Abstract
Background
The single radius total knee prosthesis was introduced with the advantage of reduced patellar symptoms; however, there is no long-term follow-up study of the same. The purpose of this study was to determine the survival rate of single radius posterior-stabilized total knee arthroplasty and patellofemoral complication rates in a consecutive series.
Methods
Seventy-one patients (103 knees) who underwent arthroplasty without patellar resurfacing using a single radius posterior-stabilized total knee prosthesis were followed up for a minimum 10 years. Clinical evaluation using Knee Society knee and function scores and radiologic evaluation were performed at regular intervals. Anterior knee pain as well as patellofemoral complications were evaluated with a simple questionnaire. The Kaplan-Meier product-limit method was used to estimate survival.
Results
Seventeen patients (23 knees) were excluded due to death (12 knees) or lost to follow-up (11 knees). Of the 80 knees enrolled, all femoral components and 78 tibial components were well fixed without loosening at final follow-up. Two revisions were performed because of tibial component loosening and periprosthetic joint infection. One patient with tibial component loosening refused to have revision surgery. No obvious tibial insert polyethylene wear was observed. The survivorships at 132 months were 96.7% using revision or pending revision as end points. Anterior knee pain was present in 6 patients (6 knees, 7.5%) at the latest follow-up. No patellofemoral complication requiring revision was encountered.
Conclusions
The single radius posterior-stabilized total knee prosthesis demonstrated an excellent minimum 10-year survivorship. The low rates of implant loosening and 7.5% of anterior knee pain as a patellofemoral complication are comparable with those reported for other modern total knee prosthesis.
Keywords: Arthroplasty, Replacement, Knee, Single-radius, Survival rate
Total knee arthroplasty (TKA) is a well-established treatment for end stage degenerative knee joints. Recently, excellent long-term survivorships of 91% to 100% have been reported for TKA.1,2) However, patellofemoral complications are among the most common causes of revision surgery following primary TKA.3) In 1996, the Scorpio single radius total knee system was introduced with the advantage of reduced patellar symptoms, as compared to conventional knee prosthesis. To date mid-term follow-up results for Scorpio total knee system have shown a 95% to 99% survival rate and reduced the patellofemoral complications.4,5,6,7,8,9) The only study of long-term outcomes for this device indicated favorable clinical outcomes at 5 to 9.5 years.9) However, the results focused on survival alone without addressing patellofemoral complications.
Patellar resurfacing during TKA is the most common method used. However, patellar resurfacing related complications include chronic pain, component wear, loosening, patellar fracture, patellar clunk syndrome, and osteonecrosis. Thus, patellar resurfacing during TKA is still questionable. Therefore the purpose of this long-term follow-up study was to determine the survival rate of Scorpio single radius posterior-stabilized TKA and to document patellofemoral complication rates in a consecutive series.
METHODS
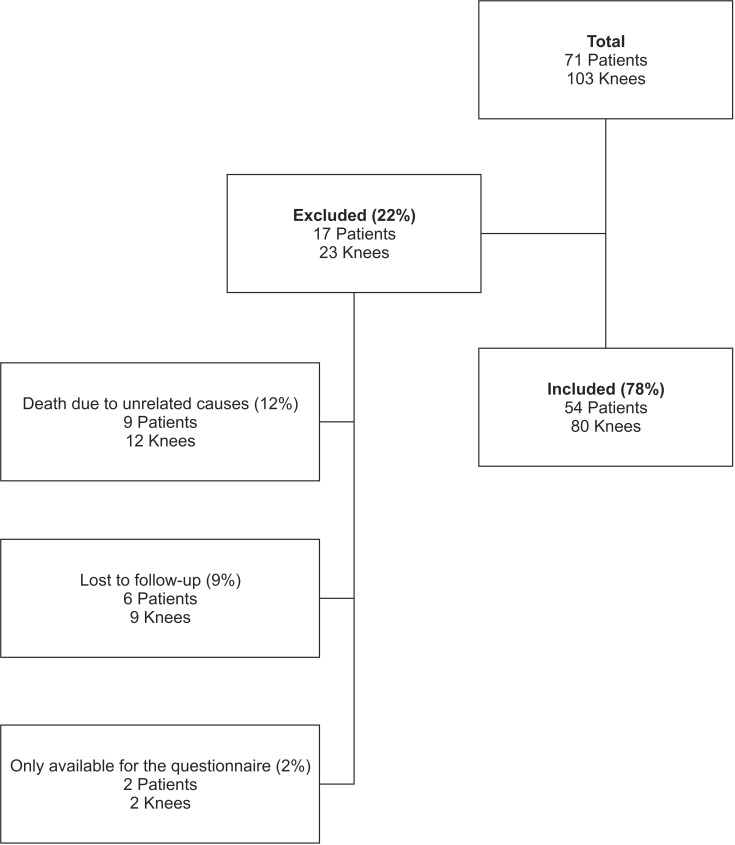
This retrospective observational study was approved by the Institutional Review Board of Chung-Ang University Hospital and all patients provided informed consent. Between January 2000 and April 2001, a consecutive series of 103 TKAs were performed in 71 patients using the Scorpio (Stryker Orthopaedics, Mahwah, NJ, USA) single radius posterior-stabilized total knee prosthesis by one surgeon. The initial diagnoses were primary osteoarthritis in 98 knees (66 patients), posttraumatic arthritis in 3 knees (3 patients), and rheumatoid arthritis in 2 knees (2 patients) (Fig. 1). Of these 71 patients, 17 patients (23 knees) were excluded from the study; 9 patients (12 knees) died of unrelated causes with the index TKA in situ at a mean of 5.9 years postoperatively (range, 1.5 to 8.5 years). Six patients (9 knees) could not be located and were considered lost to follow-up, and 2 patients (2 knees) could only be accessed by questionnaire administered by their primary care physician. Complete radiographic and clinical follow-up details were available for a minimum of 10 years (range, 10 to 11 years) for the remaining 54 patients (80 knees; 50 women and 4 men) (Fig. 1). The mean age of patients at the time of index surgery was 66 years (range, 48 to 77 years) (Table 1).
Fig. 1.
A flowchart showing the flow of patients through the study.
Table 1.
Demographic Data
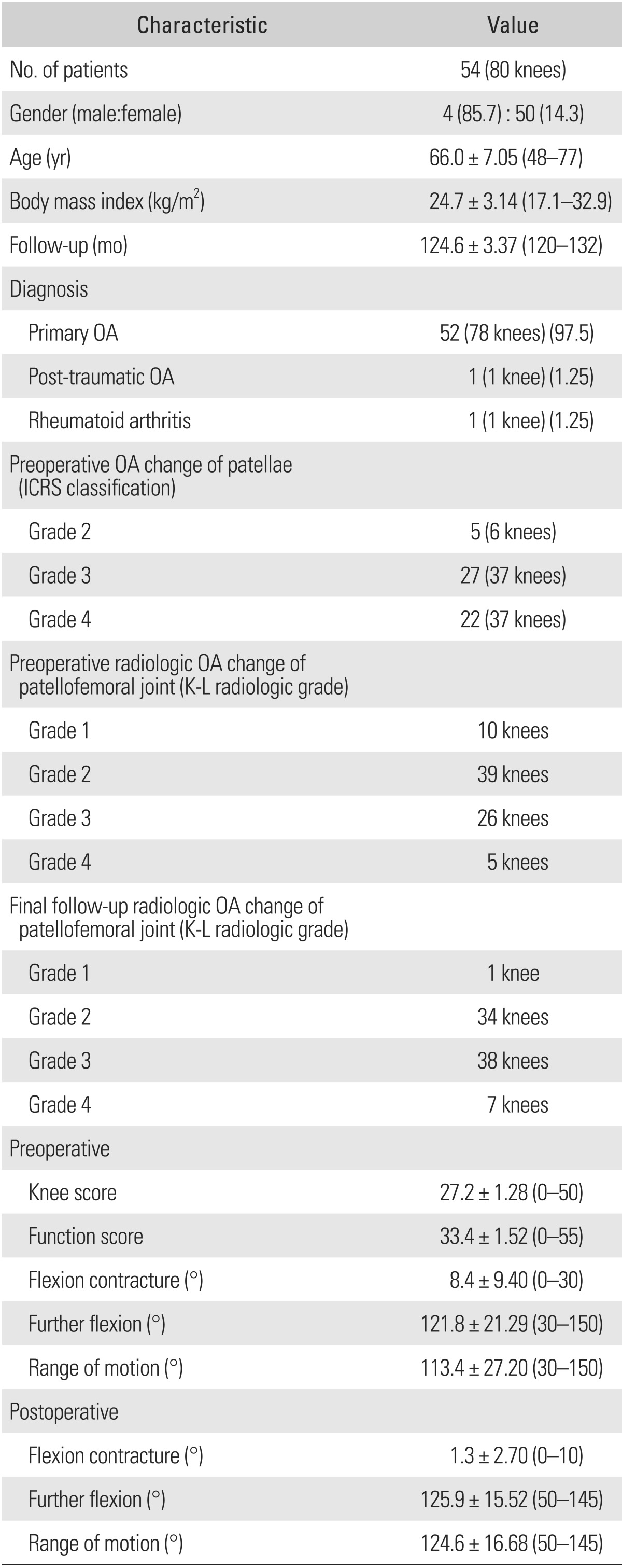
Values are presented as number (%) or mean ± standard deviation (range).
OA: osteoarthritis, ICRS: International Cartilage Repair Society, K-L: Kellgren-Lawrence.
All surgical procedures were performed by a single surgeon using the standard medial parapatellar approach, with sacrifice of anterior and posterior cruciate ligaments in all patients. After lateral subluxation of the patella, the intramedullary canal was accessed by drilling a hole located about 1 cm anterior to the center of the intercondylar notch. An epicondylar reference guide was placed in the intercondylar notch hole to adjust rotational alignment and femoral alignment guide was inserted into the intramedullary hole. After adjusting external rotation alignment, anterior skim cut, distal femoral resection and anterior, posterior and chamfer resections were performed to remove a thickness of bone equal to that of the femoral component to be inserted. Neutral tibial cuts with a 0° to 5° posterior slope in the sagittal plane were made with an extramedullary tibial guide. Stability and alignment were assessed using the trial components. None of the patella was replaced; only osteophytes were excised in all patients. All implants were inserted with cement. In cases with poor patellar tracking, lateral release was performed using a 'no thumb' technique. Eleven knees had positive finding of no thumb technique and lateral release was performed intraoperatively. Patients were mobilized immediately with weight-bearing as tolerated and active exercises were started under the supervision of a physiotherapist. During follow-up evaluations, the patients that did not return for scheduled visits were contacted by telephone. Two nurses and one private doctor found and visited nonresponders.
Clinical evaluations were performed using the Knee Society rating system.10) Results were classified as excellent (80-100), good (70-79), fair (60-69), or poor (< 60). Radiographic analysis included long leg standing radiography from the pelvis to ankle joint for evaluating the axis, weight-bearing anteroposterior view, non-weight-bearing anteroposterior view, lateral view at 30° flexion, and skyline view of the patella. Each radiograph was assessed using the Knee Society evaluation system.11) Range of motion was measured as the arcs of maximal non-weight-bearing passive flexion using a goniometer.
We defined anterior knee pain as a persistent complaint on standing or stair-climbing, after TKA.12,13) At the time of initiating the study, no scoring system for measuring anterior knee pain had been validated. To determine the presence and severity of anterior knee pain, we asked a simple question to the patients "Do you have pain around the patella during daily living activity including sitting, walking, and climbing up and down stairs?" The patients were asked to describe their level of pain on a scale of 1 to 10 using the visual analog scale (VAS). We described VAS as none (0-2), mild (3-4), moderate (5-7), and severe (8-10). Moderate to severe pain was considered meaningful.
Preoperative osteoarthritic changes of patellae were classified by International Cartilage Repair Society method.14) We compared Kellgren-Lawrence radiologic grade of patellofemoral joint using skyline view at the immediate postoperative time point and latest follow-up state, respectively, to evaluate changes of patellofemoral osteoarthritis.
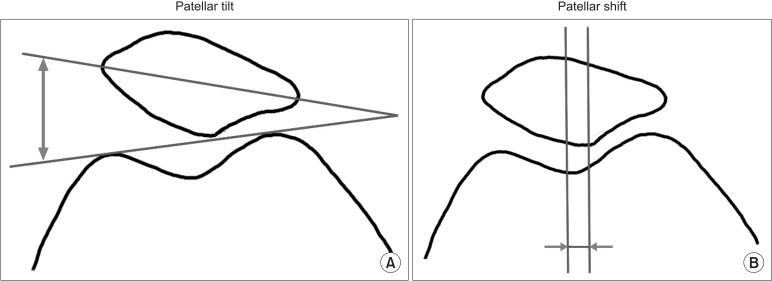
The patellar tilt was measured in the skyline view of the patella by measuring the angle of the line connecting the highest point of the medial and lateral articular surfaces of femoral prostheses (Fig. 2A). This angle is described as (+) if opened medially and as (-) if opened laterally. Lateral tilt was defined as ≥ +5°, and medial tilt as ≤ -5°. Intermediate values were defined as neutral.15) Patellar shift was evaluated by measuring the distance between the vertical line drawn through the center of patella and the vertical line crossing the center of the femoral trochlear surface (Fig. 2B). Displacement was defined as a distance between 5 mm and 10 mm. A shift of ≥ 10 mm was considered subluxation. Dislocation was defined as complete loss of contact with the joint surface.16) Patellofemoral complications such as anterior knee pain, patellar clunk syndrome, symptomatic subluxation, distal pole avulsion fracture, and lateral facet fracture were evaluated during follow-up periods.17,18)
Fig. 2.
Patellar tilt (A) and patella shift (B) were measured from the skyline view.
Statistical Analysis
Potential relationships between anterior knee pain and age, body mass index (BMI), Knee Society knee and function scores, postoperative flexion contracture, the postoperative range of motion, postoperative alignment between the femur and tibia, postoperative patellar tilt, and postoperative patellar displacement at final follow-up and gender were investigated using the Mann-Whitney U-test or Fisher exact test. A p-value of < 0.05 was considered significant.
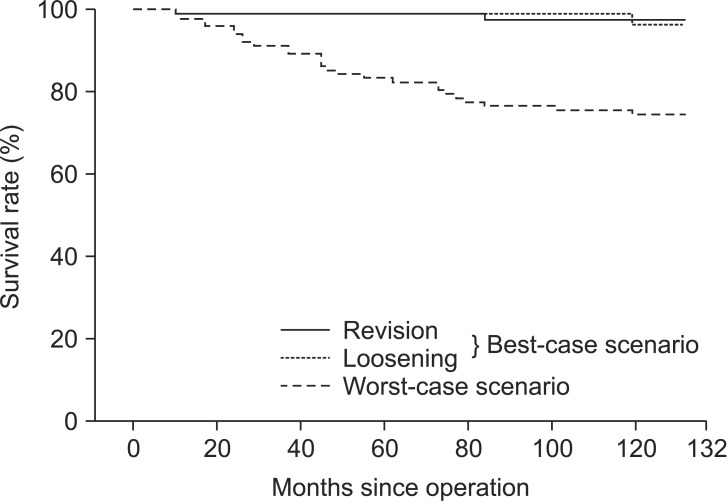
Kaplan-Meier survival analysis with 95% confidence intervals (CIs) was performed on all knees with a minimum 10-year follow-up using radiographic failure, revision or pending revision for any reason as a primary end point.19) We conducted 2 analyses: a best-case scenario (in which all patients lost to follow-up were assumed to have a good outcome); and a worst one assuming that those lost to follow-up were failures. For all analyses we used SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
The mean Knee Society knee score improved from 27.2 points preoperatively (range, 0 to 50 points) to 88.5 points at the final follow-up (range, 45 to 100 points) in the 54 patients (80 knees) with a minimum follow-up of 10 years. Clinical outcomes were classified as excellent or good for 72 (90%), fair for 3, and poor for 4. Mean preoperative function score improved from 35.9 points (range, 0 to 55 points) to 81.6 points (range, 40 to 100 points) at final follow-up. At the time of the most recent follow-up, the mean range of motion after TKA was improved from 113.4° to 124.6° (p < 0.001). Functional outcomes were classified as excellent or good for 66 (82.5%), fair for 8 (10%), and poor for 6 (7.5%). All patients had varus deformity preoperatively when the hip-knee-ankle angle was measured on the long standing radiograph. At the latest postoperative follow-up, 70 knees were in the neutral position, 7 knees had varus angle of < 5° and 3 knees had valgus angle of < 5°.
Anterior knee pain was observed in 6 of the 80 knees (6/54 patients; 7.5%) at final follow-up. However, all 6 patients with patellar pain were able to climb up and down stairs slowly. No significant relation between the anterior knee pain group and no-pain group was found in parameters including age (p = 0.438), gender (p = 0.561), BMI (p = 0.146), preoperative and postoperative Knee Society knee score (p = 0.142, p = 0.103, respectively), preoperative range of motion (p = 0.760), postoperative range of motion (p = 0.664), and all radiographic parameters at final follow-up. However, preoperative (p = 0.023) and postoperative (p = 0.048) Knee Society knee function score was significantly decreased in the anterior knee pain group (Table 2).
Table 2.
Clinical and Radiologic Parameters in Patients with or without Anterior Knee Pain
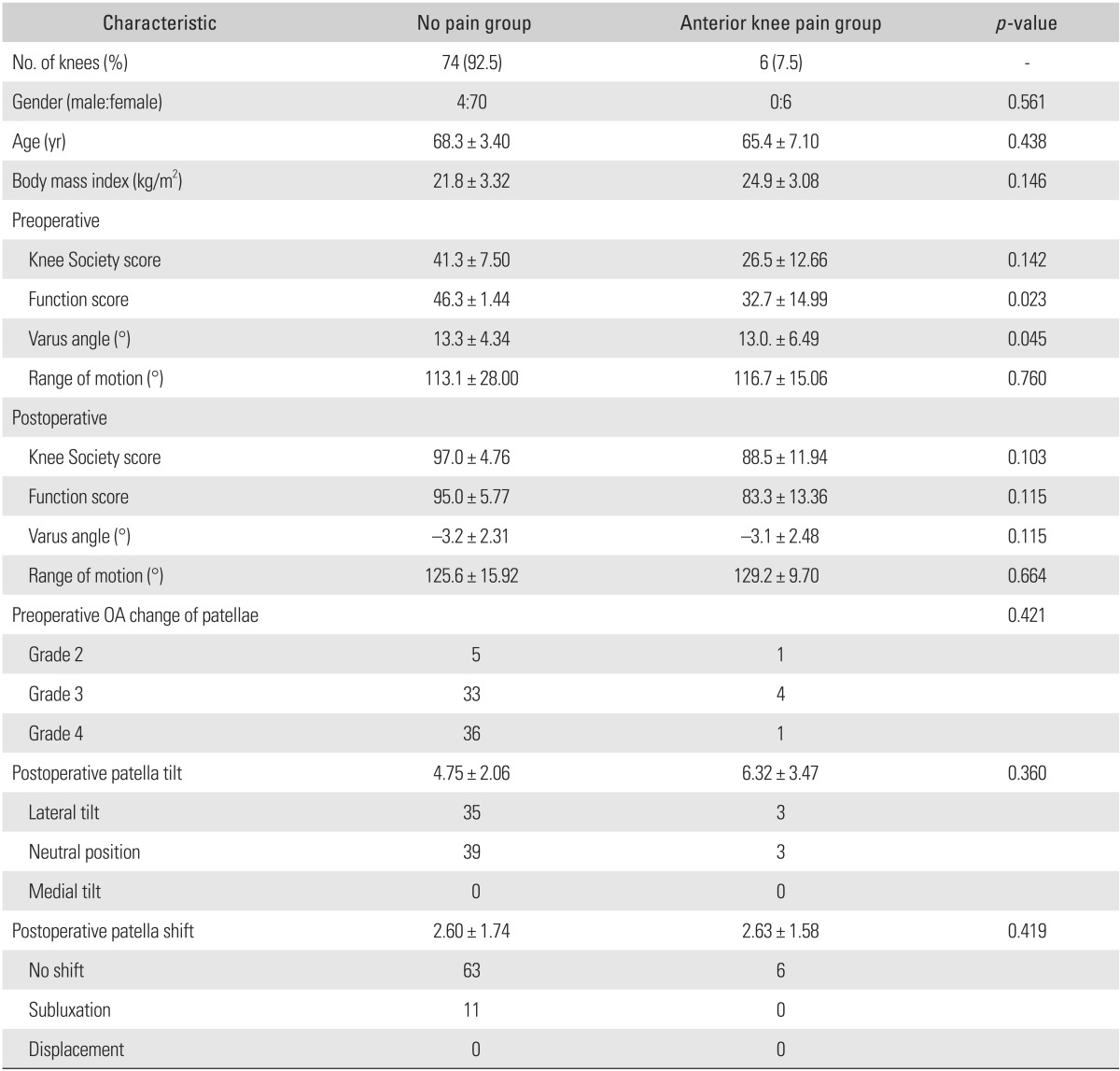
Values are presented as number (%) or mean ± standard deviation.
OA: osteoarthritis.
A non-progressive radiolucent line (a radiographic demarcation of ≥ 2 mm) was observed in 1 femoral (1.2%) and 2 tibial (2.5%) components during serial follow-up. A small osteolytic lesion of the femoral metaphysis was observed in 1 knee, but did not progress on serial radiographs. All femoral components and 78 tibial components were well fixed without loosening at the final follow-up. No obvious tibial insert polyethylene wear was observed. Two tibial components failed due to loosening at 5 years and 7 years, respectively. One of 2 patients underwent revision surgery at 7.5 years after index surgery, but the other patient refused revision surgery for personal reasons at 5.3 years postoperatively
Postoperative complications included 2 knees with periprosthetic fracture and 1 knee with periprosthetic joint infection. Two periprosthetic comminuted fractures of the femoral shaft were sustained at 2 years and 5 years, respectively; 1 patient was treated with a flexible intramedullary nail and the other with a plate and screws. The fractures united uneventfully and femoral components were still well-fixed at the final follow-up. One low-grade infection at 11 months postoperatively was treated by 2-stage reimplantation. In the best-case scenario, survival at 10 years was 96.7% (95% CI, 93.3 to 99.9), and in the worst-case scenario, it was 86.0% (95% CI, 79.2 to 92.8) (Fig. 3).
Fig. 3.
Kaplan-Meier survival rate in the best-case scenario (with implant revision or loosening as endpoints) was 96.7% (95% confidence intervals [CI], 93.3 to 99.9) and in the worst-case scenario was 86.0% (95% CI, 79.2 to 92.8).
DISCUSSION
Single radius TKA was introduced in 1996 to reduce patellofemoral joint complications and to reproduce more physiologic kinematics. To date, excellent mid-term survival outcomes of 95% to 99% were reported for single radius TKA.4,5,6,7,8) However, there are no reports of long-term survivorship and patellofemoral joint complications. To the best of our knowledge, this was the first study to address long-term survivorship of this prosthesis, the prevalence of anterior knee pain for this patella friendly implant, and to determine the relationship between anterior knee pain and specific radiological factors. We found 7.5% of anterior knee pain, no patellofemoral complications, and 96.7% of survivorship at the minimum 10 year follow-up.
Patellofemoral complications are an important type of mechanical failure after TKA, because they can impact functional activities, such as, stair climbing and squatting.18,20) Although the causal factors of patellofemoral complications were multifactorial, the design of the Scorpio knee system such as a single radius femoral component and a deep patella groove to reduce patellofemoral contact stress might be an advantage of patellofemoral problems.6) Kolisek and Barnes8) evaluated anterior knee pain and patellofemoral complications following the Scorpio single radius posterior-stabilized TKA with patellar resurfacing, and experienced 1 patellar fracture in 103 knees. Among the 86 knees included with a minimum follow-up of 4 years, the incidence of anterior knee pain was 5%. No patellofemoral complication, such as dislocation or patellar fracture were observed in our study. Six patients (7.5%) complained of mild anterior knee pain after a minimum follow-up of 10 years. However, we could not find definite mechanical causal factors such as soft tissue impingement, implant malrotation, patellar subluxation, and displacement in these 6 patients. The worse preoperative and postoperative function score in the anterior knee pain group is not causal but consequential. Therefore, it was difficult to explain the reasons of anterior knee pain in this study. Prevalence of anterior knee pain and revision rate in our cohort is similar to that reported by Kolisek and Barnes8) and lower than those in studies using multi-radius total knee system with non-resurfaced patella (Table 3).21,22,23,24,25,26)
Table 3.
Rates of Anterior Knee Pain and Reoperation due to Patellofemoral Complications after TKA Using Multi-Radius Total Knee System with Non-Resurfaced Patella
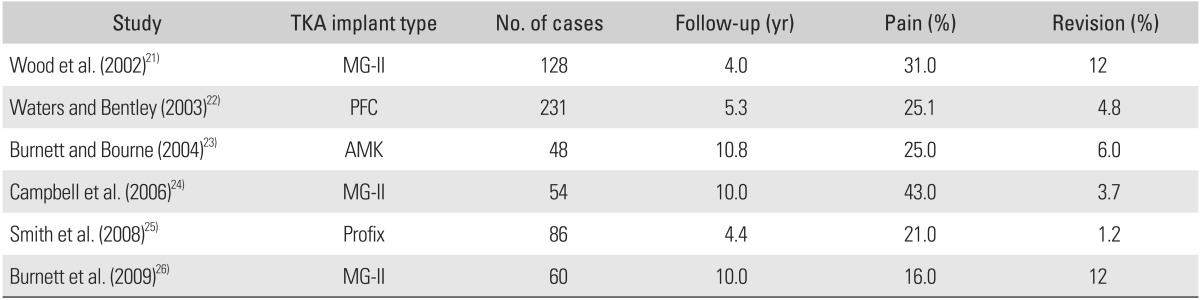
TKA: total knee arthroplasty.
Patellar resurfacing during TKA remains controversial. Recently, Li et al.27) found that overall rates of postoperative anterior knee pain of 12.9% and 24.1% for those that underwent and for those who did not undergo patellar resurfacing, respectively, among a total 1,421 knees. However Garneti et al.28) found rates of anterior knee pain of 25% and 7% in their resurfaced and non-resurfaced groups in 121 patients that underwent Scorpio single radius cruciate retaining TKA. Liu et al.29) reported no advantage of patellar resurfacing. They performed a prospective randomized trial on patellar reshaping versus resurfacing in TKA in 133 patients with a minimum 7 years follow-up, and found rates of anterior knee pain of 12.4% and 14.7% in their reshaping and resurfacing groups, respectively. Although we did not perform patellar resurfacing surgery, the 7.5% rate of anterior knee pain was similar or lower than published data.27,28) Several factors probably contribute to the development of anterior knee pain, but our results suggested differences in cohort characteristics. The current study population was predominantly female, with preoperative varus deformity, and less posttraumatic and rheumatoid arthritis than previously published study populations, which might be a positive protective factor.
Regarding clinical outcomes of single radius total knee prostheses, Abbas and Gunn4) performed 125 posterior-stabilized Scorpio TKAs and only performed 1 revision surgery, in which no aseptic loosening was apparent. The survival rate at 8 years was 99.3%.4) Borrione et al.5) reported the results of a multicenter study that included 602 knees treated with a Scorpio TKA. They performed 18 prosthetic component revisions, which included 10 knees for infection, 6 knees for prosthesis loosening, 1 knee for an oversized tibial component, and 1 knee for painful stiffness. They reported survival rates at 6 years of 95.2% with revision for any reason, and 98.3% with revision for mechanical failure such as aseptic loosening, oversized tibial component, and painful stiffness. In the present study, the survival rate at a minimum follow-up of 10 years was 96.7% with revision surgery for aseptic loosening and infection as the end point, which demonstrated that the cemented single radius posterior-stabilized total knee prosthesis showed excellent radiologic stability during mid- to long-term follow-up.
This result was consistent with the survival rates of other modern design of cemented posterior-stabilized total knee prostheses after long-term follow-up. Rand et al.2) evaluated 11,606 primary TKA at 10 years after index surgery and found that the survival rate was 91%. Rasquinha et al.30) evaluated 105 knees after posterior-stabilized modular knee arthroplasty with a minimum follow-up of 10 years. Revision surgeries were performed in 5 knees because of infection in 2, dislocation in 1, and femoral osteolysis in 2. They reported a 94.6% survival rate after a mean of 12 years with failure for any reason as the end point.
The present study had several notable limitations. First, our cohort was rather small, and of the 71 patients (103 knees) initially considered, 12 (15 knees) died during follow-up and 12 (14 knees) were lost or refused to undergo regular radiologic evaluations. Thus, the analysis was performed on only 78% of eligible patients, which may have influenced our results. Nevertheless, our observed survival rate was comparable with published values. Second, our data has some limits to generalization because the study cohort was very selective with predominantly women and all subjects had preoperative varus deformity. It is known that sores for males and valgus knee result in inferior clinical outcomes. Third, this study had no control group making it impossible to compare the clinical outcome regarding patellofemoral complications; furthermore, we did not evaluate anterior knee pain in this study. Therefore, the study has limited value of the status of anterior knee pain.
In summary, the 96.7% survival rate of Scorpio single radius posterior-stabilized TKA without patellar resurfacing at a minimum follow-up of 10 years, is encouraging. The low rates of implant loosening and 7.5% of anterior knee pain as a patellofemoral complications are comparable with those reported for other current total knee prosthesis.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Archibeck MJ, White RE., Jr What's new in adult reconstructive knee surgery. J Bone Joint Surg Am. 2006;88(7):1677–1686. doi: 10.2106/JBJS.F.00450. [DOI] [PubMed] [Google Scholar]
- 2.Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am. 2003;85-A(2):259–265. doi: 10.2106/00004623-200302000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Callaghan JJ, Rosenberg AG, Rubash HE, Simonian PT, Wickiewicz TL, editors. The adult knee. Philadelphia: Lippincott Williams & Wilkins; 2003. [Google Scholar]
- 4.Abbas D, Gunn RS. Medium-term results of the Scorpio total knee replacement. Knee. 2006;13(4):307–311. doi: 10.1016/j.knee.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Borrione F, Bonnevialle P, Mabit C, et al. Scorpio single radius total knee arthroplasty: a minimal five-year follow-up multicentric study. Int Orthop. 2011;35(12):1777–1782. doi: 10.1007/s00264-011-1226-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.D'Lima DD, Poole C, Chadha H, Hermida JC, Mahar A, Colwell CW., Jr Quadriceps moment arm and quadriceps forces after total knee arthroplasty. Clin Orthop Relat Res. 2001;(392):213–220. doi: 10.1097/00003086-200111000-00026. [DOI] [PubMed] [Google Scholar]
- 7.Gomez-Barrena E, Fernandez-Garcia C, Fernandez-Bravo A, Cutillas-Ruiz R, Bermejo-Fernandez G. Functional performance with a single-radius femoral design total knee arthroplasty. Clin Orthop Relat Res. 2010;468(5):1214–1220. doi: 10.1007/s11999-009-1190-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kolisek FR, Barnes CL. Scorpio posterior-stabilized knee system: 5-year clinical and functional results. J Arthroplasty. 2006;21(8):1187–1192. doi: 10.1016/j.arth.2006.01.020. [DOI] [PubMed] [Google Scholar]
- 9.Mahoney OM, Kinsey TL. 5- to 9-year survivorship of single-radius, posterior-stabilized TKA. Clin Orthop Relat Res. 2008;466(2):436–442. doi: 10.1007/s11999-007-0070-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;(248):13–14. [PubMed] [Google Scholar]
- 11.Insall JN, Hood RW, Flawn LB, Sullivan DJ. The total condylar knee prosthesis in gonarthrosis: a five to nine-year follow-up of the first one hundred consecutive replacements. J Bone Joint Surg Am. 1983;65(5):619–628. [PubMed] [Google Scholar]
- 12.Baldini A, Anderson JA, Zampetti P, Pavlov H, Sculco TP. A new patellofemoral scoring system for total knee arthroplasty. Clin Orthop Relat Res. 2006;452:150–154. doi: 10.1097/01.blo.0000238847.34047.90. [DOI] [PubMed] [Google Scholar]
- 13.Meftah M, Jhurani A, Bhat JA, Ranawat AS, Ranawat CS. The effect of patellar replacement technique on patellofemoral complications and anterior knee pain. J Arthroplasty. 2012;27(6):1075–1080.e1. doi: 10.1016/j.arth.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 14.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752–757. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 15.Grelsamer RP, Bazos AN, Proctor CS. Radiographic analysis of patellar tilt. J Bone Joint Surg Br. 1993;75(5):822–824. doi: 10.1302/0301-620X.75B5.8376449. [DOI] [PubMed] [Google Scholar]
- 16.Keblish PA, Varma AK, Greenwald AS. Patellar resurfacing or retention in total knee arthroplasty: a prospective study of patients with bilateral replacements. J Bone Joint Surg Br. 1994;76(6):930–937. [PubMed] [Google Scholar]
- 17.Harwin SF. Patellofemoral complications in symmetrical total knee arthroplasty. J Arthroplasty. 1998;13(7):753–762. doi: 10.1016/s0883-5403(98)90026-2. [DOI] [PubMed] [Google Scholar]
- 18.Yau WP, Wong JW, Chiu KY, Ng TP, Tang WM. Patellar clunk syndrome after posterior stabilized total knee arthroplasty. J Arthroplasty. 2003;18(8):1023–1028. doi: 10.1016/s0883-5403(03)00447-9. [DOI] [PubMed] [Google Scholar]
- 19.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53(282):457–481. [Google Scholar]
- 20.Ip D, Wu WC, Tsang WL. Comparison of two total knee prostheses on the incidence of patella clunk syndrome. Int Orthop. 2002;26(1):48–51. doi: 10.1007/s00264-001-0316-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wood DJ, Smith AJ, Collopy D, White B, Brankov B, Bulsara MK. Patellar resurfacing in total knee arthroplasty: a prospective, randomized trial. J Bone Joint Surg Am. 2002;84-A(2):187–193. doi: 10.2106/00004623-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty: a prospective, randomized study. J Bone Joint Surg Am. 2003;85-A(2):212–217. doi: 10.2106/00004623-200302000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Burnett RS, Bourne RB. Indications for patellar resurfacing in total knee arthroplasty. Instr Course Lect. 2004;53:167–186. [PubMed] [Google Scholar]
- 24.Campbell DG, Duncan WW, Ashworth M, et al. Patellar resurfacing in total knee replacement: a ten-year randomised prospective trial. J Bone Joint Surg Br. 2006;88(6):734–739. doi: 10.1302/0301-620X.88B6.16822. [DOI] [PubMed] [Google Scholar]
- 25.Smith AJ, Wood DJ, Li MG. Total knee replacement with and without patellar resurfacing: a prospective, randomised trial using the profix total knee system. J Bone Joint Surg Br. 2008;90(1):43–49. doi: 10.1302/0301-620X.90B1.18986. [DOI] [PubMed] [Google Scholar]
- 26.Burnett RS, Boone JL, Rosenzweig SD, Steger-May K, Barrack RL. Patellar resurfacing compared with nonresurfacing in total knee arthroplasty: a concise follow-up of a randomized trial. J Bone Joint Surg Am. 2009;91(11):2562–2567. doi: 10.2106/JBJS.H.00109. [DOI] [PubMed] [Google Scholar]
- 27.Li S, Chen Y, Su W, Zhao J, He S, Luo X. Systematic review of patellar resurfacing in total knee arthroplasty. Int Orthop. 2011;35(3):305–316. doi: 10.1007/s00264-010-1109-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garneti N, Mahadeva D, Khalil A, McLaren CA. Patellar resurfacing versus no resurfacing in Scorpio total knee arthroplasty. J Knee Surg. 2008;21(2):97–100. doi: 10.1055/s-0030-1247802. [DOI] [PubMed] [Google Scholar]
- 29.Liu ZT, Fu PL, Wu HS, Zhu Y. Patellar reshaping versus resurfacing in total knee arthroplasty: results of a randomized prospective trial at a minimum of 7 years' follow-up. Knee. 2012;19(3):198–202. doi: 10.1016/j.knee.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 30.Rasquinha VJ, Ranawat CS, Cervieri CL, Rodriguez JA. The press-fit condylar modular total knee system with a posterior cruciate-substituting design: a concise follow-up of a previous report. J Bone Joint Surg Am. 2006;88(5):1006–1010. doi: 10.2106/JBJS.C.01104. [DOI] [PubMed] [Google Scholar]