Abstract
Objective
Parents’ emotional, cognitive, and behavioral responses are highly influential upon children’s pain and functional outcomes. One important response to pediatric pain is acceptance: the degree to which an individual participates in routine daily activities in the presence of pain and is willing to let pain be a part of their life without efforts to control or avoid it. However, no tool currently exists to assess parents’ own acceptance of their child’s pain. The aim of this study was to validate the Parent Pain Acceptance Questionnaire (PPAQ).
Method
The PPAQ was administered to 310 parents of youth with chronic pain in an outpatient pediatric headache program and a day hospital pain rehabilitation program. An exploratory factor analysis revealed two factors for the PPAQ: an 11-item Activity Engagement scale and a 4-item Acceptance of Pain-Related Thoughts & Feelings scale.
Results
The PPAQ total score and subscales demonstrated strong internal consistency. Greater parent pain acceptance was positively associated with child pain acceptance, and was negatively correlated with parent protective behaviors, parent minimizing behaviors, parent and child pain catastrophizing, and child fear of pain. Parent protective behaviors and child pain acceptance both served as mediators of the relationship between parent pain acceptance and child functional disability.
Conclusions
The PPAQ is a valid measure of parent pain acceptance and may provide valuable insights into parent responses to child pain and the ways in which parent acceptance influences child outcomes. Clinical implications and suggestions for future research are discussed.
Keywords: Pain Acceptance, Pediatric Chronic Pain, Parents, Pain in Children
Introduction
Pediatric chronic pain occurs within a social context. A growing body of research demonstrates that parents’ emotional, cognitive, and behavioral responses are highly influential upon children’s pain and functional outcomes [1–4]. Because of the relevance of parent factors, researchers have developed a number of measures assessing parent beliefs and behaviors in the context of pediatric pain (e.g., Pain Catastrophizing Scale for Parents (PCS-P; [5]), Adult Responses to Children's Symptoms (ARCS; [6]); Parent Psychological Flexibility Questionnaire (PPFQ; [7]). In fact, after a comprehensive review, Jordan and colleagues concluded that continued development of multidimensional, theoretically-driven measures specific to concerns of parents of youth with persistent pain are necessary [8]. Such measures allow the exploration of the extent to which parent factors impact child pain-related outcomes.
One potentially influential construct is the degree to which a parent can willingly accept the presence and persistence of pain in their child’s life and continue to participate fully in their own day-to-day life. This is defined here as parent pain acceptance. Although applying the concept of pain acceptance to parents of youth with pain is relatively new, pain acceptance within an individual with pain has existed for some time. Research has demonstrated that a high level of pain acceptance is associated with less distress and disability in adults [9–11] and adolescents [12, 13] suffering with chronic pain. Further, acceptance-based treatment approaches (i.e., those that foster functional improvement by encouraging patients to pursue their values in the presence of pain) have proven effective for both adults [14, 15] and adolescents [13].
Given the established importance of pain acceptance on outcomes, in combination with what is known broadly about parental influences on child pain-related functioning, we modified the items on the Chronic Pain Acceptance Questionnaire-Parent Report [16] to develop a related measure that assesses parents’ own acceptance of their child’s pain. Specifically, parent pain acceptance refers to a parent participating in their own daily life activities in the presence of the child’s pain (e.g., “I lead a full life even though my child has a chronic pain”) and permitting their child’s pain to be a part of their life experience without focusing their efforts on controlling or avoiding it, when these efforts conflict with parent and family values (e.g., “I must keep my feelings about my child’s pain under control whenever I do something” – reverse coded). Asking parents to report on their own acceptance of their child’s pain is particularly relevant given that a common experience shared by parents of children with chronic pain is parents’ sense of being unable to progress with their own lives due to the uncertainty of living with their child’s pain condition [8].
The primary goal of this study is to introduce a measure to assess parent pain acceptance (the Parent Pain Acceptance Questionnaire; PPAQ). In addition to testing the psychometric properties of the PPAQ through exploration of its factor structure, internal consistency, and item content, we will examine the influence of parent acceptance on child pain-related functioning, through two potential mediating variables (e.g., parent protective behaviors and child pain acceptance). We believe that level of pain acceptance will influence these two variables, both of which are known to predict child functional outcomes.
We hypothesized that the PPAQ would be a psychometrically strong measure consisting of two subscales: activity engagement and pain willingness, consistent with the measures from which it was derived. With regards to the measure’s construct validity, we hypothesized that greater parent acceptance of child pain would be negatively correlated with parent pain catastrophizing, and parent protective and minimizing responses, thus comparable to findings in youth [17, 18]. With regard to child pain-related functioning, we hypothesized that parent pain acceptance would be associated with higher child pain acceptance and lower levels of child pain catastrophizing and pain-related fear, and in turn, less pain-related functional disability [11]. Lastly, given the consistently weak correlation between child pain acceptance and child pain ratings [17, 19], we anticipated a weak relationship between parent acceptance and child pain ratings.
Materials & Methods
Participants
Patients aged 8–17 and an identified parent who underwent a multidisciplinary pain evaluation within the context of large, urban northeast US pediatric hospital between September 2011 and October 2013 were eligible for the study. These evaluations were conducted at two sites within the hospital: 1) an outpatient headache clinic and b) a day hospital pain rehabilitation program. Altogether, 313 of the 350 families approached consented to participate (89% participation rate). Primary reasons for refusal were lack of interest or time.
The final sample of those with sufficient data included 310 patient/parent dyads (as three participant dyads had significant missing data and were thus excluded). Of these, 206 were from the outpatient headache clinic and 104 were from the pain rehabilitation program. The patient/parent dyads were primarily white (91.9%). The patient sample was predominantly female (75.2%), with a mean age of 13.80 years (SD = 2.69), which is reflective of the population of youth commonly seen in this tertiary care clinic setting.
The parent sample consisted of predominantly mothers. Most parent participants were married (80.5%), and many were well educated (i.e., 67.5% of mothers and 59.6% of fathers were college graduates or higher). Family socioeconomic status (SES) based on the four-factor index of social status [19] ranged from 12 (semi-skilled workers) to 66 (business owner; professional), with a mean of 47.58 (minor professional; technical) (SD = 13.27). The two recruitment sites demonstrated statistically significant differences with regard to SES; parents completing evaluations at the day hospital pain rehabilitation program reporting higher SES (M=50.77, SD=11.44) than those completing evaluations at the pediatric headache program (M=46.27, SD=13.78). Categorically, however, both group means are considered to fall in the minor professional/technical SES group such that this statistical difference does not appear to be clinically meaningful. There were no additional differences between the two sites in terms of child or parent demographic characteristics.
Physician-assigned pain diagnoses included the following: headaches (68.7%; including migraine headaches, tension-type headaches, persistent daily headaches, post-concussive headaches, combination headaches, and other cranial neuropathies), neuropathic pain (24.2%; including complex regional pain syndrome and other neuralgia), and non-neuropathic pain (7.1%; including musculoskeletal pain and functional abdominal pain).
At the time of the evaluation, patients’ mean duration of pain was greater than two years, median pain duration = 15.66 months (SD = 33.28, range = 1–194 months), with less than 5% experiencing pain symptoms for less than 3 months at the time of this assessment. There were no significant differences in parent acceptance of child pain when child pain was acute vs. chronic. When the small subset of parents of youth with pain for less than three months was removed from analyses, all findings remained consistent. Of note, there were significant subsample differences between recruitment sites in terms of typical pain rating and pain duration. Parents completing evaluations at the day hospital pain rehabilitation program had youth who reported greater typical pain ratings (p < .001) but shorter pain duration (p <.001) than youth of parents completing evaluations at the pediatric headache program.
Measures
Basic demographic (e.g., age, gender) and medical information (e.g., pain diagnosis, pain duration) was collected from patient charts.
Parent-Report Measures
The Parent Pain Acceptance Questionnaire (PPAQ) is a modified version of the validated Chronic Pain Acceptance Questionnaire (CPAQ) [20]. The CPAQ is a 20-item measure consisting of two subscales: activity engagement (11 items) and pain willingness (9 items). Previous research supports the internal consistency, factor structure, and validity of the CPAQ [20]. To create a parent self-report version of this measure, each item was modified to reflect parents’ acceptance of their child’s pain, with some items also slightly simplified or clarified. For example, item 1 “I am getting on with the business of living no matter what my pain level is” was changed to “I am getting on with life no matter what my child’s pain level is.” Item 7 (reverse coded) “I need to concentrate on getting rid of my pain” was changed to “I need to concentrate on getting rid of my child’s pain” (see Table 1 for final list of items). We also modified the response format of the adult version from a 7-point to a 5-point Likert-type scale (0 = “never true” to 4 = “always true”) for ease of use. Higher scores signify greater parent acceptance of child pain.
The Pain Catastrophizing Scale – Parent Version (PCS-P; [5]) assesses parental negative thinking associated with their child’s pain. It is comprised of 13 items rated on a 5-point Likert-type scale (0 = “not at all true” to 4 = “very true”). Items are summed to derive a total score. Higher scores indicated higher levels of catastrophic thinking. The PCS-P has strong psychometric properties and demonstrated validity with high levels of parent catastrophic thinking about their child’s pain associated with greater emotional distress and a tendency to restrict their child’s activities. The internal consistency for the Total Score in this sample is .95.
The Adult Responses to Children’s Symptoms (ARCS; [6]) assesses parents’ behavioral responses to their children’s pain. Each item queries, “When your child has pain, how often do you…?” Responses are rated on a 5-point Likert-type scale (0 = “never” to 4 = “always”). The parent protectiveness (Protect) and minimization of pain (Minimize) subscales were used in this study, with higher scores representing more frequent use of a particular type of response. Items on the Protect scale (α = .84) refer to protective parental behavior such as giving the child special attention and limiting the child’s normal activities and responsibilities. Items on the Minimize scale ((α = .73) discount and criticize the child’s pain as excessive. Higher protective and minimizing behavior scores have been found to be associated with poor child outcomes [22].
Child-Report Measures
The Chronic Pain Acceptance Questionnaire, Adolescent report (CPAQ-A; [17]) is a self-report inventory used to assess adolescent acceptance of pain. Each item is rated on a 5-point Likert-type scale (0 = “never true” to 4 = “always true.” The CPAQ-A is a 20-item measure consisting of two subscales: activity engagement (11 items) and pain willingness (9 items), as described above. Given that this measure was validated with youth 10 years of age and older, we did not include CPAQ-A data from patients below this age in any of our analyses.
The Fear of Pain Questionnaire, Child report (FOPQ-C; [21]) is a self-report inventory used to assess pain-related fears. Each item is rated on a 5-point Likert-type scale (0 = “strongly disagree” to 4 = “strongly agree”). The FOPQ-C consists of 24 items with strong internal consistency and construct validity [21]. The total FOPQ-C score (α = .94) was used in this study.
The Pain Catastrophizing Scale – Child Version (PCS-C; [23]) assesses negative thinking associated with pain. It is comprised of 13 items rated on a 5-point Likert-type scale (0 = “not at all true” to 4 = “very true”). Items are summed to derive a total score. Higher scores indicated higher levels of catastrophic thinking. The internal consistency for the Total Score on the child version of this measure was .95 in this sample.
The Functional Disability Inventory (FDI; [24, 25]) is a 15-item self-report measure assessing children’s perceived difficulty in physical and psychosocial functioning that is due to physical health. Children rate the degree to which they had any trouble completing activities in the past two weeks on a 5-point Likert-type scale (0 = “no trouble” to 4 = “impossible”). Items are summed for a total score and higher scores represent higher levels of children’s perceived functional disability. The internal consistency for this measure was .91 in this sample.
Finally, as part of a semi-structured interview with the clinical psychologist, children were asked to provide their typical (average) daily pain rating on a standard 11-point numeric rating scale [26] (0 = “no pain” to 10 = “most pain possible”).
Procedure
The study was approved by the hospital’s Institutional Review Board. Study measures were collected in the context of the child’s multidisciplinary pain evaluation with a set of measures that is part of the standard clinical assessment battery (i.e., ARCS, PCS-P, PCS-C, & FDI) and additional measures as part of an IRB-approved study protocol (i.e., CPAQ-A, PPAQ, & FOPQ-C). Questionnaires were mailed to families prior to the child’s evaluation as part of the standard clinical assessment. Parents and children were asked to complete those questionnaires independently and return them on the date of their appointment to aid in the clinical evaluation. If parents or children had not completed these questionnaires upon arrival to their appointment, they were asked to do so prior to the start of the evaluation. Pain ratings were obtained during the clinical psychologist’s interview. Patients and their parents were approached by a research assistant during their evaluation and were asked to consent/assent for the a) IRB approved study and b) to have their responses from the clinical assessment battery be used for research purposes.
Statistical Analyses
Data were analyzed with SPSS version 21 and AMOS version 20. Descriptive statistics, including skew and kurtosis, were conducted to examine underlying assumptions of normality for all variables of interest. Then, item-total correlations were calculated for the PPAQ. Maximum likelihood exploratory factor analysis (EFA) with oblique rotation was conducted to determine the factor structure of this measure. Factor loadings were examined and items with primary factor loadings <.32 were removed. Factor analysis was repeated until a solution was generated in which all items loaded adequately on the empirically derived factors. Factor analytic rule-of-thumb generally suggests 5–10 respondents per item. With 20 items, we have approximately 15 respondents per item for our analyses.
Relations with demographic variables and the construct and criterion validity of the PPAQ were examined with two-tailed bivariate Pearson correlations, chi-square analyses, and one-way ANOVAs. To assess the construct validity of the PPAQ, regression analyses with Preacher and Hayes’ bootstrap script (with n=1000 bootstrap samples) (http://afhayes.com/spss-sas-and-mplus-macros-and-code.html) was employed to assess the indirect effects, specifying a 95% Bias Corrected and Accelerated Confidence Interval (BCACI) [27]. In assessing mediation with this method, the total effect (weight c; a regression coefficient) of an independent variable (IV) on a dependent variable (DV) is composed of a direct effect (weight c’; a regression coefficient) of the IV on the DV and an indirect effect (weight a x b) of the IV on the DV through a proposed mediator (M). Weight a signifies the effects of the IV on the M while weight b reflects the effect of the M on the DV, partialling out the effect of the IV. Mediation is demonstrated if the BCACIs do not contain zero [28]. Typical pain was entered as a control variable, due to its association with our outcome of interest.
Results
Scale item selection and exploratory factor analysis
Each item of the 20-item measure was examined to determine its contribution to the scale. No items violated assumptions of normality (skew and/or kurtosis > 2.0) Next, item-total correlations were conducted, with two items dropped (item 4, “I would gladly give up important things in life to control my child’s pain better,” and item 19, “It’s a relief to realize that I don’t have to change my child’s pain to get on with living life”) (r < .30; criteria outlined by DeVellis [29]). The remaining 18 items were entered into a maximum likelihood factor analysis with oblique rotation. The criterion of eigenvalues >1 resulted in an initial three-factor solution. Two items were dropped (item 14, “Before I can make any serious plans, I have to get some control over my child’s pain,” and item 20, “I struggle to do things when my child has pain”) because both items cross-loaded > .32 on multiple factors. Upon rerunning the analysis, three factors remained, but the third factor was not internally consistent. We reran the model with 16 items and a specified 2-factor criterion. One item loaded below .32 and was removed (item 17, ‘‘I avoid putting my child in situations where their pain might increase”). The factor analysis was run once again with 15 items specifying a 2-factor structure. The two-factor structure was consistent with Cattell’s elbow criteria on the scree plot [30] and the number of hypothesized dimensions we proposed (see factor loadings in Table 1). The final 15-item scale had a Cronbach’s α of .88. Sample mean for the scale was 33.65 (SD = 10.11). PPAQ total scores were normally distributed across the sample. Factor 1, labeled Activity Engagement, contains 11 items (a = .89). Sample mean for the subscale was 23.08 (SD = 7.98). Factor 2, labeled Acceptance of Pain-Related Thoughts and Feelings, contains 4 items (a = .75). Sample mean for this subscale was 10.35 (SD = 3.53). The two subscales are normally distributed and are inter-correlated, yet distinct (r = .51, p < .001).
PPAQ across Demographic and Pain-related Factors
One-way ANOVAs and bivariate Pearson correlations were conducted to examine differences in the PPAQ total scores across demographic and pain-related factors. Given the preponderance of white participants (92%), we did not examine race or ethnicity. No significant differences were detected in parent pain acceptance across child gender or child age. Parent pain acceptance was also modestly associated with level of education for both mothers’ (r = .18, p < .01) and fathers’ (r = .17, p < .01). With regard to child pain-related factors, parent pain acceptance was not significantly associated with typical child pain ratings (r = −.12, p = .05). There was a small positive correlation between parent pain acceptance and the duration of the child’s pain (r = .15, p < .05). When examined separately by the smaller subsamples, these relationships between parent pain acceptance and child pain-related factors both became non-significant. Overall, parents of children entering an intensive rehab setting had lower levels of acceptance of their child’s pain (M=28.61, SD=9.31) than parents of children evaluated in an outpatient headache clinic (M=35.93, SD=9.64), t = 6.01 (283), p < .001.
Construct Validity of the PPAQ
Bivariate Pearson correlations between the PPAQ, parent variables, and child variables are displayed in Table 2. Notably, parent pain acceptance was negatively correlated with parent pain catastrophizing, as well as with parent protective and minimizing. For child variables, parent pain acceptance was positively associated with child pain acceptance, and was negatively correlated with child fear of pain, child pain catastrophizing, and functional disability. When these correlations were examined separately by smaller subsamples, all findings were consistent in terms of significance and direction, though the magnitude of some relationships varied to a small extent.
Regression analyses using mediational models with Preacher and Hayes’ bootstrap script were conducted to examine the direct and indirect effects of parent pain acceptance on child functioning through parent behaviors and child beliefs. Figure 1 depicts the direct (c) and indirect (c’) relationships between the independent variable (parent pain acceptance) and the dependent variable (child functional disability), through two potential mediators (parent protective behaviors and child pain acceptance).
Figure 1.
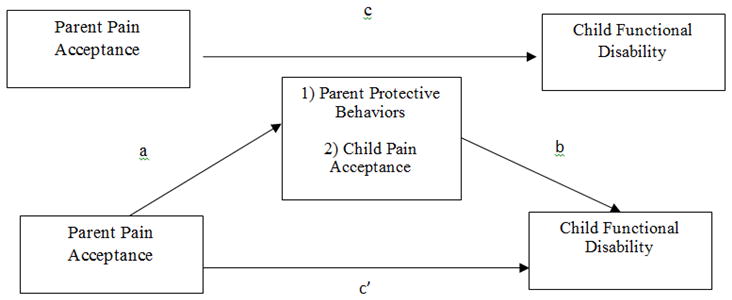
depicts the direct (c) and indirect (c’) relationships between Parent Pain Acceptance (IV) and Child Functional Disability (DV), through two potential mediators, Parent Protective Behaviors and Child Pain Acceptance.
The total effect of parent pain acceptance on child functional disability, path c, was significant, p<.001. Both the effect of parent pain acceptance on parent protective behaviors (path a1, p<.001), and the effect of parent protective behaviors on functional disability (path b1, p< .001) were also significant (see Table 3). With parent protective behaviors in the model, parent pain acceptance continued to be a significant predictor of functional disability (path c’1, p<.01). Bootstrapped results confirmed an indirect effect of parent pain acceptance on functional disability in part explained through parent protective behaviors (BCAC = −.35 – −.08, 95% CI). When analyzed separately by site, the results of the regression analysis described above were comparable across both subsamples. In contrast to the full sample findings, in both subsamples examined separately, with parent protective behaviors in the model, parent pain acceptance was no longer a significant predictor of functional disability.
The effect of parent pain acceptance on child pain acceptance (path a2, p<.001), and the effect of child pain acceptance on functional disability (path b2, p<.001) were also significant (see Table 4). With child pain acceptance in the model, parent pain acceptance was no longer a significant predictor of functional disability (path c’2). Bootstrapped results confirmed an indirect effect of parent pain acceptance on functional disability, explained through child pain acceptance (BCAC = −.32– −.15, 95% CI). Importantly, when analyzed separately by site, the results of the regression analysis described above were consistent across both subsamples, as well as with the findings from the original full sample.
Discussion
The 15-item Parent Pain Acceptance Questionnaire (PPAQ) developed in this study appears to be a psychometrically promising measure for assessing parent’s acceptance of their child’s pain, among parents of youth with chronic pain conditions. With further validation, the PPAQ may serve as a useful tool for both clinicians and researchers seeking to understand the unique parent-related factors that influence pediatric pain outcomes. It may also serve as an important tool for assessing parent change in acceptance-based treatment for youth with chronic pain and their families. Again, however, these results should be considered preliminary until findings are replicated and extended in independent samples.
In the present study, items were administered to a large sample of parents of youth with chronic pain in a pediatric headache clinic and in an intensive pain rehabilitation program. Utilizing maximum likelihood factor analysis, two factors emerged: Activity Engagement and Acceptance of Pain-Related Thoughts and Feelings. The Activity Engagement subscale emerged as hypothesized. However, the initially proposed subscale assessing pain willingness scale did not emerge as expected. What resulted instead was a smaller subset of items that reflected acceptance of the cognitive and emotional aspects of their child’s pain.
All items proposed for the PPAQ were items from a previously validated measure of parents’ perceptions of their child’s pain acceptance (CPAQ-P; [16]), modified to reflect parents’ own acceptance of their child’s pain. Interestingly, several items (n=5) were eliminated during scale refinement. The dropped items centered on parents giving up important things in life, not making plans, and struggling to do things due to their child’s pain. While such constructs appear to be relevant for adults and children who are themselves experiencing pain, they may not extend to the parents of children with pain. It may be that competing responsibilities (e.g., employment, other children) force parents of children with chronic pain to globally continue living life, though their engagement with certain activities may vary. Another item, parents’ avoidance of placing the child in situations where pain might increase, appeared to tap into a construct unrelated to parent acceptance. Taken together, the elimination of these items underscores the importance of developing and validating measures that specifically harness the experience of a parent who has a child in persistent pain, as there may be experiences that are unique to parents of children with chronic pain [8].
PPAQ psychometric properties in this sample were strong and invariant across child gender and age. Greater level of parent education was modestly associated with greater parent pain acceptance; however, the implications of this finding are unclear. One hypothesis may be that parents who are more highly educated have better access to resources (e.g., recommended literature, psycho-education, specialist evaluations) which address directly address the parent role in the treatment of chronic pain (e.g., that specifically that parents should not forgo aspects of their life in lieu of their child’s pain). Relatedly, we previously found a modest positive correlation between SES, as measured by the Hollingshead Index, and parent perceptions of child pain acceptance [16]. Therefore, additional research is necessary to determine if this finding is replicable or clinically meaningful, as most studies have not examined the relationship between education and pain acceptance. Consistent with the weak correlation between child pain acceptance and child pain ratings [17, 19], we found that parent pain acceptance was not significantly associated with their child’s typical pain ratings. This suggests that what governs parents’ activity engagement in the presence of their child’s pain and acceptance of pain-related thoughts and feelings is something other than the child’s reported pain severity.
Longer child pain duration was modestly associated with greater parent pain acceptance, suggesting that parent pain acceptance may increase over time, as parents shift from conceptualizing their child’s pain as needing to be eliminated to needing to be managed. Notably, this finding is in contrast to Simons and colleagues’ [16] finding that parents’ perceptions of child pain acceptance were consistent across pain duration. Further, as we expected, parents of children entering an intensive rehabilitation program had lower levels of acceptance of their child’s pain than parents of children evaluated in an outpatient headache clinic.
Consistent with our hypotheses, the results provide support for the construct validity of the PPAQ. As expected, parent pain acceptance was negatively associated with parent pain catastrophizing and positively associated with child pain acceptance. We also found significant negative associations between parent pain acceptance and parent protective and minimizing behaviors. Finally, with regard to child functioning, parent pain acceptance was negatively associated with fear of pain, pain catastrophizing, and functional disability. Together, these findings suggest that the extent to which parents engage in daily activities and accept their thoughts and feelings related to their child’s pain appear to counter characteristics associated with poor parent (e.g., parent pain catastrophizing) and child (e.g., child fear of pain) outcomes.
We also tested two mediational models to examine the criterion-related validity of the PPAQ and to better understand the nature of relationships between parent pain acceptance and child pain-related functioning. The findings that emerged serve to further delineate the complex associations between parent and child variables in the context of pediatric chronic pain. First, results indicated that parent protective behaviors served as a mediator of the relation between parent pain acceptance and child functional disability. This finding suggests that parents’ engagement in their own activities and their acceptance of pain-related thoughts and feelings are not only associated with their behavioral responses to their child in pain, but also may impact child pain-related functioning. There is considerable evidence supporting the inadvertent negative impact of protective parenting on a child’s ability to function in pain [4]. The mechanism by which parent pain acceptance directly impacts child functioning may be operating in a similar vein; when a child observes their parent struggling with their thoughts and feelings about the pain or observes that their parent is unable to function in their own life due to their child’s pain, they likely take note. As parents serve as important models to on how to cope and respond to stressors [4, 31], it is likely that bolstering parents’ acceptance will likely improve their child’s outcomes.
Finally, child pain acceptance mediated the relationship between parent pain acceptance and child functional disability. This suggests that child pain acceptance is inextricably tied to their parents’ acceptance of their child’s pain, and that together, both influence the child’s functional disability. This is consistent with Palermo and Chambers’ [32] integrative model which conceptualizes family factors in pediatric pain populations. The model demonstrates how parent and child variables occur within the context of dyadic relationships and interact with one another, often synergistically [32, 33]. This finding also supports operant theory suggesting that social modeling is important not only in the development of pediatric pain, but also in child and parent behavioral and emotional responses to pain [34].
The findings of this study must be viewed in light of its limitations. First, the parents in this sample were almost all white mothers, which in itself limits the generalizability of the results. Although this limitation reflects that of most pediatric pain research samples, it is imperative for future research to determine whether parent pain acceptance varies across mothers and fathers. This is relevant, given that recent findings indicate maternal vs. paternal mean differences in another parent pain-related factor: pain catastrophizing [35], particularly with regard to increased maternal rumination about the child’s pain. It is equally imperative for future research to determine whether parent pain acceptance varies across various cultural groups. A growing body of research suggests that, although pain is a universal phenomenon, cultural values may play a significant role in the experience and expression of pain in adults [36, 37], and likely in youth and their parents as well. For instance, some researchers suggest that, in a stoic, ethnically homogeneous society, pain-related impairment may be far less tolerated than in the more liberal, permissive, and pluralistic American society [38]. Relatedly, then, pain acceptance may have different meanings or have different implications in various cultural settings.
Second, although a two-factor solution best fit the data provided by this sample, it is certainly possible that other solutions could be derived with other more diverse samples and this should be examined in future research. Additionally, the PPAQ Acceptance of Pain-Related Thoughts and Feelings subscale consists of just four items. While this subscale is internally consistent (and a single-factor model for the PPAQ resulted in fit deterioration compared to the two-factor model), it is possible that additional relevant items would strengthen the psychometric properties of this subscale and of the PPAQ as a whole. Interestingly, researchers have recently derived an 8-item version of the adult CPAQ, suggesting that perhaps some of the items were either redundant or ill defined. Third, in this cross-sectional investigation, it was only possible to concurrently examine associations between parent and child variables. Longitudinal studies would further aid our understanding of the complex associations between parent variables and pediatric outcomes, by allowing for the investigation of potential causal relationships.
Lastly, a very small percentage (<5%) of the children of parent participants reported experiencing pain for less than three months (i.e., “acute pain”) at the time of the assessment. Although it is possible that this may represent a qualitatively different experience for youth and their families, no differences emerged when comparing this group with the larger chronic pain group.
These findings have several implications for future research among parents of youth with chronic pain. First, as noted previously, the PPAQ requires replication and further validation, particularly through the use of confirmatory factor analysis, in similar samples of parents of youth experiencing chronic pain. Additionally, examining parent pain acceptance in conjunction with conceptually similar questionnaires is an important next step for additional validation of the PPAQ and for more completely understanding the experience of a parent with a child in pain. Such related measures might include the Bath Adolescent Pain-Parent Impact Questionnaire (BAP-PIQ; [39]) which assesses the broad impact of child chronic pain on parents, distress in the context of child pain, or the Parent Psychological Flexibility Questionnaire (PPFQ; [7]), which assesses parent responses consistent with acceptance-based treatment approaches (e.g., present-focused attention, values-based action). Examining parent pain acceptance in conjunction with these parent-specific measures would allow researchers and clinicians to more comprehensively examine how parent cognitive, emotional, and behavioral responses to child pain interact to influence child functioning.
Future studies of pediatric pain should continue to include assessment of parent pain acceptance in order to capture additional mechanisms through which this construct contributes to child outcomes. For example, researchers should examine how parent pain acceptance relates to parent behaviors beyond protective responses, to other variables examining parent distress, and to child outcomes beyond functional disability. Further, while parent pain acceptance is important to explaining child outcomes, other variables should be identified to add to models explaining pediatric pain outcomes.
Overall, it appears that use of the PPAQ can provide valuable insights into the ways in which parent pain acceptance relates to parent responses to child pain, children’s emotional/cognitive and behavioral responses to pain, and above all, their own acceptance of pain. This knowledge may inform future interventions for children with chronic pain and their parents. For instance, additional research may further elucidate the role of parent pain acceptance as an intervention target and delineate therapeutic strategies for facilitating parent acceptance as a means of improving child outcomes. Indeed, acceptance-based approaches continue to emerge as a viable treatment modality for pediatric pain [12, 13, 40, 41]. As such approaches become more prevalent, continued research efforts are needed with regard to both treatment development and evaluation of treatment outcomes, particularly for approaches that engage parents of children with chronic pain.
In summary, this study provides a valid assessment tool for measuring a relatively unexamined construct among parents of pediatric pain patients: the Parent Pain Acceptance Questionnaire. Moreover, the results demonstrate that the PPAQ, while derived from a measure of parents’ perceptions of their child’s pain acceptance, functions in a slightly different manner and is a construct worth examining in its own right. Parent pain acceptance is closely associated with child pain acceptance and with positive psychological and functional outcomes for youth with chronic pain.
Supplementary Material
Acknowledgments
This investigation was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (K23HD067202) to LS, the Boston Children’s Hospital Career Development Fellowship Award to CS, the Sara Page Mayo Endowment for Pediatric Pain Research and Treatment, and the Department of Anesthesiology, Perioperative and Pain Medicine at Boston Children’s Hospital. We also wish to thank all of the families who participated in this study.
References
- 1.Campo JV, et al. Physical and emotional health of mothers of youth with functional abdominal pain. Archives of pediatrics & adolescent medicine. 2007;161(2):131. doi: 10.1001/archpedi.161.2.131. [DOI] [PubMed] [Google Scholar]
- 2.Lewandowski AS, et al. Systematic review of family functioning in families of children and adolescents with chronic pain. The Journal of Pain. 2010;11(11):1027–1038. doi: 10.1016/j.jpain.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caes L, et al. Parental catastrophizing about child’s pain and its relationship with activity restriction: the mediating role of parental distress. Pain. 2011;152(1):212–222. doi: 10.1016/j.pain.2010.10.037. [DOI] [PubMed] [Google Scholar]
- 4.Sieberg CB, Williams S, Simons LE. Do parent protective responses mediate the relation between parent distress and child functional disability among children with chronic pain? Journal of pediatric psychology. 2011;36(9):1043–1051. doi: 10.1093/jpepsy/jsr043. [DOI] [PubMed] [Google Scholar]
- 5.Goubert L, et al. Parental catastrophizing about their child’s pain. The parent version of the Pain Catastrophizing Scale (PCS-P): a preliminary validation. Pain. 2006;123(3):254–263. doi: 10.1016/j.pain.2006.02.035. [DOI] [PubMed] [Google Scholar]
- 6.Van Slyke DA, Walker LS. Mothers' responses to children's pain. The Clinical journal of pain. 2006;22(4):387–391. doi: 10.1097/01.ajp.0000205257.80044.01. [DOI] [PubMed] [Google Scholar]
- 7.McCracken LM, Gauntlett-Gilbert J. Role of psychological flexibility in parents of adolescents with chronic pain: Development of a measure and preliminary correlation analyses. Pain. 2011;152(4):780–785. doi: 10.1016/j.pain.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Jordan A, Eccleston C, Crombez G. Parental functioning in the context of adolescent chronic pain: a review of previously used measures. Journal of pediatric psychology. 2008;33(6):640–659. doi: 10.1093/jpepsy/jsm139. [DOI] [PubMed] [Google Scholar]
- 9.Vowles KE, McCracken LM, Eccleston C. Patient functioning and catastrophizing in chronic pain: the mediating effects of acceptance. Health Psychology. 2008;27(2S):S136. doi: 10.1037/0278-6133.27.2(Suppl.).S136. [DOI] [PubMed] [Google Scholar]
- 10.McCracken LM, Vowles KE. A prospective analysis of acceptance of pain and values-based action in patients with chronic pain. Health Psychology. 2008;27(2):215. doi: 10.1037/0278-6133.27.2.215. [DOI] [PubMed] [Google Scholar]
- 11.Wallace DP, et al. Adolescent acceptance of pain: confirmatory factor analysis and further validation of the chronic pain acceptance questionnaire, adolescent version. The Journal of Pain. 2011;12(5):591–599. doi: 10.1016/j.jpain.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 12.Wicksell RK, Melin L, Olsson GL. Exposure and acceptance in the rehabilitation of adolescents with idiopathic chronic pain–a pilot study. European Journal of Pain. 2007;11(3):267–274. doi: 10.1016/j.ejpain.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 13.Wicksell RK, et al. Evaluating the effectiveness of exposure and acceptance strategies to improve functioning and quality of life in longstanding pediatric pain–a randomized controlled trial. Pain. 2009;141(3):248–257. doi: 10.1016/j.pain.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 14.McCracken LM, Vowles KE, Eccleston C. Acceptance-based treatment for persons with complex, long standing chronic pain: a preliminary analysis of treatment outcome in comparison to a waiting phase. Behaviour research and therapy. 2005;43(10):1335–1346. doi: 10.1016/j.brat.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 15.Vowles KE, McCracken LM. Acceptance and values-based action in chronic pain: a study of treatment effectiveness and process. Journal of consulting and clinical psychology. 2008;76(3):397. doi: 10.1037/0022-006X.76.3.397. [DOI] [PubMed] [Google Scholar]
- 16.Simons LE, Sieberg CB, Kaczynski KJ. Measuring parent beliefs about child acceptance of pain: a preliminary validation of the Chronic Pain Acceptance Questionnaire, parent report. Pain. 2011;152(10):2294–2300. doi: 10.1016/j.pain.2011.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCracken LM, Gauntlett-Gilbert J, Eccleston C. Acceptance of pain in adolescents with chronic pain: Validation of an adapted assessment instrument and preliminary correlation analyses. European Journal of Pain. 2010;14(3):316–320. doi: 10.1016/j.ejpain.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 18.Weiss KE, et al. Acceptance of Pain: Associations With Depression, Catastrophizing, and Functional Disability Among Children and Adolescents in an Interdisciplinary Chronic Pain Rehabilitation Program. Journal of pediatric psychology. 2013 doi: 10.1093/jpepsy/jst028. [DOI] [PubMed] [Google Scholar]
- 19.Hollingshead AB. Four factor index of social status. 1975. [Google Scholar]
- 20.McCracken LM, Vowles KE, Eccleston C. Acceptance of chronic pain: component analysis and a revised assessment method. Pain. 2004;107(1):159–166. doi: 10.1016/j.pain.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 21.Simons LE, et al. The Fear of Pain Questionnaire (FOPQ): assessment of pain-related fear among children and adolescents with chronic pain. The Journal of Pain. 2011;12(6):677–686. doi: 10.1016/j.jpain.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 22.Simons LE, Claar RL, Logan DL. Chronic pain in adolescence: Parental responses, adolescent coping, and their impact on adolescent's pain behaviors. Journal of Pediatric Psychology. 2008;33(8):894–904. doi: 10.1093/jpepsy/jsn029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Crombez G, et al. The child version of the pain catastrophizing scale (PCS-C): a preliminary validation. Pain. 2003;104(3):639–646. doi: 10.1016/S0304-3959(03)00121-0. [DOI] [PubMed] [Google Scholar]
- 24.Walker LS, Greene JW. The functional disability inventory: measuring a neglected dimension of child health status. Journal of Pediatric Psychology. 1991;16(1):39–58. doi: 10.1093/jpepsy/16.1.39. [DOI] [PubMed] [Google Scholar]
- 25.Claar RL, Walker LS. Functional assessment of pediatric pain patients: psychometric properties of the functional disability inventory. Pain. 2006;121(1):77–84. doi: 10.1016/j.pain.2005.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.von Baeyer CL, et al. Three new datasets supporting use of the Numerical Rating Scale (NRS-11) for children’s self-reports of pain intensity. Pain. 2009;143(3):223–227. doi: 10.1016/j.pain.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 27.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior research methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 28.Zhao X, Lynch JG, Chen Q. Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research. 2010;37(2):197–206. [Google Scholar]
- 29.DeVellis RF. Scale development: Theory and applications. Vol. 26. Sage; 2011. [Google Scholar]
- 30.Cattell RB. The scree test for the number of factors. Multivariate behavioral research. 1966;1(2):245–276. doi: 10.1207/s15327906mbr0102_10. [DOI] [PubMed] [Google Scholar]
- 31.Connelly M, et al. Parent pain responses as predictors of daily activities and mood in children with juvenile idiopathic arthritis: the utility of electronic diaries. Journal of pain and symptom management. 2010;39(3):579–590. doi: 10.1016/j.jpainsymman.2009.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Palermo TM, Chambers CT. Parent and family factors in pediatric chronic pain and disability: an integrative approach. Pain. 2005;119(1):1–4. doi: 10.1016/j.pain.2005.10.027. [DOI] [PubMed] [Google Scholar]
- 33.Palermo TM, Eccleston C. Parents of children and adolescents with chronic pain. Pain. 2009;146(1–2):15. doi: 10.1016/j.pain.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goodman JE, McGrath PJ. Mothers’ modeling influences children's pain during a cold pressor task. Pain. 2003;104(3):559–565. doi: 10.1016/S0304-3959(03)00090-3. [DOI] [PubMed] [Google Scholar]
- 35.Hechlerl T, et al. Parental catastrophizing about their child's chronic pain: are mothers and fathers different? European Journal of Pain. 2011;15(5):515. e1–515. e9. doi: 10.1016/j.ejpain.2010.09.015. [DOI] [PubMed] [Google Scholar]
- 36.Hobara M. Beliefs about appropriate pain behavior: cross-cultural and sex differences between Japanese and Euro-Americans. European journal of pain. 2005;9(4):389–393. doi: 10.1016/j.ejpain.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 37.Nayak S, et al. Culture and gender effects in pain beliefs and the prediction of pain tolerance. Cross-Cultural Research. 2000;34(2):135–151. [Google Scholar]
- 38.Sanders SH, et al. Chronic low back pain patients around the world: cross-cultural similarities and differences. The Clinical journal of pain. 1992;8(4):317–323. doi: 10.1097/00002508-199212000-00006. [DOI] [PubMed] [Google Scholar]
- 39.Jordan A, et al. The Bath Adolescent Pain–Parental Impact Questionnaire (BAP-PIQ): Development and preliminary psychometric evaluation of an instrument to assess the impact of parenting an adolescent with chronic pain. Pain. 2008;137(3):478–487. doi: 10.1016/j.pain.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 40.Wetherell JL, et al. A randomized, controlled trial of acceptance and commitment therapy and cognitive-behavioral therapy for chronic pain. Pain. 2011;152(9):2098–2107. doi: 10.1016/j.pain.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 41.Gauntlett-Gilbert J, et al. Acceptance and values-based treatment of adolescents with chronic pain: Outcomes and their relationship to acceptance. Journal of pediatric psychology. 2013;38(1):72–81. doi: 10.1093/jpepsy/jss098. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


