Abstract
Background
Helicopter emergency medical services (EMS) transport is expensive, and previous work has shown that cost-effective use of this resource is dependent on the proportion of minor injuries flown. To understand how over-triage to helicopter EMS versus ground EMS can be reduced, it is important to understand factors associated with helicopter transport of patients with minor injuries.
Objectives
The aim was to characterize patient and hospital characteristics associated with helicopter transport of patients with minor injuries.
Methods
This was a retrospective analysis of adults ≥18 years who were transported by helicopter to Level I/II trauma centers from 2009 through 2010 as identified in the National Trauma Data Bank. Minor injuries were defined as all injuries scored at an Abbreviated Injury Scale (AIS) < 3. Patient and hospital characteristics associated of being flown with only minor injuries were compared in an unadjusted and adjusted fashion. Hierarchical, multivariate logistic regression was used to adjust for patient demographics, mechanism of injury, presenting physiology, injury severity, urban-rural location of injury, total EMS time, hospital characteristics, and region.
Results
A total of 24,812 records were identified, corresponding to 76,090 helicopter transports. The proportion of helicopter transports with only minor injuries was 36% (95% confidence interval [CI] = 34% to 39%). Patient characteristics associated with being flown with minor injuries included being uninsured (odds ratio [OR] 1.36, 95% CI = 1.26 to 1.47), injury by a fall (OR 1.32, 95% CI = 1.20 to 1.45), or other penetrating trauma (OR 2.52, 95% CI = 2.12 to 3.00). Being flown with minor injuries was more likely if the patient was transported to a trauma center that also received a high proportion of patients with minor injuries by ground EMS (OR 1.89, 95% CI = 1.58 to 2.26) or a high proportion of EMS traffic by helicopter (OR 1.35, 95% CI = 1.02 to 1.78). No significant association with urban-rural scene location, or total EMS time was found.
Conclusions
Better recognizing which patients with falls and penetrating trauma have serious injuries that could benefit from being flown may lead to the more cost-effective use of helicopter EMS. More research is needed to determine why patients without insurance, who are most at risk for high out-of-pocket expenses from helicopter EMS, are at higher risk for being flown when only having minor injuries. This suggests that interventions to optimize cost-effectiveness of helicopter transport will likely require an evaluation of helicopter triage guidelines in the context of regional and patient needs.
INTRODUCTION
Unintentional injuries are a leading cause of death in the United States for people under the age of 44 years, and the fifth leading cause of death for all age groups, accounting for approximately 121,000 deaths in 2010.1 The development of helicopter emergency medical services (EMS) was, in part, a means to provide advanced critical care and rapidly transport patients from the scene of injury to trauma centers due to their ability to fly over terrain and access remote locations. In 2010, there were 74 air ambulance companies operating approximately 850 helicopters flying around 400,000 EMS missions yearly.2
While earlier studies using regional databases found mixed evidence for the clinical benefit of helicopter EMS,3–12 more recent studies using the National Trauma Data Bank (NTDB) found that odds of death were 14% to 39% lower for patients transported by helicopter EMS than by ground EMS.13,14 Patients transported by helicopter EMS were also, on average, more severely injured and more likely to benefit from transport.15,16 However, a large fraction of patients transported by helicopter had minor injuries, with regional studies finding 60% of patients had minor injuries, and NTDB studies finding 57% of patients had minor injuries, as defined by an Injury Severity Score (ISS) < 15.17 However, because the ISS was designed to quantify disseminated transfer of mechanical energy to the human body, it does not capture isolated injuries as well as the Abbreviated Injury Scale (AIS).18 Thus, these estimates of minor injury transports are limited because there are many patients with an ISS < 15 who have severe focal and time-sensitive injuries that could potentially benefit from helicopter transport.
Moreover, there are significant financial and personnel costs with helicopter EMS programs. A survey of providers found individual institutional costs ranging from $114,777 to $4.5 million per year,19 and hourly operational costs of about $5,000, which is approximately 10 to 15 times the cost of a ground EMS unit.17 The average charge per transport for the largest U.S. privately owned helicopter EMS program have risen from $13,000 per transport in 2007 to over $36,000 per transport in 2013.20 Based on a previous cost-effectiveness analysis, it was found that the cost-effectiveness of helicopter transport is highly dependent on reducing the proportion of patients with minor injuries.21 Furthermore, the NTSB has investigated 230 helicopter EMS crashes since 1983, and between 2003 and 2010, there were 99 crashes with 99 fatalities.22 Given the high costs and inherent risks associated with helicopter transport, there is a need to better understand factors associated with the high rates of minor injury transports by helicopter.
The aim of this study was to identify patient- and hospital-level factors associated with the helicopter EMS transport of patients with minor injuries to inform policy and guideline development. More efficient usage of this resource would lead to improved cost-effectiveness and potentially limit patients’ and operators’ exposure to personal expense and risks.
METHODS
Study Design
This study was a retrospective analysis using the NTDB National Sample Program (NSP) for admissions in 2009 and 2010. The NSP contains data collected from 95 Level I and II trauma centers with survey weights to estimate national level statistics for the 453 Level I and II trauma centers in the United States. We reported nationally weighted estimates. We received a waiver from informed consent requirements from the Stanford University School of Medicine’s institutional review board for this study.
Study Setting and Population
Inclusion criteria included all helicopter scene transports for patients 18 years of age and older in the United States. We excluded helicopter transports associated with inter-facility transfers. Records with an unknown mode of transportation, patient age, or AIS score were also excluded.
Outcome Measures
The primary outcome of interest is the transport of patients with minor injuries by helicopter EMS. Our primary definition of having only minor injuries is a maximum AIS score < 3. This study uses AIS as the primary measure of minor injury because it is a more conservative measure that considers patients who may have isolated serious injuries. In a secondary analysis, we examined the proportion of patients flown with ISS < 15. The NTDB provides hospital-calculated AIS and ISS codes, as well as International Classification of Diseases, ninth revision, Clinical Modification (ICD-9-CM) derived diagnosis codes. We used ICD-9-CM derived injury severity where possible. For incidents where the calculated AIS scores were missing (886, 3.5%), we substituted hospital-assigned AIS scores from the NTDB.
Data Analysis
We tabulated the patient and hospital characteristics of helicopter transports to Level I and Level II trauma centers using the NTDB sampling weights and strata to produce nationally weighted patient-level estimates. Patient characteristics were also tabulated by the primary outcome of transports, with a maximum AIS score < 3 versus ≥ 3. To analyze hospital characteristics, overall trauma volume, non-interfacility helicopter and ground EMS transport volume, and the fraction of ground EMS transports for patients 18 years of age and older for minor injuries (AIS < 3) were calculated for each hospital. Records were then divided into quartiles based on the hospital characteristics and tabulated by the primary outcome of AIS < 3.
To test unadjusted differences in the likelihood of experiencing a helicopter transport with minor injury vs. serious injuries according to patient and hospital characteristics, we used chi-square tests. To identify factors independently associated with being flown with minor injuries, we used sample-weighted multivariate logistic regression with covariates chosen to include a broad range of patient and hospital characteristics that could reasonably influence the decision to transport by helicopter. The model was adjusted for patient characteristics including age, sex, and insurance status. Adjustment was also made for incident characteristics, such as injury mechanism, urban influence code > 2 (representing a rural location), total EMS time, EMS transport time, EMS-measured systolic blood pressure (sBP), and Glasgow Coma Scale (GCS) score. The regression model also adjusts for hospital level characteristics, including the Level I status of the hospital, the region where the hospital is located, the annual total volume of the hospital, the annual volume of helicopter transports, the percentage of EMS transports by helicopter, the minor injury transport rate for ground EMS transports, and the mean total EMS time for ground and helicopter transports. The covariates were examined for multicollinearity, and variance inflation factor were calculated for each covariate. We found the mean variance inflation factor among variables was 1.77 and the maximum was 4.81, indicating acceptable levels of multicollinearity between the covariates.
Based on best practices for analyses using the NTDB, all missing data were handled with multiple imputation by chained equations using previously published multiple imputation models appropriate for the imputation of missing EMS and hospital collected trauma registry data.23–27 We created 10 imputation datasets. The regression analysis run on the 10 imputation datasets and the final results were obtained through Rubin’s rules of combination.28 We used STATA 13/IC for all analyses.
RESULTS
There were an estimated 76,090 (95% CI = 63,019 to 89,160) patients transported by helicopter from the scene of injury to U.S. Level I and II trauma centers in 2009-2010 (Figure 1). Overall, the majority of patients were male (72%), and were 18 to 35 years of age (40%) (Table 1). Motor vehicle crashes (MVCs) accounted for the majority of transports (47%). Of the transports with data, the majority (53%) originated from urban areas, with overall EMS run times more than 60 minutes (49%). Helicopter transport times were frequently under 30 minutes (52%).
Figure 1.
Flowchart detailing exclusion criteria.
AIS = Abbreviated Injury Scale
Table 1.
Minor and major injury helicopter transports stratified by patient characteristics.
| Characteristic | Overall | Minor Injury (AIS< 3) |
Severe Injury (AIS ≥ 3) |
||||
|---|---|---|---|---|---|---|---|
| Weighted N |
Column Percent |
Weighted N |
Column Percent |
Weighted N |
Column Percent |
P | |
| Total patients | 76,090 | - | 27,673 | - | 48,418 | - | |
| Age, yrs | <0.001 | ||||||
| 18-35 | 29,943 | 39 | 11,070 | 40 | 18,873 | 39 | |
| 35-55 | 27,692 | 36 | 10,421 | 38 | 17,271 | 36 | |
| 55-70 | 12,769 | 17 | 4,406 | 16 | 8,363 | 17 | |
| >70 | 5,686 | 7 | 1,776 | 6 | 3,911 | 8 | |
| Sex | <0.001 | ||||||
| Female | 21,256 | 28 | 8,255 | 30 | 13,001 | 27 | |
| Male | 54,814 | 72 | 19,413 | 70 | 35,401 | 73 | |
| Insurance | <0.001 | ||||||
| Private medical | 22,855 | 30 | 7,895 | 29 | 14,960 | 31 | |
| Automotive | 7,743 | 10 | 2,633 | 10 | 5,110 | 11 | |
| Medicare | 7,189 | 9 | 2,491 | 9 | 4,698 | 10 | |
| Medicaid | 5,573 | 7 | 1,900 | 7 | 3,674 | 8 | |
| Uninsured | 14,639 | 19 | 6,209 | 22 | 8,430 | 17 | |
| Other | 6,800 | 9 | 2,826 | 10 | 3,974 | 8 | |
| Injury mechanism | <0.001 | ||||||
| Motor vehicle | 35,441 | 47 | 12,055 | 44 | 23,386 | 49 | |
| Fall | 8,330 | 11 | 3,444 | 12 | 4,886 | 10 | |
| Motor/pedal cyclist | 10,562 | 14 | 3,250 | 12 | 7,312 | 15 | |
| Other blunt | 12,153 | 16 | 4,625 | 17 | 7,528 | 16 | |
| Firearm | 4,159 | 5 | 1,217 | 4 | 2,943 | 6 | |
| Other penetrating | 2,184 | 3 | 1,298 | 5 | 887 | 2 | |
| EMS blood pressure | <0.001 | ||||||
| sBP ≥ 110 mm Hg | 49,517 | 65 | 19,871 | 72 | 29,645 | 61 | |
| sBP < 110 mm Hg | 11,656 | 15 | 2,836 | 10 | 8,820 | 18 | |
| EMS Glasgow Coma Scale | <0.001 | ||||||
| GCS = 15 | 36,049 | 47 | 16,207 | 59 | 19,842 | 41 | |
| GCS < 15 | 26,151 | 34 | 6,746 | 24 | 19,405 | 40 | |
| Scene location | 0.644 | ||||||
| Urban | 23,539 | 31 | 8,838 | 32 | 14,701 | 30 | |
| Rural | 20,703 | 27 | 7,930 | 29 | 12,773 | 26 | |
| Total EMS time (min) | 0.007 | ||||||
| < 30 | 864 | 1 | 340 | 1 | 524 | 1 | |
| 30-45 | 9,548 | 13 | 3,579 | 13 | 5,969 | 12 | |
| 45-60 | 17,111 | 22 | 6,745 | 24 | 10,366 | 21 | |
| >60 | 26,373 | 35 | 9,218 | 33 | 17,155 | 35 | |
| EMS transport time (min) | 0.146 | ||||||
| < 30 | 39,906 | 52 | 14,841 | 54 | 25,066 | 52 | |
| 30-45 | 9,583 | 13 | 3,603 | 13 | 5,980 | 12 | |
| 45-60 | 1,915 | 3 | 657 | 2 | 1,258 | 3 | |
| >60 | 964 | 1 | 285 | 1 | 679 | 1 | |
AIS = Abbreviated Injury Scale; sBP = systolic blood pressure
Patients with minor injuries comprised 36% (95% CI = 34% to 39%) of all helicopter transports. Compared to patients with severe injuries, there were some statistically significant differences in baseline patient characteristics. Patients with minor injuries transported by helicopter were more often uninsured (22% vs. 17%, p < 0.001). A higher proportion of patients with minor injuries experienced a fall mechanism (12% vs. 10%, p < 0.001) or other penetrating injuries (5% vs. 2%, p < 0.001). A higher proportion of minor injury patients also had sBP > 110 mm Hg (72% vs. 61%, p < 0.001), and GCS of 15 (71% vs. 51%, p < 0.001), as well as a total EMS time of > 60 min (50% vs. 46%, p < 0.007). We found major and minor injury patients differed little with regard to scene location and EMS transport time.
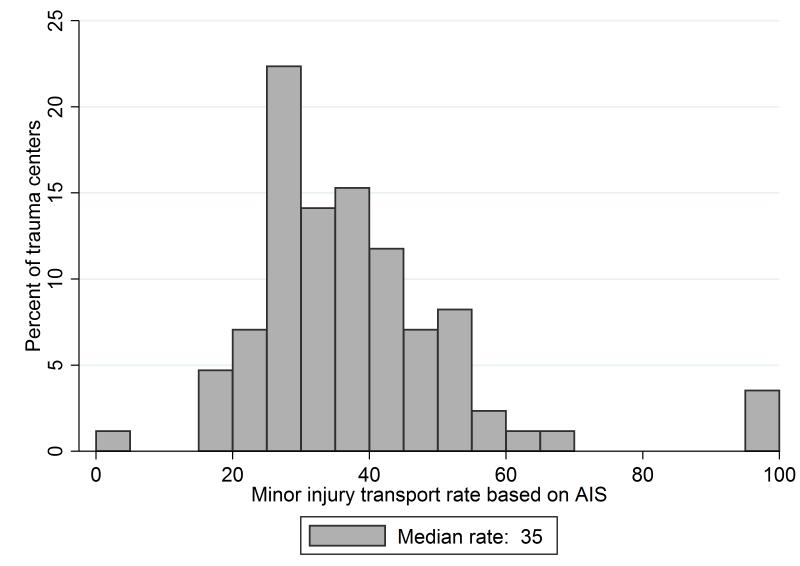
Hospital characteristics were also evaluated (Table 2). Overall, the South had the largest number of transports (57%), and the Northeast region had the fewest (8%). The majority of transports were treated at a Level 1 trauma center (73%). Figure 2 shows the distribution of helicopter minor injury transport rates across the 85 hospitals represented in the NSP. The median rate is 35%, with a range of 0% to 100%. For hospitals with annual helicopter volume of 10 or more transports, the rate of minor injury transport ranged from 16% to 58%.
Table 2.
Minor and major injury helicopter transports stratified by trauma center characteristics
| Characteristic | Overall | Minor Injury (AIS< 3) |
Severe Injury (AIS ≥ 3) |
||||
|---|---|---|---|---|---|---|---|
| Weighted N |
Column Percent |
Weighted N |
Column Percent |
Weighted N |
Column Percent |
P | |
| Region | 0.255 | ||||||
| Midwest | 12,543 | 16 | 4,648 | 17 | 7,895 | 16 | |
| Northeast | 5,645 | 7 | 1,959 | 7 | 3,686 | 8 | |
| South | 43,773 | 58 | 16,532 | 60 | 27,240 | 56 | |
| West | 14,130 | 19 | 4,534 | 16 | 9,597 | 20 | |
| Designation | 0.474 | ||||||
| Level I | 56,041 | 74 | 20,115 | 73 | 35,926 | 74 | |
| Level II | 20,049 | 26 | 7,557 | 27 | 12,492 | 26 | |
| Mean annual trauma volume | <0.001 | ||||||
| First quartile (53-1,469) | 19,024 | 25 | 7,154 | 26 | 11,870 | 25 | |
| Second quartile (1,474-1,978) | 19,067 | 25 | 8,333 | 30 | 10,735 | 22 | |
| Third quartile (2,054-2,876) | 20,972 | 28 | 6,899 | 25 | 14,072 | 29 | |
| Fourth quartile (3,032-5,894) | 17,028 | 22 | 5,286 | 19 | 11,741 | 24 | |
| Mean annual HEMS volume | <0.001 | ||||||
| First quartile (1-216) | 20,402 | 27 | 6,994 | 25 | 13,408 | 28 | |
| Second quartile (221-294) | 19,117 | 25 | 8,643 | 31 | 10,474 | 22 | |
| Third quartile (301-381) | 18,115 | 24 | 6,123 | 22 | 11,992 | 25 | |
| Fourth quartile (386-642) | 18,456 | 24 | 5,912 | 21 | 12,544 | 26 | |
| % EMS transports by helicopter | 0.001 | ||||||
| First quartile (0-10) | 19,514 | 26 | 6,341 | 23 | 13,173 | 27 | |
| Second quartile (11-14) | 20,196 | 27 | 6,428 | 23 | 13,768 | 28 | |
| Third quartile (14-18) | 18,220 | 24 | 7,923 | 29 | 10,297 | 21 | |
| Fourth quartile (19-31) | 18,161 | 24 | 6,980 | 25 | 11,180 | 23 | |
| % Ground EMS AIS < 3 | <0.001 | ||||||
| First quartile (10-26) | 19,199 | 25 | 6,252 | 23 | 12,948 | 27 | |
| Second quartile (26-33) | 19,425 | 26 | 5,828 | 21 | 13,597 | 28 | |
| Third quartile (33-37) | 18,691 | 25 | 7,815 | 28 | 10,877 | 22 | |
| Fourth quartile (38-71) | 18,775 | 25 | 7,778 | 28 | 10,997 | 23 | |
| Mean total ground EMS time | <0.154 | ||||||
| First quartile (33-43) | 19,434 | 26 | 7,405 | 27 | 12,030 | 25 | |
| Second quartile (43-46) | 19,016 | 25 | 6,558 | 24 | 12,458 | 26 | |
| Third quartile (46-48) | 21,780 | 29 | 8,541 | 31 | 13,239 | 27 | |
| Fourth quartile (48-63) | 15,784 | 21 | 5,124 | 19 | 10,659 | 22 | |
| Mean total helicopter EMS time | <0.001 | ||||||
| First quartile (39-56) | 19,034 | 25 | 7,850 | 29 | 11,184 | 23 | |
| Second quartile (56-63) | 22,488 | 30 | 8,719 | 32 | 13,768 | 29 | |
| Third quartile (64-70) | 16,104 | 21 | 4,750 | 17 | 11,354 | 24 | |
| Fourth quartile (72-104) | 18,083 | 24 | 6,223 | 23 | 11,859 | 25 | |
HEMS = helicopter EMS; AIS = Abbreviated Injury Scale
Figure 2.
Histogram of minor injury (AIS < 3) helicopter transport rates for the 85 trauma centers in the NTDB receiving helicopter traffic.
We noted no significant differences by region or trauma center designation between minor and severely injured patients. Hospitals in the two lowest quartiles for mean annual trauma volume (53 to 1,978 patients per year) received a larger proportion of minor injury transports (56% vs. 47%, p < 0.001). Similarly, hospitals in the two lowest quartiles for mean annual helicopter EMS volume (1 to 294) had a higher proportion of minor injury transports (56% vs. 50%, p < 0.001), as did hospitals in the higher two quartiles of EMS calls (14% to 31%) transported by helicopter (54% vs 44%, p = 0.001). Hospitals in the highest two quartiles of ground EMS minor injury transport rates (33% to 71%) also had a high proportion of helicopter patients with minor injuries (56% vs. 45%, p < 0.001). Finally, hospitals receiving flights in the lowest two quartiles for total helicopter EMS time (39 to 63 min) received a higher proportion of minor injury transports (61% vs. 52%, p < 0.001).
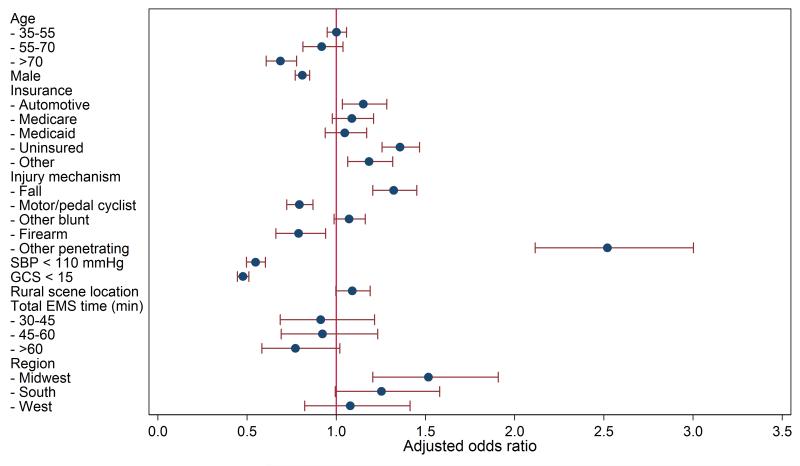
We found that most of the factors that had unadjusted associations with minor injury transport remained significant after multivariate adjustment (Figure 3). Characteristics independently associated with minor injury helicopter transport included lack of patient insurance (adjusted odds ratio [OR] 1.36, 95% CI = 1.26 to 1.47), fall as the mechanism of injury (OR 1.32, 95% CI = 1.20 to 1.45), and other penetrating injuries (OR 2.52, 95% CI = 2.12 to 3.00). Male sex was less often associated with minor injury helicopter transport (OR 0.81, 95% CI = 0.77 to 0.85), as was age older than 70 years (OR 0.69, 95% CI = 0.61 to 0.78). As expected, patients’ physiologic stability was inversely associated with minor injury transport. An sBP < 110 mm Hg (OR 0.55, 95% CI = 0.50 to 0.60) or GCS < 15 (OR 0.48, 95% CI = 0.45 to 0.51) had lower odds ratios of minor injury helicopter transport.
Figure 3.
Adjusted odds ratios and 95% confidence intervals for AIS score < 3 helicopter transport associated with a) patient characteristics, and b) hospital characteristics, from a logistic regression analysis.
Hospital characteristics were associated with the transport of minor injury patients as well. Hospitals with high annual trauma patient volumes (2,054 to 5,894 patients) were associated with lower odds of minor injury transports (3rd quartile: OR 0.77, 95% CI = 0.64 to 0.94, 4th quartile: OR 0.75, 95% CI = 0.58 to 0.96). High proportions of transports by helicopter (14% to 31%) were also significantly associated with minor injury transports (3rd quartile: OR 1.49, 95% CI = 1.09 to 2.09; 4th quartile: OR 1.35, 95% CI = 1.02 to 1.78). There were regional differences in transport of patients with minor injuries, with higher odds in the Midwest as compared to the Northeast (OR 1.52, 95% CI = 1.20 to 1.91). Higher rates of ground EMS minor injury transport (33% to 71%) were also associated with helicopter minor injury transport (3rd quartile: OR 1.64, 95% CI = 1.34 to 2.00, 4th quartile: OR 1.89, 95% CI = 1.58 to 2.26).
DISCUSSION
We found the overall rate of minor injury transports for helicopter EMS to be 36%, which is likely to represent a more reliable estimate of low-risk patients that could potentially have been safely transported by ground EMS than previous estimates based on the ISS. We also found a large trauma center variation in the rate of minor injury (AIS < 3) transports ranging from 16% to 58% in trauma centers with more than 10 transports per year. While certainly geographic and logistical differences likely account for a portion in this variation, our findings suggest there is room for reducing the use of helicopter transport for minor injury patients. When we used ISS < 15 as a cutoff, the rate was 59%, comparable to rates of 57% to 60% found in other studies.14,15,17 The proportion of patients with ISS < 15 flown to trauma centers is nearly twice as high as the overtriage rate that would be expected with adherence to the American College of Surgeons field triage guidelines (34.3%). This suggests that promoting adherence to these guidelines could reduce the reduce the proportion of non-severely injured patients who are flown to trauma centers.29
Our results show that several patient characteristics are more likely to be associated with patients transported for minor injuries. We were surprised to learn that scene location and EMS transport time were not characteristics associated with minor injury transports. This argues against the notion that helicopters are being used to overcome distance and time barriers for minor injury patients. Falls and penetrating mechanisms of injury were associated in unadjusted and adjusted analyses. This result is not surprising given the dramatic presentation of these injuries and suggests current field triage methods have difficulty assessing injury severity in patients with these mechanisms of injury as compared to other mechanisms. In addition, our analysis shows uninsured patients are more likely to be minor injury helicopter transports. It is unclear why these patients are more likely to be flown with minor injuries, although previous work found a similar link between uninsured patients and the use of ground ambulances for non-emergencies as a means of travelling to the hospital.30 The bill from helicopter transport, reported to be as high as $30,000 to 40,000,20 can impose on uninsured patients significant financial liabilities, and further investigation will be necessary to determine the extent of this disparity and the underlying cause.
Some hospital characteristics were also associated with minor injury helicopter transport. Hospitals in the Midwest were significantly more likely to receive minor injury helicopter transports than those in other regions. This difference is likely due to multiple factors, including the long distances between hospitals, the presence of many rural communities, decreased availability of ground ambulances for long distance transport, and lower population densities. Further investigation is necessary to determine the differences in the helicopter EMS systems of the four census regions and their implications on minor injury transports. In addition, hospitals in the top two quartiles for the fraction of EMS transports by helicopter were more likely to receive patients with minor injuries by helicopter. This result suggests areas where helicopters are prevalent will more likely use them with minor injury patients, increasing the fraction of EMS transports arriving by helicopter. Hospitals in the top two quartiles for ground ambulance minor injury transport were also more significantly likely to receive minor injuries by helicopter. The relationship between ground and helicopter minor injury transport suggests that the character of the overall EMS system plays a significant role, and efforts to decrease minor injury transport rates by regional policymakers should consider interaction between ground and helicopter EMS services.
Reducing the overall number of medically unnecessary helicopter transports is the most efficient method for increasing the cost-effectiveness of the intervention, and the results of this work indicate some areas for improvement. Significant associations with falls and penetrating mechanisms of injury suggest additional work is necessary to improve field triaging of these patients. Further work is also necessary to investigate the significant association of uninsured patients with minor injury transports, which can unnecessarily burden those least able to pay for this expensive intervention.
However, these associations account for a small fraction of the overall minor injury transport volume. Individually, the previously highlighted characteristics are associated with a 2 to 10 percentage point increase in minor injury transport, as shown by the unadjusted analysis. A large proportion of minor injury transports are unaccounted for, seeming to indicate the field triage system appears to correlate poorly with the AIS of helicopter transport patients. Further work is needed to determine what updates are necessary to better differentiate major and minor injury patients. One possible explanation for high rates of minor injury helicopter transport may be that the decision to fly is likely pre-determined once a helicopter has been deployed to the scene, even if there is no medical need. Another explanation is the utilization of the helicopter is dependent on a confounding factor, such as patient choice, which has been shown to affect destination decisions in EMS.31 Additional work should also examine upstream decision points, such as the factors influencing the decision to dispatch a helicopter. Characterization of and improvements in upstream decision points should also help alleviate the difficulties with the field triaging system.
LIMITATIONS
While the collection of data in the NTDB has greatly improved since 2007, a significant amount of data is missing from several variables. In particular, scene location data are missing from almost 40% of the incidents, and total EMS time data is missing from about 30% of the incidents, which this study addressed using multiple imputation. Furthermore, urban and rural scene location is not directly indicative of distance from the hospital, which makes it difficult to characterize minor injury transport rates as a function of distance from the hospital. In addition, the analysis performed in this study is inherently descriptive, and cannot establish causality between minor injury transport and patient or trauma center characteristics. Moreover, because the final outcome of minor injury is determined using hospital diagnosis data, this study cannot provide insight into the reasoning or process that led field personnel to transport a patient by helicopter instead of ground ambulance. This method of outcome determination also limits the ability of this study to characterize true over-triage, and instead is able to determine only if patients had minor injuries.
CONCLUSIONS
This study has identified characteristics associated with the transport of patients with minor injuries by helicopter. Patients suffering from falls and other penetrating injuries are associated with minor injury helicopter transport. Updated field triage protocols should focus on differentiating serious from minor injuries among patients with those mechanisms of injury. Transport of minor injuries by helicopter is also associated with lack of insurance and with hospitals that have high rates of ground ambulance minor injury transport. Future helicopter triage guideline development is necessary to manage this limited and expensive resource, and to avoid burdening patients with financial liability for unnecessary care.
Acknowledgments
The project was supported by Award Number K12HL109009 from the National Heart, Lung, and Blood Institute (Delgado). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health. This project was also funded in part by the Stanford University School of Medicine Medical Scholars Research Program.
Footnotes
Prior Presentations: SAEM Mid-Atlantic Regional Meeting, Philadelphia, PA, February 2014.
Disclosures: The authors have no conflicts of interest to disclose.
References
- 1.Centers for Disease Control and Prevention . WISQARS: Web-based injury statistics query and reporting systems. 10 Leading Causes of Death by Age Group; United States: [Accessed Aug 10, 2014]. 2010. Available at: http://www.cdc.gov/injury/wisqars/pdf/10LCID_All_Deaths_By_Age_Group_2010-a.pdf. [Google Scholar]
- 2.Federal Aviation Administration [Accessed Aug 10, 2014];Fact Sheet – FAA initiatives to improve helicopter air ambulance safety. Available at: http://www.faa.gov/news/fact_sheets/news_story.cfm?newsId=15794.
- 3.Baxt WG, Moody P. The impact of a rotorcraft aeromedical emergency care service on trauma mortality. JAMA. 1983;249(22):3047–51. [PubMed] [Google Scholar]
- 4.Baxt WG, Moody P, Cleveland HC, et al. Hospital-based rotorcraft aeromedical emergency care services and trauma mortality: a multicenter study. Ann Emerg Med. 1985;14(9):859–64. doi: 10.1016/s0196-0644(85)80634-x. [DOI] [PubMed] [Google Scholar]
- 5.Baxt WG, Moody P. The impact of advanced prehospital emergency care on the mortality of severely brain-injured patients. J Trauma. 1987;27(4):365–9. doi: 10.1097/00005373-198704000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Schiller WR, Knox R, Zinnecker H, et al. Effect of helicopter transport of trauma victims on survival in an urban trauma center. J Trauma. 1988;28(8):1127–34. doi: 10.1097/00005373-198808000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Nicholl P, Brazier JE, Snooks HA, Court R, Si S. Effects of London helicopter emergency medical service on survival after trauma. Br Med J. 1995;311:217–22. doi: 10.1136/bmj.311.6999.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brathwaite CE, Rosko M, McDowell R, Gallagher J, Proenca J, Spott MA. A critical analysis of on-scene helicopter transport on survival in a statewide trauma system. J Trauma. 1998;45(1):140–4. doi: 10.1097/00005373-199807000-00029. [DOI] [PubMed] [Google Scholar]
- 9.Chappell VL, Mileski WJ, Wolf SE, Gore DC. Impact of discontinuing a hospital-based air ambulance service on trauma patient outcomes. J Trauma. 2002;52(3):489–91. doi: 10.1097/00005373-200203000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Biewener A, Aschenbrenner U, Rammelt S, Grass R, Zwipp H. Impact of helicopter transport and hospital level on mortality of polytrauma patients. J Trauma. 2004;56(1):94–8. doi: 10.1097/01.TA.0000061883.92194.50. [DOI] [PubMed] [Google Scholar]
- 11.Talving P, Teixeira PGR, Barmparas G, et al. Helicopter evacuation of trauma victims in Los Angeles: does it improve survival? World J Surg. 2009;33:2469–76. doi: 10.1007/s00268-009-0185-1. [DOI] [PubMed] [Google Scholar]
- 12.Bulger EM, Guffey D, Guyette FX, et al. Impact of prehospital mode of transport after severe injury: a multicenter evaluation from the Resuscitation Outcomes Consortium. J Trauma Acute Care Surg. 2013;72(3):1–16. doi: 10.1097/TA.0b013e31824baddf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Galvagno SMJ, Haut ER, Zafar SN, et al. Association between helicopter vs. ground emergency medical services and survival for adults with major trauma. JAMA. 2012;307(15):1602–10. doi: 10.1001/jama.2012.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sullivent EE, Faul M, Wald MM. Reduced mortality in injured adults transported by helicopter emergency medical services. Prehospital Emerg Care. 2011;15(3):295–302. doi: 10.3109/10903127.2011.569849. [DOI] [PubMed] [Google Scholar]
- 15.Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML. Helicopters and the civilian trauma system: national utilization patterns demonstrate improved outcomes after traumatic injury. J Trauma. 2010;69(5):1030–6. doi: 10.1097/TA.0b013e3181f6f450. [DOI] [PubMed] [Google Scholar]
- 16.Cunningham P, Rutledge R, Baker C, Clancy T. A comparison of the association of helicopter and ground ambulance transport with the outcome of injury in trauma patients transported from the scene. J Trauma. 1997;43(6):940–6. doi: 10.1097/00005373-199712000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Bledsoe BE, Wesley K, Eckstein M, Dunn TM, O’Keefe MF. Helicopter scene transport of trauma patients with nonlife-threatening injuries: a meta-analysis. J Trauma. 2006;60(6):1257–66. doi: 10.1097/01.ta.0000196489.19928.c0. [DOI] [PubMed] [Google Scholar]
- 18.Baker S, O’Neill B. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. Trauma Acute Care. 1974;14(3):187–96. [PubMed] [Google Scholar]
- 19.Taylor CB, Stevenson M, Jan S, Middleton PM, Fitzharris M, Myburgh JA. A systematic review of the costs and benefits of helicopter emergency medical services. Injury. 2010;41(1):10–20. doi: 10.1016/j.injury.2009.09.030. [DOI] [PubMed] [Google Scholar]
- 20.Air Methods Corporation [Accessed Aug 10, 2014];Annual Report 2013. Available at: http://www.airmethods.com/airmethods/investors/financial-reports/detail/2014/03/03/air-methods-2013-annual-report#.U-gQQWOK2So.
- 21.Delgado MK, Staudenmayer KL, Wang NE, et al. Cost-effectiveness of helicopter versus ground emergency medical services for trauma scene transport in the United States. Ann Emerg Med. 2013;62(4):351–64. doi: 10.1016/j.annemergmed.2013.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sumwalt RL. [Accessed Aug 10, 2014];Current Issues with Air Medical Transport: EMS Helicopter Safety. Available at: https://www.ntsb.gov/doclib/speeches/sumwalt/Sumwalt_050411.pdf.
- 23.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377–99. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 24.Moore L, Hanley JA, Turgeon AF, Lavoie A, Emond M. A multiple imputation model for imputing missing physiologic data in the National Trauma Data Bank. J Am Coll Surg. 2009;209(5):572–9. doi: 10.1016/j.jamcollsurg.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 25.Newgard CD. The validity of using multiple imputation for missing out-of-hospital data in a state trauma registry. Acad Emerg Med. 2006;13:314–24. doi: 10.1197/j.aem.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 26.Glance LG, Osler TM, Mukamel DB, Meredith W, Dick AW. Impact of statistical approaches for handling missing data on trauma center quality. Ann Surg. 2009;249(1):143–8. doi: 10.1097/SLA.0b013e31818e544b. [DOI] [PubMed] [Google Scholar]
- 27.Moore L, Hanley JA, Lavoie A, Turgeon A. Evaluating the validity of multiple imputation for missing physiological data in the national trauma data bank. J Emerg Trauma Shock. 2009;2(2):73–9. doi: 10.4103/0974-2700.44774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rubin DB, Schenker N. Multiple imputation in health-care databases: an overview and some applications. Stat Med. 1991;10(4):585–98. doi: 10.1002/sim.4780100410. [DOI] [PubMed] [Google Scholar]
- 29.Newgard CD, Staudenmayer K, Hsia RY, et al. The cost of overtriage: more than one-third of low-risk injured patients were taken to major trauma centers. Health Aff (Millwood) 2013;32(9):1591–9. doi: 10.1377/hlthaff.2012.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brown E, Sindelar J. The emergent problem of ambulance misuse. Ann Emerg Med. 1993;22:646–50. doi: 10.1016/s0196-0644(05)81841-4. [DOI] [PubMed] [Google Scholar]
- 31.Newgard CD, Mann NC, Hsia RY, et al. Patient choice in the selection of hospitals by 9-1-1 emergency medical services providers in trauma systems. Acad Emerg Med. 2013;20:911–9. doi: 10.1111/acem.12213. [DOI] [PMC free article] [PubMed] [Google Scholar]