abuse history
The Childhood Trauma Questionnaire (CTQ; Bernstein & Fink, 1998) was completed by mothers at four months postpartum. Mothers self-rated their childhood maltreatment experiences on a 28-item, 5 point Likert scale (1-never true to 5-very often true). The CTQ yields subscale scores for childhood emotional, physical, or sexual abuse, as well as physical and emotional neglect. Test-retest reliabilities range from 0.79 to 0.86, and good validity has been reported, based on correlations with trauma sequelae (Bernstein & Fink, 1998), a structured interview for childhood trauma, and therapist ratings of childhood trauma (David P Bernstein et al., 2003). In the present study, a total abuse score was obtained by adding the abuse and neglect scales. Scores ranged from 25 to 121 (M= 44.49, SD = 17.66).
Maternal depressive symptoms
Mothers reported current depressive symptoms at the 7-month home visit using the Postpartum Depression Screening Scale (PPDS; Beck & Gable, 2002). The PPDS includes 35 items that are rated using a 5-point Likert scale (1=strongly disagree to 5=strongly agree). Scores are summed to yield a total symptom score. This scale has a sensitivity of 0.78, a specificity of 0.99 and a positive predictive value of 0.93 compared with a structured-interview (SCID) depression diagnosis. In prior research with postpartum women, internal consistency was standardized Cronbach’s alpha of 0.97 (Beck & Gable, 2000). A score of 80 or higher denotes clinically significant symptomatology (Beck & Gable, 2000). Twenty-five percent of women had clinically significant depression at the 7-month data collection. In the present study, a continuous score was used in the statistical analyses. PPDS scores in this sample ranged from 35 to 132 (M = 63.79, SD = 23.31).
Maternal PTSD symptoms
Mothers reported on their lifetime PTSD symptoms during the telephone screening or at the home visits. Women also reported their current PTSD symptoms at the 7-month home visit using the National Women’s Study PTSD Module (NWS-PTSD; Resnick, Kilpatrick, Dansky, Saunders, & Best, 1993). This 26-item instrument is a version of the Diagnostic Interview Schedule (DIS) that was modified for use in large epidemiological studies. The scale items assess all 3 PTSD domains (intrusion, avoidance and hyperarousal), and an algorithm follows DSM-IV criteria to derive a PTSD diagnosis (must meet at least 1 intrusion, 3 avoidance, and 2 hyperarousal symptoms). External validity is good, as shown by adequate agreement (kappa = .77) with a clinician-administered structured interview (SCID), high sensitivity of 0.99 and adequate specificity of 0.79, as compared with the SCID (Resnick et al., 1993). Twenty-seven percent of women met PTSD criteria at the 7-month data collection. A continuous current PTSD symptom count score was used in statistical analyses. PTSD scores ranged from 0 to 17 in this sample (M = 4.51, SD = 4.55).
Psychosocial stress exposure
During the 4-month telephone interview, mothers reported on their exposure to specific stressors and traumatic events during the time interval between 6 weeks and 4 months postpartum using a modified version of the Life Stressors Checklist (LSC; Wolfe & Kimerling, 1997). Items included common stressful or traumatic experiences, including environmental and interpersonal stressors (e.g., money problems, harassment, physical or sexual abuse). For analytic purposes in this study, a total trauma exposure score was computed adding all items, ranging from 0 to 6 (M= .81, SD = .97).
Demographics
During the 7-month home visit, mothers reported on their current living situation, relationship status, race/ethnicity, employment status, and education level, and provided information regarding their family’s total annual income.
Results
Missing Data
Results of preliminary bivariate analyses revealed no evidence for differential attrition: The subsample of participants who completed the 7 month visit (N = 153) did not differ significantly from the participants in the larger MACY study (N = 268) on key demographic characteristics, including maternal age, race/ethnicity, education, or partner status, the family’s total annual income, or on infant race/ethnicity or gender. In the present analysis, 9% of all data points were missing overall. For infant salivary cortisol, the most common reason for missing scores was the infant being asleep at the time or unable to provide enough saliva for the assay. Those infants with complete salivary cortisol data did not differ from those with missing samples on any demographic or independent variable evaluated. Bivariate associations showed no relationships between any cortisol measures (including responder status) and time of sample collection, infants’ birth weight, infants’ health at the time of the 7-month visit, or time from last feeding or sleeping. Therefore these factors were not included in final statistical models.
Reasons for missing behavioral data included technical problems with videotaping, participant scheduling conflicts, or examiner error. Mother-infant dyads with complete observational data did not differ from those with missing scores on any demographic or risk variable included in this study. Thus, there is no indication of sample bias due to missing data. Full Information Maximum Likelihood (FIML) was used to handle missing data in all statistical analyses. The FIML approach fits the model to all of the non-missing values for each observation and maximizes power by using all of the participants in the analysis (Widaman, 2006). In addition, the M-plus program, which is used for the Structured Equation Models (SEM) reported in this paper, employs test statistics in FIML that are robust to non-normally distributed data (Allison, 2003; Muthén & Muthén, 2007).
Descriptive Statistics
Bivariate correlations were used for preliminary examination of the pattern of associations between variables. Pearson product-moment correlation was used to measure the association between continuous variables, while point-biserial correlations and the phi coefficient were used for the two dichotomous variables (single mother and cortisol reactivity). As seen in Table 1, a history of childhood maltreatment was significantly associated with increased psychosocial stress postpartum, as well as current levels of depressive and PTSD symptoms. Positive parenting was not associated with a history of childhood maltreatment, severity of abuse or type of abuse (i.e., physical vs. sexual). Maternal positive parenting showed moderate to strong associations with demographic risk variables (i.e., total annual income and single mother status), and with maternal post-partum PTSD and depressive symptoms. Infants’ positive behavior during the Reunion episode of the SFP and was associated with maternal positive parenting and infant distress during the Still Face episode. Finally, infants’ cortisol reactivity status (Responder vs. Non-Responder) was moderately associated with maternal levels of depression and maternal positive parenting.
Table 1.
Bivariate Correlations
| 2 | 3 | 4 | 5 | 6a | 7 | 8 | 9 | 10 | 11a | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Childhood Maltreatment History | .38* | .53* | .25* | −.14 | −.01 | −.05 | −.06 | −.05 | .05 | −.12 |
| 2. Maternal Depressive Symptoms | .58* | .27* | −.12 | .08 | −.24* | −.15 | .11 | .07 | .27* | |
| 3. Maternal PTSD Symptoms | .22* | −.08 | −.01 | −.06 | −.04 | .07 | .12 | .21 | ||
| 4. Trauma and Stress | −.28* | .30* | −.21* | −.23* | .01 | −.01 | .14 | |||
| 5. Total Family Income | −.47* | .40* | .33* | −.02 | −.04 | −.07 | ||||
| 6. Single Mother (1 = single mom) | −.52* | −.40* | .10 | −.02 | .17b | |||||
| 7. Positive Parenting-Free Play | .79* | −.15 | .26* | −.32* | ||||||
| 8. Positive Parenting - Teaching Tasks | −.17 | .27* | −.25* | |||||||
| 9. Infant Distress during Still Face Episode | −.37* | .13 | ||||||||
| 10. Infant Positive Behavior - Reunion | −.32* | |||||||||
| 11. Infant Cortisol Reactivity (0 = Non-Responder) |
Note.
= point-biserial correlation.
p < .05.
Hypothesis Testing
To investigate the relationship between maternal history of childhood abuse, environmental risk, maternal psychopathology, and maternal parenting on infant behavioral and physiological dysregulation, structural equation model (SEM) was used. All SEM models were fitted using M-plus 5.2 (Muthén & Muthén, 2007) with FIML estimation. Global model fit was evaluated using the overall χ2 test of model fit (p > .05), the root mean square error of approximation (RMSEA < 0.08; Browne & Cudeck, 1993), and the comparative fit index (CFI > 0.95). Based on the widely used guideline of 5 to 10 cases per parameter, the present sample size was appropriate for model testing.
The hypothesized model is displayed in Figure 1. A history of childhood maltreatment was predicted to influence mothers’ post-partum exposure to psychosocial stressors, depressive and PTSD symptom levels, and maternal parenting quality (i.e., latent variable derived of positive parenting during free-play and teaching tasks). In addition, maternal depressive and PTSD symptom levels and environmental risks (psychosocial stress, being a single parent, and total family income) were expected to predict lower levels of maternal positive parenting in observed mother-infant interactions across both low- and high-challenge observational tasks. Finally, our indices of maternal mental health and parenting behaviors assessed at 7 months were hypothesized to influence the infant’s behavioral and physiological regulation following a social stressor (SFP) at the same age. Infants’ observed levels of positive affect and behavior during the post-still face reunion were used as the behavioral outcome, while children’s classification as cortisol “Non-Responder (0)” or “Responder (1)” following the SFP was used as the physiological outcome.
Figure 1. Hypothesized Model of Early Biobehavioral Regulation.
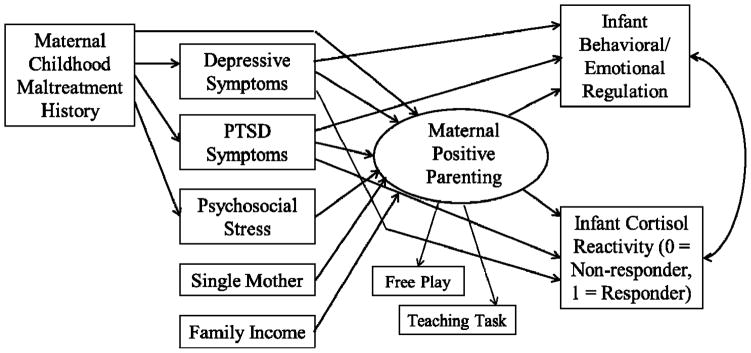
Partial mediation model. Proposed direct and mediated effects of maternal childhood abuse on maternal parenting, via maternal psychopathology and traumatic stress. Also includes direct and indirect effects for maternal psychopathology on infant biobehavioral regulation, via maternal positive parenting.
Global fit indices indicate the proposed model does not provide a good fit for the observed data, χ2= 72.90, df = 24, p = .00; CFI = .85, RMSEA = .12. The paths predicting infant outcomes from maternal levels of depressive and PTSD symptoms at 7 months were non-significant, and were taken out of the model. In addition, maternal positive parenting at 7 months was not associated with maternal childhood maltreatment history. To further examine this association, post-hoc correlations between different types of childhood abuse and maternal parenting were estimated. All correlations were non-significant (r = −.13 to .05). In addition, ANOVA was used to compare the parenting of those who experienced severe abuse and those who did not. Results indicated non-significant differences, F = .26 (1, 140), p = .61 for free play positive parenting, and F = .08 (1, 140), p = .78 for teaching task positive parenting. Thus, the path from childhood maltreatment to positive parenting was also dropped from the model. Model trimming resulted in improved fit, χ2= 77.47, df = 29, p = .01; CFI = .85, RMSEA = .11. In addition, and consistent with expectations, maternal levels of depression and anxiety at 7 months were highly correlated, although each measure was differentially associated with maternal positive parenting. When the correlation between depressive and PTSD symptoms was included, model fit was good, χ2= 42.32, df = 28, p = .04; CFI = .96, RMSEA = .06.
The final model (See Figure 2) explained 10% of the variance in infants’ cortisol responder status and 7% of the variance in infants’ positive behavioral and affective responses during the Reunion episode of the SFP. A history of childhood maltreatment significantly predicted higher levels of maternal depressive symptoms (std b = .39, p = .00), PTSD (std b = .55, p = .00), and psychosocial stress (std b = .25, p = .00) at 7 months postpartum. In turn, higher levels of maternal depressive symptoms (std b = −.24, p = .01), being a single mother (std b = −.41, p = .00), and income (std b = .19, p = .02) were significantly associated with maternal parenting. Finally, positive maternal parenting at 7 months predicted a higher level of infant’s positive behavior and affect during the Reunion episode of the SFP at the same age (std b = .26, p = .00) and decreased the odds of the infant being classified as a cortisol “Responder” (std b = −.32, p = .00). The indirect effect of depression on infant outcomes via positive parenting was tested, and it was significant for both cortisol responder status (std b = .07, p = .04), and infant positive behavior and affect during the SFP reunion (std b = −.06, p = .04).
Figure 2. Empirical Results from Infant Biobehavioral Regulation Model.
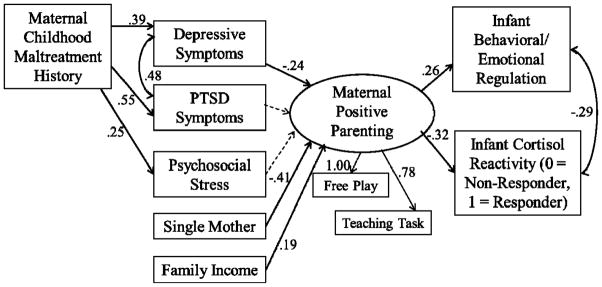
Structural Equation Modeling results using FIML with standardized parameter estimates. Solid lines are p < .05. Dashed lines are p > .05.
The model was also estimated controlling for the association between infant distress during the Still-Face episode and infant’s positive affect and behavior during the Recovery episode, and results were unchanged. To explore potential differences between participants recruited from the community and those who previously participated in the pregnancy trauma survey, a 2-group SEM model was estimated. Model fit for this model was acceptable, but worse than that of the more parsimonious one group model, suggesting that the initial one-group model provides the best explanation for these data.
Discussion
Using observational, self-report, and biobehavioral assessments, the present study examined the association of a maternal history of maltreatment during childhood, maternal PTSD and depressive symptoms at 7 months postpartum, with concurrent assessments of maternal positive parenting and children’s behavioral and physiological reactivity and regulation following exposure to a relational stressor (SFP). Findings suggest that a history of child maltreatment, in and of itself, is not associated with reduced ability to engage in maternal positive parenting at 7 months postpartum. However, survivors of child maltreatment were more likely to report postnatal psychosocial stress and higher levels of depressive and PTSD symptoms. In turn, high levels of depressive symptoms, though not PTSD symptoms, were associated with less positive maternal parenting behaviors. Further, less positive maternal parenting was associated with more infant physiological reactivity and less behavioral/emotional regulation.
Maternal Positive Parenting
Consistent with prior studies of physically and sexually abused women (Arata, 2002; Barnes et al., 2009; Beitchman et al., 1992; Feerick & Snow, 2005; Gladstone et al., 2004), our results suggest that a history of maltreatment during childhood is robustly associated with higher adult levels of depressive symptoms, PTSD symptoms, and exposure to psychosocial stress. However, contrary to our prediction, a history of childhood maltreatment was not directly associated with maternal positive parenting behaviors. Further, post-hoc mean difference and correlational analyses revealed that positive parenting was also not influenced by the severity of abuse or the type of abuse experienced (i.e., physical vs. sexual). Opposite to findings using women’s self-reports of parenting, previous objective observations of mother-child interactions have shown similar levels of maternal sensitivity, support, assistance, and confidence among abused and non-abused mothers (DiLillo, Tremblay, & Peterson, 2000; Fitzgerald et al., 2005), suggesting that, among child maltreatment victims, perceptions of ones parenting may not translate into observable behaviors.
Instead, positive parenting behaviors were associated only with demographic characteristics (e.g., single parenthood and low SES) and level of concurrent depressive symptomatology. The association of maternal depressive symptoms at 7 months postpartum with lower maternal positive parenting is consistent with expectations and prior research findings (Connell & Goodman, 2002; Constance Hammen et al., 2004; Reissland et al., 2005) . One possible mechanism accounting for this association has been identified by Lovejoy, Gracjzik, O’Hare and Neuman (2000); these authors propose that parenting difficulties among depressed women may stem from disturbances in the regulation of positive and negative affect, such that women who experience lower levels of positive affect (e.g., symptoms denoting a lack of interest/pleasure and low energy) are more likely to display less engaged and positive affect during social interactions with their children. In addition, specific depressive symptoms (e.g., difficulty concentrating, suicidal thoughts) may interfere with mothers’ capacity to be emotionally available and attentive to her child’s needs and to respond appropriately during daily interactions (Goodman, 2007).
In contrast to the significant influence of depressive symptoms on parenting behaviors, and contrary to our hypothesis, higher levels of PTSD symptoms were not associated with poorer maternal parenting quality during parent-infant interactions. Although clinical work and trauma theory suggest that PTSD symptoms would be strongly associated with less positive parenting (Appleyard & Osofsky, 2003), little empirical data exist to support this hypothesis. PTSD symptoms are psychiatrically unique in that they are, by definition, tied to one or more traumatic events. Thus, it is possible that women’s traumatic experiences translate into maladaptive parenting behaviors only under markedly stressful situations or in response to particular environmental “triggers.” If infant cues are not experienced as “triggering” by mothers, then symptoms may not interfere with a mother’s ability to engage in sensitive, warm, and responsive interactions with their infants.
The striking lack of association between PTSD and parenting may also be a result of the method used to assess maternal parenting in the present research. We captured mother’s interactional style by assigning global codes to free play and teaching tasks and creating a latent variable that represents maternal behaviors across these settings. Assessment of moment-to-moment interactive behaviors is recommended to more accurately understand the parenting behaviors of women with post-traumatic stress symptoms, as their deficits may entail subtle difficulties in appropriately reading infant cues, while positive relational elements (such as engagement and positive affect) are preserved (Feldman et al., 2009).
Infant Reactivity and Regulation
The ability of the infant to regulate biobehavioral processes is embedded in their social context. In this sample, maternal positive parenting was associated with infant cortisol reactivity to stressors, as well as affective and behavioral responses after the stressor, but not with the infant’s response during the stressful situation (i.e., distress during the Still-Face Episode). In addition, none of the additional maternal or environmental characteristics were associated with infant outcomes. Findings have significant long-term implications, as the foundation for later self-regulation is established during infancy (Sroufe, et al.,, 1997). In fact, previous research has established relative continuity from early maladaptive regulatory behaviors (i.e., less frequency, lack of active strategies) to increased behavioral problems and anxiety during toddlerhood and to psychiatric problems during childhood (Calkins & Degnan, 2006).
Infants’ positive affect and social engagement during the Reunion episode was negatively associated with their level of distress during the Still-Face (see Bosquet Enlow et al., 2011 for similar results), suggesting that infants who have higher behavioral reactivity to a stressor have a more difficult time re-engaging in positive interactions with their mother after the stressor is withdrawn (Tronick & Beeghly, 2011). However, maternal positive parenting predicted more positive affect and behavior after the stressor, even after accounting for the effects of behavioral reactivity, suggesting that maternal caregiving may buffer the influence of behavioral risk. Infant’s behavior during the Reunion episode of the SFP may provide particularly valuable information about dyads’ ability to repair “mismatches” and the infant’s ability to be soothed, use the caregiver for comfort, and reorganize behavioral and affective states after the stressor is terminated. Findings are consistent with Mesman et al.’s (2009) meta-analytic review and Beeghly and Tronick’s (2011) “open systems” framework, which proposes that repeated interactions with responsive caregivers result in secure working models of relationships, allowing infants to be more flexible and re-organize in the face of environmental perturbations.
Consistent with prior research (Feldman, 2009), maternal positive parenting predicted infants’ cortisol response following the SFP. Infants with less sensitive, warm, engaged, and joyful mothers, were more likely to be classified as cortisol responders, that is, to show an increase in cortisol levels post-stressor (as compared to baseline). This pattern of cortisol reactivity to psychosocial stressors has been proposed as a marker of neurodevelopmental vulnerability, as it is opposite to the characteristic lack of HPA axis reactivity to psychosocial stressors seen in infants and children (e.g., beginning at 6 months) (Jansen et al., 2011), which is hypothesized to protect the developing brain from the potentially neurotoxic effects of chronic cortisol exposure (Charmandari et al., 2005). Cortisol responder status was not associated with infant distress during the Still-Face, so physiological reactivity was not merely a reflection of behavioral reactivity. Findings highlight the social processes involved in HPA axis early functioning (Gunnar & Donzella, 2002), as well as the potential long-term neurodevelopmental impact of early caregiving (Charmandari et al., 2005).
Infants’ physiological reactivity following the SFP was associated with their behavioral regulation during the Reunion episode. Both of these were positively linked to maternal positive parenting. The disparate temporal course of behavioral reactivity/regulation (which can occur in minutes) and cortisol reactivity (which unfolds over a substantially longer time frame and may be shaped by numerous aspects of the paradigm) makes it difficult to evaluate the causal agents in these linkages. Previous studies examining coordination of physiological and behavioral regulation early in development have yielded inconsistent findings, perhaps due to use of different stress-induction tasks (e.g., doctor visit on Gunnar et al., 1996; repeated SFP on Haley & Stansbury, 2003) and differential time courses in different response channels. We speculate that poor behavioral regulation and higher cortisol levels in the aftermath of the SFP might both reflect weakened infant regulatory capacity as a consequence of the lack of positive parenting. Further research is needed to determine whether there is a direct relationship between the early behavioral dysregulation and the later rise in cortisol, or if this relationship is entirely mediated by their joint linkage to parenting behavior.
Surprisingly, maternal depressive and PTSD symptoms were not linked to infant outcomes within our sample, suggesting that concurrent maternal depressive and PTSD symptoms do not directly influence infant physiological or behavioral responses, and any impact must be indirect through maternal parenting behaviors. However, despite high rates of childhood maltreatment experiences (76% percent maltreated), the number of women currently diagnosed with clinically significant depression or PTSD is relatively low (25% and 27%, respectively), and results may be different with clinical samples. The lack of association may also be a result, at least in part, of the timing of our psychopathology assessment. Women who are currently asymptomatic may have a history of depression or PTSD, and potential genetic vulnerabilities may increase the risk for physiological reactivity and emotional regulation, despite mother’s current functioning.
Limitations and Conclusions
Results of the present study should be interpreted in light of its limitations. First, the cross-sectional nature of the data does not permit making causal attributions for the association between maternal parenting and infant biobehavioral measures. It is possible that child characteristics exert an evocative effect on maternal parenting, and bi-directional associations exist. Within our data, infant’s level of distress during the stressor (a potential marker of negative emotionality) was not associated with the mother’s positive parenting, supporting mother-to-infant effects. However, longitudinal studies are needed to establish the proposed causal link.
In addition, the present study does not include information about genetic vulnerability, and there are known genetic contributions to infants’ reactivity and regulation capacities (Luijk et al., 2010). The results of the present study may be influenced by a gene-environment association, such that genetic similarity contributes to both low positive parenting and infant biobehavioral outcomes. Future research would benefit from a more nuanced understanding of the effects of genetic factors and potential gene-by-environment relationships on infants’ physiological and behavioral reactivity and regulation.
In summary, the results of the present evaluation highlight the impact of maternal parenting behaviors on early biobehavioral reactivity and regulation, a potentially key contributor to long-term neurodevelopment. Mothers who are sensitive, warm, engaged, and joyful during interactions have babies who may be less likely to experience frequent HPA axis activation following distressing events and who may be better able to engage socially and display positive affect once a stressor is terminated, regardless of current maternal mental health symptoms, childhood maltreatment history, and demographic status. Consistent with previous reports, maternal parenting is influenced by women’s depressive symptoms and demographic risk, but is not a direct result of maternal maltreatment history. Findings underscore the importance of early maternal parenting, suggesting that single, low-income, depressed mothers are at heightened risk for parenting deficits, and interventions with this high-risk group that target parenting skills may interrupt one mechanism implicated in infant biobehavioral risk.
Acknowledgments
Support for this research or manuscript preparation was provided by grants from the National Institute of Mental Health and Eunice Kennedy Shriver National Institute of Child Health and Human Development (MH080147; PI: Muzik) and the Michigan Institute for Clinical and Health Research (MICHR) at the University of Michigan (UL1RR024986; PI: Muzik). The authors wish to thank the mothers and children who made this research possible and gratefully acknowledge the valuable feedback from James L. Abelson, MD., PhD., and the contributions of Amanda Fezzey, Heather Cameron, Rena Menke, Alexi Wisher, Lauren Earls, Lori Stark, Alex Busuito.
Contributor Information
Cecilia Martinez-Torteya, University of Michigan.
Carolyn J. Dayton, University of Michigan
Marjorie Beeghly, Wayne State University.
Julia S. Seng, University of Michigan
Ellen McGinnis, University of Michigan.
Amanda Broderick, University of Michigan.
Katherine Rosenblum, University of Michigan.
Maria Muzik, University of Michigan.
References
- Ainsworth MDS, Blehar MC, Waters E, Wall S. Patterns of attachment: A psychological study of the strange situation. Oxford England: Lawrence Erlbaum; 1978. [Google Scholar]
- Allison PD. Missing data techniques for structural equation modeling. Journal of Abnormal Psychology. 2003;112(4):545–557. doi: 10.1037/0021-843X.112.4.545. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual for mental disorders. 4. Washington, DC US: American Psychiatric Press; 2000. text revision (DSM-IV-TR) [Google Scholar]
- Aoki Y, Zeanah CH, Heller SS, Bakshi S. Parent–infant relationship global assessment scale: A study of its predictive validity. Psychiatry and Clinical Neurosciences. 2002;56(5):493–497. doi: 10.1046/j.1440-1819.2002.01044.x. [DOI] [PubMed] [Google Scholar]
- Arata CM. Child Sexual Abuse and Sexual Revictimization. Clinical Psychology: Science and Practice. 2002;9(2):135–164. doi: 10.1093/clipsy.9.2.135. [DOI] [Google Scholar]
- Banyard VL. The impact of childhood sexual abuse and family functioning on four dimensions of women’s later parenting. Child Abuse & Neglect. 1997;21(11):1095–1107. doi: 10.1016/s0145-2134(97)00068-9. [DOI] [PubMed] [Google Scholar]
- Barnes JE, Noll JG, Putnam FW, Trickett PK. Sexual and physical revictimization among victims of severe childhood sexual abuse. Child Abuse & Neglect. 2009;33(7):412–420. doi: 10.1016/j.chiabu.2008.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck CT, Gable RK. Postpartum Depression Screening Scale: development and psychometric testing. Nursing Research. 2000;49(5):272–282. doi: 10.1097/00006199-200009000-00006. [DOI] [PubMed] [Google Scholar]
- Beebe DW. Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatric Clinics of North America. 2011;58(3):649–665. doi: 10.1016/j.pcl.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeghly M, Fuertes M, Liu C, Delonis MS, Tronick E. Maternal Sensitivity: A Foundation for Clinical Practice. Hauppauge, NY: Nova Science; 2011. Maternal sensitivity in dyadic context: mutual regulation, meaning-making, and reparation. [Google Scholar]
- Beeghly Marjorie. Translational research on early language development: current challenges and future directions. Development and Psychopathology. 2006;18(3):737–757. doi: 10.1017/s0954579406060366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beitchman JH, Zucker KJ, Hood JE, DaCosta GA. A review of the long-term effects of child sexual abuse. Child Abuse & Neglect. 1992;16(1):101–118. doi: 10.1016/0145-2134(92)90011-F. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L. Childhood Trauma Questionnaire: A retrospective self-report. Harcourt Brace & Company; 1998. [Google Scholar]
- Bernstein David P, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Blair C, Granger DA, Kivlighan KT, Mills-Koonce R, Willoughby M, Greenberg MT, Hibel LC, et al. Maternal and child contributions to cortisol response to emotional arousal in young children from low-income, rural communities. Developmental Psychology. 2008;44(4):1095–1109. doi: 10.1037/0012-1649.44.4.1095. [DOI] [PubMed] [Google Scholar]
- Bosquet Enlow M, Kitts RL, Blood E, Bizarro A, Hofmeister M, Wright RJ. Maternal posttraumatic stress symptoms and infant emotional reactivity and emotion regulation. Infant Behavior & Development. 2011;34(4):487–503. doi: 10.1016/j.infbeh.2011.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand SR, Brennan PA, Newport DJ, Smith AK, Weiss T, Stowe ZN. The impact of maternal childhood abuse on maternal and infant HPA axis function in the postpartum period. Psychoneuroendocrinology. 2010;35(5):686–693. doi: 10.1016/j.psyneuen.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand SR, Engel SM, Canfield RL, Yehuda R. The effect of maternal PTSD following in utero trauma exposure on behavior and temperament in the 9-month-old infant. Annals of the New York Academy of Sciences. 2006;1071:454–458. doi: 10.1196/annals.1364.041. [DOI] [PubMed] [Google Scholar]
- Braungart-Rieker JM, Garwood MM, Powers BP, Wang X. Parental sensitivity, infant affect, and affect regulation: predictors of later attachment. Child Development. 2001;72(1):252–270. doi: 10.1111/1467-8624.00277. [DOI] [PubMed] [Google Scholar]
- Brennan PA, Pargas R, Walker EF, Green P, Newport DJ, Stowe Z. Maternal depression and infant cortisol: influences of timing, comorbidity and treatment. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2008;49(10):1099–1107. doi: 10.1111/j.1469-7610.2008.01914.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, Cudeck MR. Alternative Ways of Assessing Model Fit. In: Bollen Kenneth A, Scott Long J., editors. Testing Structural Equation Models. 1993. pp. 136–159. [Google Scholar]
- Caldwell JG, Shaver PR, Li CS, Minzenberg MJ. Childhood Maltreatment, Adult Attachment, and Depression as Predictors of Parental Self-Efficacy in At-Risk Mothers. Journal of Aggression, Maltreatment & Trauma. 2011;20(6):595–616. doi: 10.1080/10926771.2011.595763. [DOI] [Google Scholar]
- Calkins SD. Origins and outcomes of individual differences in emotion regulation. Monographs of the Society for Research in Child Development. 1994;59(2–3):53–72. [PubMed] [Google Scholar]
- Calkins SD, Degnan KA. Temperament in Early Development. In: Ammerman RT, editor. Comprehensive handbook of Personality and Psychopathology. Vol. 3. Hoboken, NJ, USA: John Wiley & Sons; 2006. pp. 64–84. [Google Scholar]
- Cassidy J, Mohr JJ. Unsolvable Fear, Trauma, and Psychopathology: Theory, Research, and Clinical Considerations Related to Disorganized Attachment Across the Life Span. Clinical Psychology: Science and Practice. 2001;8(3):275–298. doi: 10.1093/clipsy.8.3.275. [DOI] [Google Scholar]
- Charmandari E, Tsigos C, Chrousos G. Endocrinology of the stress response. Annual Review of Physiology. 2005;67:259–284. doi: 10.1146/annurev.physiol.67.040403.120816. [DOI] [PubMed] [Google Scholar]
- Chemtob CM, Nomura Y, Rajendran K, Yehuda R, Schwartz D, Abramovitz R. Impact of maternal posttraumatic stress disorder and depression following exposure to the September 11 attacks on preschool children’s behavior. Child Development. 2010;81(4):1129–1141. doi: 10.1111/j.1467-8624.2010.01458.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. The impact of child maltreatment and psychopathology on neuroendocrine functioning. Development and Psychopathology. 2001;13(4):783–804. [PubMed] [Google Scholar]
- Clark R. The parent-child early relational assessment: A factorial validity study. Educational and psychological measurement. 1999;59(5):821–846. doi: 10.1177/00131649921970161. [DOI] [Google Scholar]
- Clark GN, Seifer R. Assessment of parents’ interactions with their developmentally delayed infants. Infant Mental Health Journal. 1985;6(4):214–225. doi: 10.1002/1097-0355(198524)6:4<214::AID-IMHJ2280060406>3.0.CO;2-3. [DOI] [Google Scholar]
- Cole PM, Woolger C, Power TG, Smith KD. Parenting difficulties among adult survivors of father-daughter incest. Child Abuse & Neglect. 1992;16(2):239–249. doi: 10.1016/0145-2134(92)90031-l. [DOI] [PubMed] [Google Scholar]
- Cole Pamela M, Zahn-Waxler C, Fox NA, Usher BA, Welsh JD. Individual differences in emotion regulation and behavior problems in preschool children. Journal of Abnormal Psychology. 1996;105(4):518–529. doi: 10.1037/0021-843X.105.4.518. [DOI] [PubMed] [Google Scholar]
- Connell AM, Goodman SH. The association between psychopathology in fathers versus mothers and children’s internalizing and externalizing behavior problems: a meta-analysis. Psychological Bulletin. 2002;128(5):746–773. doi: 10.1037/0033-2909.128.5.746. [DOI] [PubMed] [Google Scholar]
- Copeland D, Harbaugh BL. Differences in parenting stress between married and single first time mothers at six to eight weeks after birth. Issues in Comprehensive Pediatric Nursing. 2005;28(3):139–152. doi: 10.1080/01460860500227556. [DOI] [PubMed] [Google Scholar]
- Corbett BA, Schupp C, Simon D, Ryan N, Mendoza S. Elevated cortisol during play is associated with age and social engagement in children with autism. Molecular Autism. 2010;1(13):1–12. doi: 10.1186/2040-2392-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crittenden PM. Abusing, neglecting, problematic, and adequate dyads: Differentiating by patterns of interaction. Merrill-Palmer Quarterly. 1981;27(3):201–218. [Google Scholar]
- Davis EP, Snidman N, Wadhwa PD, Glynn LM, Schetter CD, Sandman CA. Prenatal Maternal Anxiety and Depression Predict Negative Behavioral Reactivity in Infancy. Infancy. 2004;6(3):319–331. doi: 10.1207/s15327078in0603_1. [DOI] [Google Scholar]
- Dayton CJ, Levendosky AA, Davidson WS, Bogat GA. The child as held in the mind of the mother: The influence of prenatal maternal representations on parenting behaviors. Infant Mental Health Journal. 2010;31(2):220–241. doi: 10.1002/imhj.20253. [DOI] [PubMed] [Google Scholar]
- Desai S, Arias I, Thompson MP, Basile KC. Childhood victimization and subsequent adult revictimization assessed in a nationally representative sample of women and men. Violence and Victims. 2002;17(6):639–653. doi: 10.1891/vivi.17.6.639.33725. [DOI] [PubMed] [Google Scholar]
- Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: a theoretical integration and synthesis of laboratory research. Psychological Bulletin. 2004;130(3):355–391. doi: 10.1037/0033-2909.130.3.355. [DOI] [PubMed] [Google Scholar]
- DiLillo D, Tremblay GC, Peterson L. Linking childhood sexual abuse and abusive parenting: the mediating role of maternal anger. Child Abuse & Neglect. 2000;24(6):767–779. doi: 10.1016/s0145-2134(00)00138-1. [DOI] [PubMed] [Google Scholar]
- Earls L, Muzik M, Beeghly M. Maternal and Infant Behavior Coding Manual. 2009. [Google Scholar]
- Edhborg M, Seimyr L, Lundh W, Widström AM. Fussy child - difficult parenthood? Comparisons between families with a “depressed” mother and non-depressed mother 2 months postpartum. Journal of Reproductive and Infant Psychology. 2000;18(3):225–238. doi: 10.1080/713683036. [DOI] [Google Scholar]
- Egeland B, Hiester M. The long-term consequences of infant day-care and mother-infant attachment. Child Development. 1995;66(2):474–485. doi: 10.2307/1131591. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Spinrad TL, Eggum NM, Silva KM, Reiser M, Hofer C, Smith CL, et al. Relations among maternal socialization, effortful control, and maladjustment in early childhood. Development and Psychopathology. 2010;22(3):507–525. doi: 10.1017/S0954579410000246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feerick M, Snow K. The Relationships Between Childhood Sexual Abuse, Social Anxiety, and Symptoms of Posttraumatic Stress Disorder in Women. Journal of Family Violence. 2005;20(6):409–419. doi: 10.1007/s10896-005-7802-z. [DOI] [Google Scholar]
- Feldman R. Unpublished manual. Bar-Ilan University; 1998. Coding Interactive Behavior (CIB) manual. [Google Scholar]
- Feldman Ruth, Granat A, Pariente C, Kanety H, Kuint J, Gilboa-Schechtman E. Maternal depression and anxiety across the postpartum year and infant social engagement, fear regulation, and stress reactivity. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48(9):919–927. doi: 10.1097/CHI.0b013e3181b21651. [DOI] [PubMed] [Google Scholar]
- Feng X, Shaw DS, Skuban EM, Lane T. Emotional exchange in mother-child dyads: stability, mutual influence, and associations with maternal depression and child problem behavior. Journal of Family Psychology: JFP: Journal of the Division of Family Psychology of the American Psychological Association (Division 43) 2007;21(4):714–725. doi: 10.1037/0893-3200.21.4.714. [DOI] [PubMed] [Google Scholar]
- Field T, Diego M, Hernandez-Reif M. Depressed mothers’ infants are less responsive to faces and voices. Infant Behavior & Development. 2009;32(3):239–244. doi: 10.1016/j.infbeh.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgerald MM, Shipman KL, Jackson JL, McMahon RJ, Hanley HM. Perceptions of parenting versus parent-child interactions among incest survivors. Child Abuse & Neglect. 2005;29(6):661–681. doi: 10.1016/j.chiabu.2004.10.012. [DOI] [PubMed] [Google Scholar]
- Forbes EE, Cohn JF, Allen NB, Lewinsohn PM. Infant Affect during Parent-Infant Interaction at 3 and 6 Months: Differences Between Mothers and Fathers and Influence of Parent History of Depression. Infancy: The Official Journal of the International Society on Infant Studies. 2004;5(1):61–84. doi: 10.1207/s15327078in0501_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortunato CK. Unpublished doctoral dissertation. The Pennsylvania State University; 2009. Patterns of adrenocortical reactivity and recovery to emotional challenges in early childhood: Relations to child temperament and parenting quality. [Google Scholar]
- Gelfand DM, Teti DM. The effects of maternal depression on children. Clinical Psychology Review. 1990;10(3):329–353. doi: 10.1016/0272-7358(90)90065-I. [DOI] [Google Scholar]
- Gladstone GL, Parker GB, Mitchell PB, Malhi GS, Wilhelm K, Austin MP. Implications of childhood trauma for depressed women: An analysis of pathways from childhood sexual abuse to deliberate self-harm and revictimization. The American Journal of Psychiatry. 2004;161(8):1417–1425. doi: 10.1176/appi.ajp.161.8.1417. [DOI] [PubMed] [Google Scholar]
- Goodman SH. Depression in mothers. Annual Review of Clinical Psychology. 2007;3:107–135. doi: 10.1146/annurev.clinpsy.3.022806.091401. [DOI] [PubMed] [Google Scholar]
- Goossens FA, Melhuish EC. On the ecological validity of measuring the sensitivity of professional caregivers: The laboratory versus the nursery. European Journal of Psychology Education. 1996;11(2):169–176. [Google Scholar]
- Granger DA, Cicchetti D, Rogosch FA, Hibel LC, Teisl M, Flores E. Blood contamination in children’s saliva: Prevalence, stability, and impact on the measurement of salivary cortisol, testosterone, and dehydroepiandrosterone. Psychoneuroendocrinology. 2007;32(6):724–733. doi: 10.1016/j.psyneuen.2007.05.003. [DOI] [PubMed] [Google Scholar]
- Granger DA, Stansbury K, Henker B. Preschoolers’ behavioral and neuroendocrine responses to social challenge. Merrill-Palmer Quarterly: Journal of Developmental Psychology. 1994;40(2):190–211. [Google Scholar]
- Granger DA, Weisz JR, McCracken JT, Ikeda SC. Reciprocal influences among adrenocortical activation, psychosocial processes, and the behavioral adjustment of clinic-referred children. Child Development. 1996;67(6):3250–3262. [PubMed] [Google Scholar]
- Gross JJ. Handbook of Emotion Regulation. Guilford Press; 2009. [Google Scholar]
- Gunnar MR, Larson MC, Hertsgaard L, Harris ML, Brodersen L. The stressfulness of separation among nine-month-old infants: effects of social context variables and infant temperament. Child Development. 1992;63(2):290–303. [PubMed] [Google Scholar]
- Gunnar Megan R, Brodersen L, Krueger K, Rigatuso J. Dampening of Adrenocortical Responses during Infancy: Normative Changes and Individual Differences. Child Development. 1996;67(3):877–889. doi: 10.1111/j.1467-8624.1996.tb01770.x. [DOI] [PubMed] [Google Scholar]
- Gunnar Megan R, Donzella B. Social regulation of the cortisol levels in early human development. Psychoneuroendocrinology. 2002;27(1–2):199–220. doi: 10.1016/s0306-4530(01)00045-2. [DOI] [PubMed] [Google Scholar]
- Haley DW, Stansbury K. Infant stress and parent responsiveness: regulation of physiology and behavior during still-face and reunion. Child Development. 2003;74(5):1534–1546. doi: 10.1111/1467-8624.00621. [DOI] [PubMed] [Google Scholar]
- Hammen C, Burge D, Adrian C. Timing of mother and child depression in a longitudinal study of children at risk. Journal of Consulting and Clinical Psychology. 1991;59(2):341–345. doi: 10.1037//0022-006x.59.2.341. [DOI] [PubMed] [Google Scholar]
- Hammen Constance, Shih JH, Brennan PA. Intergenerational transmission of depression: test of an interpersonal stress model in a community sample. Journal of Consulting and Clinical Psychology. 2004;72(3):511–522. doi: 10.1037/0022-006X.72.3.511. [DOI] [PubMed] [Google Scholar]
- Huot RL, Brennan PA, Stowe ZN, Plotsky PM, Walker EF. Negative affect in offspring of depressed mothers is predicted by infant cortisol levels at 6 months and maternal depression during pregnancy, but not postpartum. Annals of the New York Academy of Sciences. 2004;1032:234–236. doi: 10.1196/annals.1314.028. [DOI] [PubMed] [Google Scholar]
- Jacobvitz D, Leon K, Hazen N. Does expectant mothers’ unresolved trauma predict frightened/frightening maternal behavior? Risk and protective factors. Development and Psychopathology. 2006;18(2):363–379. doi: 10.1017/S0954579406060196. [DOI] [PubMed] [Google Scholar]
- Jansen J, Beijers R, Riksen-Walraven M, de Weerth C. Cortisol reactivity in young infants. Psychoneuroendocrinology. 2010;35(3):329–338. doi: 10.1016/j.psyneuen.2009.07.008. [DOI] [PubMed] [Google Scholar]
- Jansen PW, Saridjan NS, Hofman A, Jaddoe VWV, Verhulst FC, Tiemeier H. Does disturbed sleeping precede symptoms of anxiety or depression in toddlers? The generation R study. Psychosomatic Medicine. 2011;73(3):242–249. doi: 10.1097/PSY.0b013e31820a4abb. [DOI] [PubMed] [Google Scholar]
- Kogan N, Carter AS. Mother-infant reengagement following the still-face: The role of maternal emotional availability an infant affect regulation. Infant Behavior and Development. 1996;19(3):359–370. [Google Scholar]
- Kopp CB. Regulation of distress and negative emotions: A developmental view. Developmental Psychology. 1989;25(3):343–354. doi: 10.1037/0012-1649.25.3.343. [DOI] [Google Scholar]
- Levendosky AA, Graham-Bermann SA. Parenting in Battered Women: The Effects of Domestic Violence on Women and Their Children. Journal of Family Violence. 2001;16(2):171–192. doi: 10.1023/A:1011111003373. [DOI] [Google Scholar]
- Linver MR, Brooks-Gunn J, Kohen DE. Family processes as pathways from income to young children’s development. Developmental Psychology. 2002;38(5):719–734. [PubMed] [Google Scholar]
- Lipman EL, MacMillan HL, Boyle MH. Childhood abuse and psychiatric disorders among single and married mothers. The American Journal of Psychiatry. 2001;158(1):73–77. doi: 10.1176/appi.ajp.158.1.73. [DOI] [PubMed] [Google Scholar]
- Loman MM, Gunnar MR. Early experience and the development of stress reactivity and regulation in children. Neuroscience and Biobehavioral Reviews. 2010;34(6):867–876. doi: 10.1016/j.neubiorev.2009.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: a meta-analytic review. Clinical Psychology Review. 2000;20(5):561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Luijk MPCM, Velders FP, Tharner A, van Ijzendoorn MH, Bakermans-Kranenburg MJ, Jaddoe VWV, Hofman A, et al. FKBP5 and resistant attachment predict cortisol reactivity in infants: gene-environment interaction. Psychoneuroendocrinology. 2010;35(10):1454–1461. doi: 10.1016/j.psyneuen.2010.04.012. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Bronfman E, Parsons E. Atypical attachment in infancy and early childhood among children at developmental risk. IV. Maternal frightened, frightening, or atypical behavior and disorganized infant attachment patterns. Monographs of the Society for Research in Child Development. 1999;64(3):67–96. doi: 10.1111/1540-5834.00034. discussion 213–220. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Zoll D, Connell D, Grunebaum HU. The depressed mother and her one-year-old infant: environment, interaction, attachment, and infant development. New Directions for Child Development. 1986;(34):61–82. doi: 10.1002/cd.23219863407. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K. Maternal depressive symptoms, disorganized infant-mother attachment relationships and hostile-aggressive behavior in the preschool classroom: a prospective longitudinal view from infancy to age five. In: Cicchetti D, Toth S, editors. Developmental Perspectives on Depression. Rochester, NY US: University of Rochester Press; 1992. pp. 131–169. [Google Scholar]
- Lyons-Ruth Karlen, Block D. The disturbed caregiving system: Relations among childhood trauma, maternal caregiving, and infant affect and attachment. Infant Mental Health Journal. 1996;17(3):257–275. doi: 10.1002/(SICI)1097-0355(199623)17:3<257::AID-IMHJ5>3.0.CO;2-L. [DOI] [Google Scholar]
- Main M, Hesse E. Attachment in the preschool years: Theory, research, and intervention. Chicago, IL, US: University of Chicago Press; 1990. Parents’ unresolved traumatic experiences are related to infant disorganized attachment status: Is frightened and/or frightening parental behavior the linking mechanism? pp. 161–182. The John D. and Catherine T. MacArthur Foundation series on mental health and development. [Google Scholar]
- Meijssen D, Wolf MJ, Koldewijn K, Houtzager BA, van Wassenaer A, Tronick E, Kok J, et al. The effect of the Infant Behavioral Assessment and Intervention Program on mother-infant interaction after very preterm birth. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2010;51(11):1287–1295. doi: 10.1111/j.1469-7610.2010.02237.x. [DOI] [PubMed] [Google Scholar]
- Mesman J, van IJzendoorn MH, Bakermans-Kranenburg MJ. The many faces of the Still-Face Paradigm: A review and meta-analysis. Developmental Review. 2009;29(2):120–162. doi: 10.1016/j.dr.2009.02.001. [DOI] [Google Scholar]
- Meyer B, Johnson SL, Winters R. Responsiveness to threat and incentive in bipolar disorder: Relations of the BIS/BAS scales with symptoms. Journal of Psychopathology and Behavioral Assessment. 2001;23(3):133–143. doi: 10.1023/A:1010929402770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. 1998–2007. Mplus User’s Guide. Los Angeles, CA: Muthén & Muthén; 2007. [Google Scholar]
- Neu M, Robinson J. Maternal holding of preterm infants during the early weeks after birth and dyad interaction at six months. Journal of Obstetric, Gynecologic, and Neonatal Nursing: JOGNN/NAACOG. 2010;39(4):401–414. doi: 10.1111/j.1552-6909.2010.01152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obel C, Hedegaard M, Henriksen TB, Secher NJ, Olsen J, Levine S. Stress and salivary cortisol during pregnancy. Psychoneuroendocrinology. 2005;30(7):647–656. doi: 10.1016/j.psyneuen.2004.11.006. [DOI] [PubMed] [Google Scholar]
- Pauli-Pott U, Mertesacker B, Beckmann D. Predicting the development of infant emotionality from maternal characteristics. Development and Psychopathology. 2004;16(1):19–42. [PubMed] [Google Scholar]
- Reissland N, Shepherd J, Herrera E. Teasing play in infancy: Comparing mothers with and without self-reported depressed mood during play with their babies. European Journal of Developmental Psychology. 2005;2(3):271–283. doi: 10.1080/17405620444000319. [DOI] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology. 1993;61(6):984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Robinson C, Mandleco B, Olsen S, Hart C. Authoritative, Authoritarian, and Permissive Parenting Practices - Development of a New Measure. Psychological Reports. 1995;77(3):819–830. [Google Scholar]
- Rueda MR, Rothbart MK. The influence of temperament on the development of coping: The role of maturation and experience. New Directions for Child and Adolescent Development. 2009;2009(124):19–31. doi: 10.1002/cd.240. [DOI] [PubMed] [Google Scholar]
- Sameroff A. A unified theory of development: a dialectic integration of nature and nurture. Child Development. 2010;81(1):6–22. doi: 10.1111/j.1467-8624.2009.01378.x. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ, Fiese BH. Transactional Regulation: The Developmental Ecology of Early Intervention. In: Shonkoff Jack P, Meisels Samuel J., editors. Handbook of Early Childhood Intervention. Cambridge University Press; 2000. pp. 134–158. [Google Scholar]
- Schechter DS, Davis B. Parenting in times of crisis. Psychiatric Annals. 2007;37(6):423. doi: 10.3928/0090-4481-20070401-11. [DOI] [PubMed] [Google Scholar]
- Scher CD, Forde DR, McQuaid JR, Stein MB. Prevalence and demographic correlates of childhood maltreatment in an adult community sample. Child Abuse & Neglect. 2004;28(2):167–180. doi: 10.1016/j.chiabu.2003.09.012. [DOI] [PubMed] [Google Scholar]
- Schore AN. Affect dysregulation & disorders of the self. SciELO Brasil; 2003. Retrieved from http://www.scielo.br/pdf/rprs/v28n3/v28n3a19.pdf. [Google Scholar]
- Schuetze P, Lopez FA, Granger DA, Eiden RD. The association between prenatal exposure to cigarettes and cortisol reactivity and regulation in 7-month-old infants. Developmental Psychobiology. 2008;50(8):819–834. doi: 10.1002/dev.20334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng JS, Low LK, Sperlich M, Ronis DL, Liberzon I. Prevalence, trauma history, and risk for posttraumatic stress disorder among nulliparous women in maternity care. Obstetrics and Gynecology. 2009;114(4):839–847. doi: 10.1097/AOG.0b013e3181b8f8a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sroufe LA, et al. Psychopathology as an outcome of development. Development and Psychopathology. 1997;9:251–268. doi: 10.1017/s0954579497002046. [DOI] [PubMed] [Google Scholar]
- Tees MT, Harville EW, Xiong X, Buekens P, Pridjian G, Elkind-Hirsch K. Hurricane Katrina-related maternal stress, maternal mental health, and early infant temperament. Maternal and Child Health Journal. 2010;14(4):511–518. doi: 10.1007/s10995-009-0486-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson RA. Emotion regulation: a theme in search of definition. Monographs of the Society for Research in Child Development. 1994;59(2–3):25–52. [PubMed] [Google Scholar]
- Tronick E, Als H, Adamson L, Wise S, Brazelton TB. The infant’s response to entrapment between contradictory messages in face-to-face interaction. Journal of the American Academy of Child Psychiatry. 1978;17(1):1–13. doi: 10.1016/s0002-7138(09)62273-1. [DOI] [PubMed] [Google Scholar]
- Tronick Ed, Beeghly M. Infants’ meaning-making and the development of mental health problems. The American Psychologist. 2011;66(2):107–119. doi: 10.1037/a0021631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberg M Katherine, Olson KL, Beeghly M, Tronick EZ. Making up is hard to do, especially for mothers with high levels of depressive symptoms and their infant sons. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2006;47(7):670–683. doi: 10.1111/j.1469-7610.2005.01545.x. [DOI] [PubMed] [Google Scholar]
- Weinberg MK, Tronick EZ, Cohn JF, Olson KL. Gender differences in emotional expressivity and self-regulation during early infancy. Developmental Psychology. 1999;35(1):175–188. doi: 10.1037//0012-1649.35.1.175. [DOI] [PubMed] [Google Scholar]
- Widaman KF. III. MISSING DATA: WHAT TO DO WITH OR WITHOUT THEM. Monographs of the Society for Research in Child Development. 2006;71(3):42–64. doi: 10.1111/j.1540-5834.2006.00404.x. [DOI] [Google Scholar]
- Wolfe J, Kimerling R. Assessing psychological trauma and PTSD. New York: Guilford Press; 1997. Gender issues in the assessment of Posttraumatic Stress Disorder; pp. 192–238. [Google Scholar]
- Yehuda R, Bierer LM. Transgenerational transmission of cortisol and PTSD risk. Progress in Brain Research. 2008;167:121–135. doi: 10.1016/S0079-6123(07)67009-5. [DOI] [PubMed] [Google Scholar]


