Abstract
There is a high rate of mortality in elderly patients who sustain a fracture of the hip. We aimed to determine the rate of preventable mortality and errors during the management of these patients. A 12 month prospective study was performed on patients aged > 65 years who had sustained a fracture of the hip. This was conducted at a Level 1 Trauma Centre with no orthogeriatric service. A multidisciplinary review of the medical records by four specialists was performed to analyse errors of management and elements of preventable mortality. During 2011, there were 437 patients aged > 65 years admitted with a fracture of the hip (85 years (66 to 99)) and 20 died while in hospital (86.3 years (67 to 96)). A total of 152 errors were identified in the 80 individual reviews of the 20 deaths. A total of 99 errors (65%) were thought to have at least a moderate effect on death; 45 reviews considering death (57%) were thought to have potentially been preventable. Agreement between the panel of reviewers on the preventability of death was fair. A larger-scale assessment of preventable mortality in elderly patients who sustain a fracture of the hip is required. Multidisciplinary review panels could be considered as part of the quality assurance process in the management of these patients.
Cite this article: Bone Joint J 2014;96-B:1178–84.
Keywords: Hip fracture; Preventable mortality; Errors
Despite the decreasing incidence of fractures of the hip in Australia,1 the total number of fractures is rising in line with global trends.2,3 The increasing burden has major socio-economic consequences.4This age group is highly vulnerable to morbidity and mortality. Pre-existing illness and functional deficit, surgical stress, and post-operative immobilisation result in rates of mortality one-year after operation of up to 30%.5 It is not known whether the mortality reflects the poor pre-existing health of the patients or errors in medical care. However, there has been a steady increase in the age of patients who sustain this injury over the last four decades with little change in mortality.4,6
Mortality has been widely used as an endpoint in assessing this group of patients, and is taken as a surrogate marker for the quality of care delivered to geriatric patients with a fracture of the hip. In-hospital mortality rates of up to 20% have been cited in systems that have orthopaedic care as their main model.7 Potentially preventable errors occur in the management of elderly patients. Impressive reduction in the rates of mortality has been achieved when more holistic models of care have been followed.8
In the management of elderly patients with a fracture of the hip, crude mortality may not be an appropriate measure of the quality of care. A proportion of these patients will die irrespective of the quality of medical treatment. Studies on preventable mortality have been used for the past 50 years to assess the delivery of trauma care,9 with institutions identifying deaths which may not have occurred if alternative management had been undertaken.10 Such studies have been used in Australia11,12 particularly in the modern trauma community.13-19The prevalence of potentially preventable errors and mortality in patients who have sustained a fracture of the hip is not known.
We hypothesised that substantial preventable mortality and errors exist in the management of elderly patients who sustain a fracture of the hip, and performed a prospective study using a panel of experts to identify these.
Patients and Methods
The study took place at the John Hunter Hospital, New South Wales (NSW), a university affiliated, Royal Australian College of Surgeons verified, Level 1 trauma centre which admits > 400 patients with a fracture of the hip per year.20 All patients aged > 65 years with a proximal femoral fracture of AO Müller classification 31 A or B21 were prospectively followed on admission over a one-year period (2011). This involved 437 patients. Patients who met inclusion criteria were identified and those who died as inpatients were subjected to review by a panel of multidisciplinary experts. The study had ethical approval.
The panel consisted of a geriatrician (TLB), orthopaedic surgeon (ZJB), an anaesthetist (PLB) and general physician (JA). All were chosen due to their experience and interest in managing orthogeriatric patients and all had a knowledge and understanding of the resources and expectations of the orthopaedic trauma and medical services of the institution.
Each member of the panel was blinded to the others’ opinions during the review process. They were provided with a death review synopsis, a succinct summary of the events during hospitalisation, as well as a hard copy of all the medical records during admission, including the pathology results and death certificates. They were briefed on how to complete a preventable mortality questionnaire before review of the deaths. The questionnaire was based on previous studies of preventable mortality.12,22,23
The questionnaire allowed a maximum of five crucial errors deemed significant to the reviewer to be listed. The location and time of the error (emergency department, pre-operative ward, operating theatre (OT), within 24 hours post-operatively, between 24 and 72 hours post-operatively, and beyond 72 hours post-operatively) and the nature of the error (delay in treatment, delay to OT, delay in diagnosis, errors in diagnosis, technique, and medical judgement, inadequate documentation, communication failure) was recorded. Whether the error had an impact on the outcome (death) was noted (no impact, minimal impact, moderate impact, major impact), as was its preventability (unpreventable, potentially preventable, probably preventable or definitely preventable). Errors were presented as means for all the reviewers combined.
Ultimately, deaths could therefore be classified as ‘unpreventable’, ‘possibly preventable’, ‘probably preventable’ or ‘definitely preventable’. Preventable death was defined as one that satisfies three tenets: 1) the general condition on admission was survivable, 2) the delivery of care was sub-optimal and 3) the error in care was directly or indirectly implicated in the death of the patient.9
Demographic, peri-operative and predictive data were collected for patients and compared with available data for all patients who were admitted with a fracture of the hip in 2011. Admissions for 2011 were calculated by cross-referencing with our institutional long bone fracture database and theatre records. Mortality was generated by submission of patient demographics to the NSW Government Registry of Births, Deaths and Marriages.
A control group was prepared from the 417 patients with a fracture of the hip who did not die as an inpatient. Each was matched for age, gender and American Society of Anesthesiologists (ASA) grade24 with one of those who died as an inpatient. Reviewers also recorded the medical errors from these patients’ records.
Statistical analysis
Continuous data are presented as a mean value for all assessors, with range, for parametric variables and as medians and interquartile ranges (IQR) for non-parametric variables. Categorical data are presented as proportions. Comparisons between means were performed using one-way analysis of variance (ANOVA) and between medians using the Mann–Whitney U test. Categorical data were analysed using the chi-squared test. The level of agreement between pairs of reviewers was calculated using Cohen’s Kappa coefficient. The intraclass correlation coefficient (ICC) was used to assess the agreement achieved between reviewers. Statistical significance was set at p = < 0.05. Analysis was performed using IBM SPSS Statistics 20 (IBM SPSS Inc., Armonk, New York).
Results
Of the 437 patients identified for inclusion in the study (mean age 85 years (66 to 99); M:F 138:299), 20 died as inpatients (4.6%) and the overall 30-day mortality for the cohort was 37 patients (8.4%).
The mean age of the 20 inpatients who died was 86.3 years (67 to 96; M:F 10:10). A total of 14 of this group presented to the emergency department during normal working hours (defined as 7am to 7pm, Monday to Friday); 14 had general medical and/or medical subspecialty review during the admission. The control group was matched with a mean age of 86.4 years (67 to 97; M:F 9:11) and ASA matched for the 14 who died as an inpatient and had been assessed by an anaesthetist.
A total of 13 of those who died as an inpatient underwent operative intervention. This was performed at a mean of 25.9 hours (2 to 52) after admission, and 11 of these had their operation within normal working hours. Only two of the operative candidates had their surgery postponed due to insufficient operative availability. The mean length of the anaesthetic was 120 minutes (92 to 160). The ASA grade was 2 for one patient, 3 for eight patients and 4 for four patients. There were no intra-operative deaths. A total of three patients died within 24 hours of surgery. The median time between the operation and death was 4.6 days (0.33 to 26.4).
Only six of the 20 deaths occurred in normal working hours: six of the 20 deaths were due to myocardial infarction, four to sepsis, four to pneumonia, two to gastrointestinal haemorrhage, one to stroke, one to pulmonary embolus, one to intestinal ischaemia and one to acute renal failure. Only two patients were referred to the coroner in addition to the three who died within 24 hours of the operation, for whom referral was compulsory. The treating resident doctors decided the cause of death in 13 patients.
There was a lack of agreement between the four reviewers about the number errors in the delivery of care in both the patients who died and amongst the controls. However in both groups, the geriatrician identified the greatest number of errors per patient (Table I). A total of 152 errors were identified in the 20 deaths and 54 errors were identified in the control group.
Table I.
Reviewer errors and death preventability (shown as mean values with ranges)
| Mortality preventability (n = 80) | ||||||
|---|---|---|---|---|---|---|
| Errors per control | Errors per death | Unpreventable | Potentially preventable | Probably preventable | Definitely preventable | |
| Physician | 0.55 (0 to 1) | 0.85 (0 to 3) | 11 | 6 | 3 | 0 |
| Geriatrician | 1.10 (0 to 3) | 2.75 (0 to 5) | 2 | 11 | 7 | 0 |
| Anaesthetist | 0.70 (0 to 4) | 2.15 (0 to 4) | 9 | 8 | 3 | 0 |
| Orthopaedic Surgeon | 0.55 (0 to 2) | 1.85 (0 to 4) | 13 | 7 | 0 | 0 |
The errors noted by the reviewers for those who died as an inpatient were accumulated and collated in subgroups. In order of prevalence, these were: insufficient medical team involvement (n = 22, 14.1%), poor management of medical conditions (n = 19, 12.3%), poor fluid or haemodynamic management (n = 15, 9.9%), poor management of arrhythmia (n = 13, 8.6%), poor management of medication (n = 13, 8.6%), poor pre-operative medical assessment (n = 11, 7.4%), delay of operative intervention (n = 8, 4.9%), poor electrolyte management (n = 8, 4.9%), inadequate orthopaedic skill (in geriatric patient management; n = 6, 3.7%) and poor communication between specialties (n = 6, 3.7%). Other less represented errors accounted for the remainder (n = 33, 21.7%).
The errors in the control group were divided into poor discharge planning (n = 14, 25.9%), insufficient medical involvement (n = 9, 16.7%), poor cognitive documentation (mostly failing to assess cognitive ability with an assessment of the mental state; n = 9, 16.7%), poor fluid or haemodynamic management (n = 5, 9.3%), inadequate orthopaedic skills (n = 3, 5.6%) and other types of error identified less frequently (n = 14, 25.9%)
The 152 errors which contributed to the deaths were allocated between 211 types: error in judgement (n = 55, 26.0%), error in diagnosis (n = 44, 20.8%), delay in treatment (n = 35, 16.6%), delay in diagnosis (n = 25,11.8%), error in technique (n = 22, 10.4%), communication (n = 15, 8.1%), delay to theatre (n = 10, 4.7%) and inadequate documentation (n = 5, 2.4%). The 54 errors in the control group were grouped into 60 types: error in judgement (n = 32, 53.3%), communication (n = 13, 21.7%), error in technique (n = 5, 8.3%), inadequate documentation (n = 4, 6.7%), delay in treatment (n = 3, 5.0%), error in diagnosis (n = 2, 3.3%) and delay to theatre (n = 1, 1.7%).
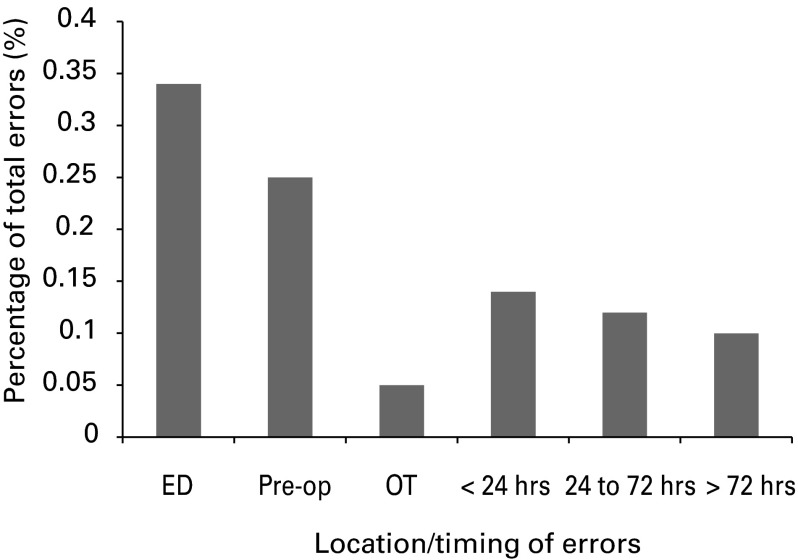
The 152 errors amongst the patients who died were distributed over 259 timings and locations. More than half (n = 155, 59.9%) of errors occurred pre-operatively, with 88 (34.0%) in the emergency department and 67 (25.9%) on the ward. Only 13 (5.0%) of errors occurred during the operation, with 36 (13.9%) happening within the first 24 hours post-operatively, 30 (11.6%) between 24 and 72 hours post-operatively, and 25 (9.7%) occurring after 72 hours (Fig. 1). Of the errors, 3 (2.0%) were deemed unpreventable, 48 (31.6%) possibly preventable, 41 (27.0%) probably preventable and 60 (39.5%) definitely preventable.
Fig. 1.
Histogram showing location and timing of errors (ED, emergency department; OT, operating theatre, Pre-op, pre-operative).
In the control group, the 54 errors were spread over 120 timings and locations. More than two-thirds of errors occurred post-operatively; 19 (15.8%) within the 24 hours, 26 (21.7%) between 24 and 72 hours post-operatively, and 36 (30.0%) after 72 hours. In contrast, 20 (16.7%) occurred in the emergency department, 17 (14.2%) pre-operatively on the ward and 2 (1.7%) intra-operatively. No errors were deemed unpreventable, 5 (9.3%) possibly preventable, 17 (31.5%) probably preventable and 32 (59.3%) definitely preventable.
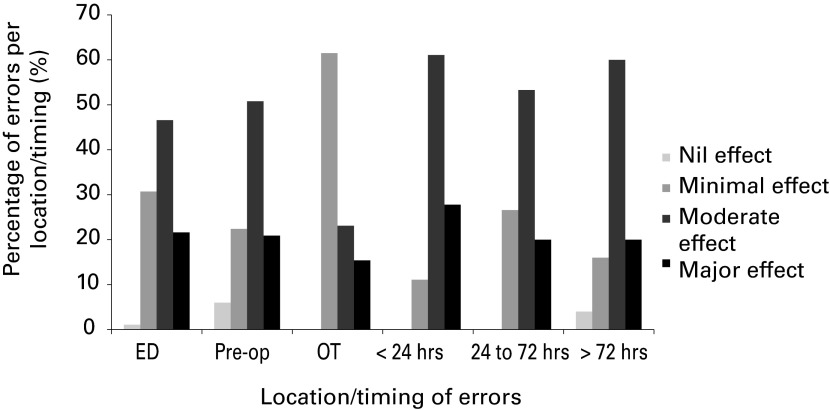
When the impact of the errors is considered with regard to timing and location for inpatient deaths, it was only in the operating theatre that most errors were thought to have minimal effect on the outcome (Fig. 2).
Fig. 2.
Histogram showing the effect on error outcome per location/timing (ED, emergency department; OT, operating theatre; Pre-op, pre-operative).
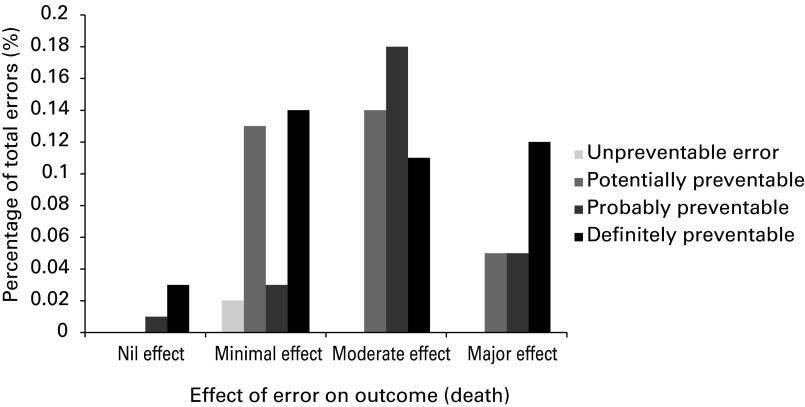
The effect of errors on mortality was recorded as: 6 (3.9%) having no effect, 48 (31.6%) having minimal effect, 65 (42.8%) having a moderate effect and 33 (21.7%) having a major effect on death. The relationship between the effect of errors on mortality, and the preventability of those errors, showed that 44 (66.4%) of the errors that had a moderate effect on death (n = 65, 42.8% of errors), and 25 (75.8%) of the errors that had a major effect (n = 33, 21.7% of errors), were probably or definitely preventable (Fig. 3).
Fig. 3.
Histrogram showing the effect of errors on outcome and preventability.
Of the 80 reviews of inpatient mortality, 35(43.8%) of the deaths were classified as unpreventable, 32 (40%) as possibly preventable and 13 (16.3%) as probably preventable. No reviewer considered any of the deaths as definitely preventable (Table I).
Unpreventable deaths featured a mean of 5.7 (1 to 13) errors per review. Possibly and probably preventable deaths had 9.1 (3 to 13) and 8.5 (2 to 13) mean errors per review, respectively. This difference in errors between groups was statistically significant (p < 0.001 Kruskal– Wallis). There was no significant difference in age (p = 0.41, Kruskal–Wallis,), time to surgery (p = 0.41, Kruskal–Wallis) or ASA grade (χ² test, p = 0.78) between these patients (Table II).
Table II.
Differences between preventability of death reviews (means with ranges as appropriate)
| Review outcome | Errors | Age (yrs) | Time to operation (hrs) | ASA* Grade (Grade, reviews with ASA, %) |
|---|---|---|---|---|
| Unpreventable (n = 35) | 5.7 (1 to 13)† | 84.3 (67 to 96) | 23.8 (2 to 52) | 2:2 (9.5%)/3:12 (57.1%) /4:7 (33.3%) |
| Possibly preventable (n = 32) | 9.1 (3 to 13)† | 88.0 (67 to 96) | 24.0 (2 to 52) | 2:2 (8.0%)/3:18 (72.0%)/4:5 (20.0%) |
| Probably preventable(n = 13) | 8.5 (2 to 12)† | 86.5 (73 to 95) | 24.2 (20 to 52) | 2:0 (0%)/ 3:6 (60%)/4:4 (40%) |
*ASA, American Society of Anesthesiologists † Kruskal–Wallis, p < 0.001
Fair agreement regarding preventability of each death was demonstrated by an intra-class correlation coefficient of 0.46 (95% confidence interval (CI): 0.001 to 0.778). The Kappa index of concordance recorded moderate agreement between the anaesthetist and orthopaedic surgeon (κ = 0.54). Within the other relationships, agreement was slight (κ = 0.07 to 0.17) and even worse than chance between the anaesthetist and general physician (κ = -0.13) (Table III).
Table III.
Level of agreement between reviewers
| Kappa-concordance | |||
|---|---|---|---|
| Geriatrician | Physician | Anaesthetist | |
| Physician | 0.171 | - | - |
| Anaesthetist | 0.07 | -0.126 | - |
| Orthopaedic surgeon | 0.053 | 0.147 | 0.538 |
Discussion
In this study, preventable errors were found in the care of geriatric patients with hip fractures, some of which were considered to have contributed to the patients’ death. Therefore, an element of preventable mortality exists in our institution, as do inadequacies in management.
Very few errors occurred during the operation. Most were deemed to have had minimal effect on death and occurred pre-operatively involving inadequate medical involvement in patient care and inadequate management of medical conditions.
A wide range of errors was made, of which most were thought to have been probably preventable and had at least a moderate effect on the eventual outcome. Deaths with a higher degree of preventability featured more errors, despite there being no difference in age, ASA score, or time to surgery, all of which are considered to be independent predictors of mortality.25,26
More than half of all inpatient deaths were thought to be at least possibly preventable. The inter-observer agreement between the reviewers was fair. Despite the fact that most patients presented and had their surgery during normal working hours, more than two-thirds of deaths happened outside this time, and from a wide variety of conditions.
A control group was included for which all reviewers cited fewer errors. Lack of involvement from a medical team, poor discharge planning and poor cognitive assessment, which affects the selection of destination of discharge and hence length of stay, were the major errors which were identified. Errors in fluid and haemodynamic management constituted the main error in ‘medical management’. Errors in judgement and communication constituted of 75% of the types of error, and most of these occurred post-operatively. The outcomes between the control group and those who died were not blinded, which could affect the identification of errors despite efforts to remain objective. As most errors that can be prevented and influence mortality occur in the peri-operative period, future designs of study could be improved by focusing on this period of time and blinding outcomes.
Surgeons were the first to publish rates of mortality and have tended to assume responsibility for their outcomes.27 Reduction in the rate of mortality has been commonly used as a surrogate marker for improvement in care in trauma surgery.28 A reduction of preventable mortality has been well documented after the introduction of trauma systems. In seminal studies from Orange County, California, potentially salvageable deaths related to trauma were substantially reduced from 71% to 21%29 and from 34% to 15%.30 This experience has been repeated elsewhere.12-14,16-18
It is currently recommended that fixation of fractures of the hip should be undertaken within 36 hours of presentation,31 with delays of more than 48 hours leading to increased mortality.32,33 In our cohort, timely operative management was achieved but may have limited the time available for medical preparation or pre-operative planning. Shorter times between admission and surgery have been shown to be a predictor of increased inpatient mortality, possibly for this reason.34
Teixeira et al15 examined 2000 deaths over eight years in a mature trauma system, showing ‘delay in treatment’, ‘clinical judgement’ and ‘missed diagnosis’ to be the major types of error. The management of fractures in the elderly does not include the same urgency, but we similarly see that ‘delay in treatment’, ‘error in diagnosis’, and ‘error in judgement’ constitute the most common types of error in this study.
The variety of causes of death was similar to other reports.35Inpatient mortality was 4.6% in our institution, which is higher than in many international centres.8No deaths were deemed definitely avoidable, which is understandable given the complex physiological state of patients who sustain a fracture of the hip, but most had elements of preventability.
The greatest agreement regarding the possible prevention of death was between the orthopaedic surgeon and anaesthetist. The second greatest was between the physician and geriatrician, however this was slight. Other agreement was slight, with no agreement between the anaesthetist and physician.
Detailed examination of the negative relationship revealed agreement in seven patients. However, the physician believed that death had a higher degree of preventability in six patients and cited lack of involvement of the medical team and failure to diagnose infection early. In the remaining seven patients, in which the anaesthetist cited a higher degree of preventability, poor management of peri-operative rapid atrial fibrillation, bradycardia, and hypotension were cited. These were not mentioned by the physician. This difference in perspective suggests that better peri-operative haemodynamic management, led by anaesthetists, and better post-operative medical leadership, led by physicians, would reduce mortality.
As shown in large trauma studies, it is not the lack of availability of sophisticated personnel or institutional resources that leads to preventable deaths, but inadequate management.36
Blinding reviewers results in low Kappa concordance compared with panel discussions. The increase in concordance from discussion does not necessarily relate to an increased validity of the technique, as the Kappa score was designed for independent reviewers.10 Kappa scores in some multiple panel trauma reviews of mortality have achieved a concordance of p > 0.8,37 which is far greater than our scores with blinded reviewers.
Panels have been made up in different ways in the past, with different ways of establishing whether a death was preventable or not. These have included: panel consensus reviews (which tend to overestimate preventable death), independent reviews, modified independent review and a unanimous review (which tend to underestimate preventability).9 In our study, we allowed each reviewer’s opinion to constitute a single entity, for analysis. Each subspecialty has a particular insight into certain facets of orthogeriatric management, and can detect errors, and whether these could have been avoided and death possibly prevented. The panel consisted of specialists who were well versed, and involved in the provision of orthogeriatric care. As the public awareness of what constitutes good clinical care has increased, the ability for the medical profession to assess quality must likewise increase. If preventable mortality can be identified, improved models of care should be formulated and validated. Better use of existing resources has been shown to decrease length of stay, the time between admission and surgery, and mortality.38
The need for institutional protocol and guidelines has been suggested recently by the NSW Health Clinical Excellence Commission39 based largely on the British Orthopaedic Association’s 2007 Blue Book and recent National Institute of Health and Clinical Excellence guidelines.31,40 Prospective data collection is the optimal way of assessing the effects of changes in management, as seen in the United Kingdom.41 Large retrospective population-based studies of geriatric patients who sustain fractures of the hip have been performed in the state of NSW.42 The reduction of mortality amongst high energy patients has been elucidated through analysis of the NSW trauma registry.43 Similar prospectively collected State or National level registries of hip fractures would allow similar analyses.
The fact that more than 50% of deaths were at least possibly preventable, suggests that mortality can be reduced with improved care pathways.44 In the event that preventable mortality is overestimated, it certainly does not diminish the importance of trying to reduce the medical errors that may result in death. Even if a patient’s life expectancy is short, preventable errors that lead to death in hospital should still not be acceptable for the medical profession.
The financial burden of the management of hip fractures in the elderly is projected to increase dramatically as their prevalence increases.45An Australian National Hip Fracture Registry, currently being trialled and based on the United Kingdom National Hip Fracture Database,41 could benefit from including information about deaths as an inpatient to identify preventable errors and preventable mortality. This may be an effective way of comparing institutions that have different models of treatment of hip fractures to identify the ideal management.
A proportion of elderly patients who die while in hospital after treatment for a fracture of the hip do so for preventable reasons. The need for timely senior input in peri-operative medical optimisation is evident. The prevalence of preventable mortality and errors in care can be used as an indicator of quality in the management of these patients.
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Chang KP, Center JR, Nguyen TV, Eisman JA. Incidence of hip and other osteoporotic fractures in elderly men and women: Dubbo Osteoporosis Epidemiology Study. J Bone Miner Res 2004;19:532–536. [DOI] [PubMed] [Google Scholar]
- 2.No authors listed. AIHW. The problem of osteoporotic hip fracture in Australia, 2010. http://www.aihw.gov.au/publication-detail/?id=6442468333 (date last accessed 14 May 2014).
- 3.Cheng SY, Levy AR, Lefaivre KA, et al. Geographic trends in incidence of hip fractures: a comprehensive literature review. Osteoporos Int 2011;22:2575–2586. [DOI] [PubMed] [Google Scholar]
- 4.Bergström U, Jonsson H, Gustafson Y, et al. The hip fracture incidence curve is shifting to the right. Acta Orthop 2009;80:520–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mundi S, Pindiprolu B, Simunovic N, Bhandari M. Similar mortality rates in hip fracture patients over the past 31 years. Acta Orthop 2014;85:54–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haleem S, Lutchman L, Mayahi R, Grice JE, Parker MJ. Mortality following hip fracture: trends and geographical variations over the last 40 years. Injury 2008;39:1157–1163. [DOI] [PubMed] [Google Scholar]
- 7.Stone ME Jr, Barbaro C, Bhamidipati CM, Cucuzzo J, Simon R. Elderly hip fracture patients admitted to the trauma service: does it impact patient outcome? J Trauma 2007;63:1348–1352. [DOI] [PubMed] [Google Scholar]
- 8.Kammerlander C, Roth T, Friedman SM, et al. Ortho-geriatric service: a literature review comparing different models. Osteoporosis Int 2010;21(Suppl):S637–S646. [DOI] [PubMed] [Google Scholar]
- 9.MacKenzie EJ. Review of evidence regarding trauma system effectiveness resulting from panel studies. J Trauma 1999;47(Suppl):S34–S41. [DOI] [PubMed] [Google Scholar]
- 10.Wilson DS, McElligott J, Fielding LP. Identification of preventable trauma deaths: confounded inquiries? J Trauma 1992;32:45–51. [DOI] [PubMed] [Google Scholar]
- 11.McDermott FT, Cordner SM, Tremayne AB. Evaluation of the medical management and preventability of death in 137 road traffic fatalities in Victoria, Australia: an overview. Consultative Committee on Road Traffic Fatalities in Victoria. J Trauma 1996;40:520-33; discussion 33-5.:. [DOI] [PubMed] [Google Scholar]
- 12.Sugrue M, Caldwell E, D'Amours S, et al. Time for a change in injury and trauma care delivery: a trauma death review analysis. ANZ J Surg 2008;78:949–954. [DOI] [PubMed] [Google Scholar]
- 13.Ivatury RR, Guilford K, Malhotra AK, et al. Patient safety in trauma: maximal impact management errors at a level I trauma center. J Trauma 2008;64:265–270; discussion 270–272. [DOI] [PubMed] [Google Scholar]
- 14.Teixeira PG, Inaba K, Hadjizacharia P, et al. Preventable or potentially preventable mortality at a mature trauma center. J Trauma 2007;63:1338–1346; discussion 1346–1347. [DOI] [PubMed] [Google Scholar]
- 15.Teixeira PG, Inaba K, Salim A, et al. Preventable morbidity at a mature trauma center. Arch Surg 2009;144:536–541; discussion 541–542. [DOI] [PubMed] [Google Scholar]
- 16.Saltzherr TP, Wendt KW, Nieboer P, et al. Preventability of trauma deaths in a Dutch Level-1 trauma centre. Injury 2011;42:870–873. [DOI] [PubMed] [Google Scholar]
- 17.Gruen RL, Jurkovich GJ, McIntyre LK, Foy HM, Maier RV. Patterns of errors contributing to trauma mortality: lessons learned from 2,594 deaths. Ann Surg 2006;244:371–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stewart RM, Myers JG, Dent DL, et al. Seven hundred fifty-three consecutive deaths in a level I trauma center: the argument for injury prevention. J Trauma 2003;54:66–70; discussion 70–71. [DOI] [PubMed] [Google Scholar]
- 19.Zafarghandi MR, Modaghegh MH, Roudsari BS. Preventable trauma death in Tehran: an estimate of trauma care quality in teaching hospitals. J Trauma 2003;55:459–465. [DOI] [PubMed] [Google Scholar]
- 20.Williams N, Hardy BM, Tarrant S, et al. Changes in hip fracture incidence, mortality and length of stay over the last decade in an Australian major trauma centre. Arch Osteoporosis 2013;8:150. [DOI] [PubMed] [Google Scholar]
- 21.No authors listed. Müller AO classification of fractures: long Bones. https://www.aofoundation.org/Documents/mueller_ao_class.pdf (date last accessed 11 June 2014).
- 22.Shackford SR, Hollingsworth-Fridlund P, McArdle M, Eastman AB. Assuring quality in a trauma system: the Medical Audit Committee: composition, cost, and results. J Trauma 1987;27:866–875. [PubMed] [Google Scholar]
- 23.Hoyt DB, Hollingsworth-Fridlund P, Fortlage D, Davis JW, Mackersie RC. An evaluation of provider-related and disease-related morbidity in a level I university trauma service: directions for quality improvement. J Trauma 1992;33:586–601. [DOI] [PubMed] [Google Scholar]
- 24.Owens WD, Felts JA, Spitznagel EL Jr. ASA physical status classifications: a study of con- sistency of ratings. Anesthesiology 1978;49:239–243. [DOI] [PubMed] [Google Scholar]
- 25.Söderqvist A, Ekström W, Ponzer S, et al. Prediction of mortality in elderly patients with hip fractures: a two-year prospective study of 1,944 patients. Gerontology 2009;55:496–504. [DOI] [PubMed] [Google Scholar]
- 26.Aharonoff GB, Koval KJ, Skovron ML, Zuckerman JD. Hip fractures in the elderly: predictors of one year mortality. J Orthop Trauma 1997;11:162–165. [DOI] [PubMed] [Google Scholar]
- 27.Trunkey DD. Invited commentary: panel reviews of trauma mortality. J Trauma 1999;47:S44–S45. [DOI] [PubMed] [Google Scholar]
- 28.Dutton RP, Stansbury LG, Leone S, et al. Trauma mortality in mature trauma systems: are we doing better? An analysis of trauma mortality patterns, 1997-2008. J Trauma 2010;69:620–626. [DOI] [PubMed] [Google Scholar]
- 29.West JG, Cales RH, Gazzaniga AB. Impact of regionalization: The Orange County experience. Arch Surg 1983;118:740–744. [DOI] [PubMed] [Google Scholar]
- 30.Cales RH. Trauma mortality in Orange County: the effect of implementation of a regional trauma system. Ann Emerg Med 1984;13:1–10. [DOI] [PubMed] [Google Scholar]
- 31.No authors listed. N.I.C.E. Hip fracture: The management of hip fracture in adults, 2011. http://www.nice.org.uk/nicemedia/live/13489/54918/54918.pdf (date last accessed 14 May 2014).
- 32.Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ 2010;182:1609–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moja L, Piatti A, Pecoraro V, et al. Timing matters in hip fracture surgery: patients operated within 48 hours have better outcomes: a meta-analysis and meta-regression of over 190,000 patients. PloS one 2012;7:46175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clague JE, Craddock E, Andrew G, Horan MA, Pendleton N. Predictors of outcome following hip fracture: admission time predicts length of stay and in-hospital mortality. Injury 2002;33:1–6. [DOI] [PubMed] [Google Scholar]
- 35.Incalzi RA, Capparella O, Gemma A, et al. Predicting in-hospital mortality after hip fracture in elderly patients. J Trauma 1994;36:79–82. [DOI] [PubMed] [Google Scholar]
- 36.Esposito TJ, Sanddal ND, Hansen JD, Reynolds S. Analysis of preventable trauma deaths and inappropriate trauma care in a rural state. J Trauma 1995;39:955–962. [DOI] [PubMed] [Google Scholar]
- 37.Maio RF, Burney RE, Gregor MA, Baranski MG. A study of preventable trauma mortality in rural Michigan. J Trauma 1996;41:83–90. [DOI] [PubMed] [Google Scholar]
- 38.Yousri TA, Khan Z, Chakrabarti D, Fernandes R, Wahab K. Lean thinking: can it improve the outcome of fracture neck of femur patients in a district general hospital? Injury 2011;42:1234–1237. [DOI] [PubMed] [Google Scholar]
- 39.No authors listed. CEC. Fractured Hip Surgery in the Elderly. 2011; Available from: http://www.cec.health.nsw.gov.au/__documents/programs/patient-safety/patient-safety-report-hip-fractures-1.pdf (date last accessed 14 May 2014).
- 40.No authors listed. BOA. The care of patients with fragility fractures (also known as the Blue Book), 2007. http://www.boa.ac.uk/Publications/Pages/Bluebooks.aspx (date last accessed 14 May 2014).
- 41.No authors listed. NHFD. National Report 2011 Summary, 2011. http://www.nhfd.co.uk/003/hipfracturer.nsf/NHFDNationalReport2011_Final.pdf (date last accessed 14 May 2014).
- 42.Hindmarsh DM, Hayen A, Finch CF, Close JC. Relative survival after hospitalisation for hip fracture in older people in New South Wales, Australia. Osteoporosis Int 2009;20:221–229. [DOI] [PubMed] [Google Scholar]
- 43.Curtis KA, Mitchell RJ, Chong SS, et al. Injury trends and mortality in adult patients with major trauma in New South Wales. Med J Aust 2012;197:233–237. [DOI] [PubMed] [Google Scholar]
- 44.Lau TW, Leung F, Siu D, Wong G, Luk KD. Geriatric hip fracture clinical pathway: the Hong Kong experience. Osteoporos Int 2010;21(Suppl):S627–S636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.White SM, Griffiths R. Projected incidence of proximal femoral fracture in England: a report from the NHS Hip Fracture Anaesthesia Network (HIPFAN). Injury 2011;42:1230–1233. [DOI] [PubMed] [Google Scholar]