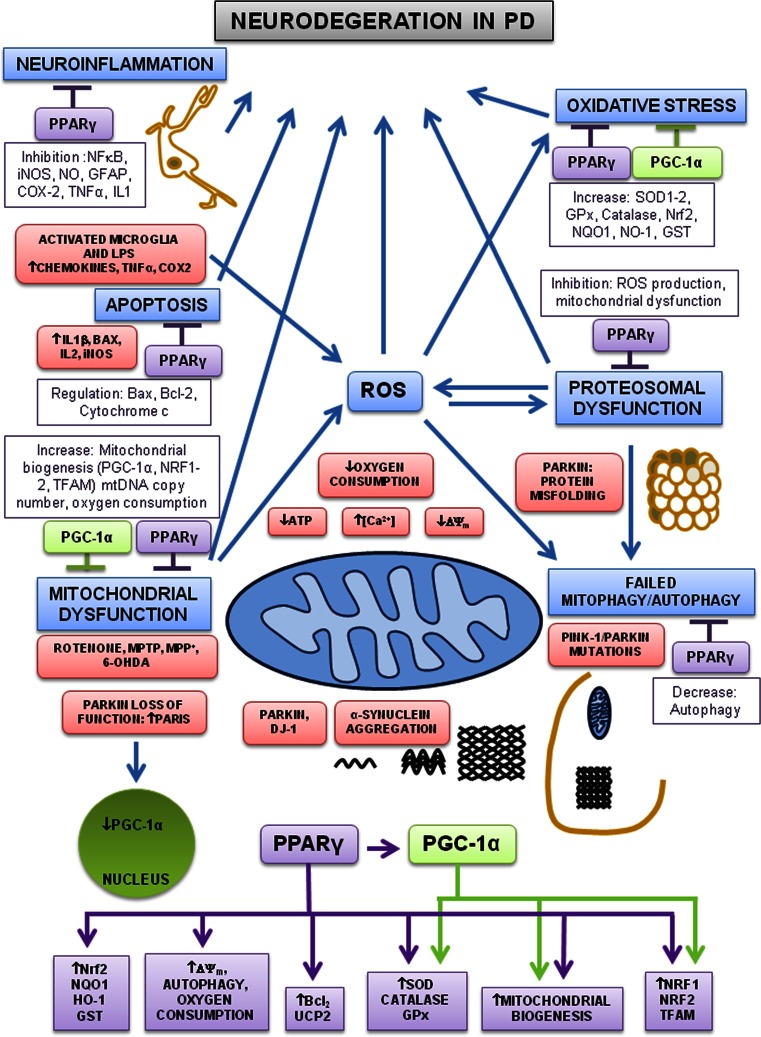
Fig. 1.
Pathways involved in neuroprotection by PPARγ and PGC-1α in PD. Mitochondrial dysfunction, oxidative stress, proteosomal dysfunction, neuroinflammation, autophagy and apoptosis are all implicated in the pathogenesis of PD. Environmental factors and toxins (rotenone, MPTP, MPP+ and 6-OHDA) directly induce both oxidative stress and mitochondrial dysfunction. Different toxins increase oxidative stress (ROS) and cause mitochondrial dysfunction, both increase [Ca2+], decrease ATP, decrease mitochondrial membrane potential, decrease oxygen consumption and cause failure in autophagy, proteosomal dysfunction and abnormal protein aggregation which ultimately lead to neuronal death. Activated microglia release inflammatory cytokines and increase ROS, driving neuronal degeneration. DJ-1 and PARKIN mutations cause aggregation of α-synuclein and PARKIN/PINK-1 mutations cause failure in autophagy. Mutations in the PARKIN gene cause protein misfolding. Mutations in PARKIN also increase expression of the PARIS, thereby repressing the expression of PGC-1α. PPARγ agonists inhibit microglial activation and reduce inflammation by decreasing expression of cytokines, TNF-α, COX2 and iNOS. PPARγ agonists reduced apoptosis by inhibition of BAX, IL2, IL1β and by increasing Bcl-2 expression. PPARγ agonists increase antioxidant defences, mitochondrial biogenesis, oxygen consumption, mitochondrial membrane potential, autophagy, PGC-1α and other transcription factors. Moreover, PGC-1α induces the expression of downstream target genes involved in mitochondrial biogenesis, transcription factors and antioxidant defences. Thus, PGC-1α and PPARγ agonists regulate the expression of several target genes involved in neuronal survival and neuroprotection by inhibiting mitochondrial dysfunction, oxidative stress, proteosomal dysfunction, autophagy, neuroinflammation and apoptosis