Abstract
In Korea, which still lacks a well-established trauma care system, the inability to transport patients to adequate treatment sites in a timely manner is a cause of low trauma patient survival. As such, this study was conducted to serve as a basis for the establishment of a future trauma transport system. We performed a comparative analysis of the transport time, and treatment outcomes between trauma victims transported by ground ambulance (GAMB) and those transported via the helicopter emergency medical service (HEMS) through the National Emergency Management Agency's 119 reporting system, which is similar to the 911 system of the United States, from March 2011 to May 2014. The HEMS-transported patients received treatment instructions, by remote communication, from our trauma specialists from the time of accident reporting; in certain instances, members of the trauma medical staff provided treatment at the scene. A total of 1,626 patients were included in the study; the GAMB and HEMS groups had 1,547 and 79 patients, respectively. The median transport time was different between 2 groups (HEMS, 60 min vs. GAMB, 47 min, P<0.001) but for all patients was 49 min (less than the golden hour). Outcomes were significantly better in the HEMS compared to the GAMB, using the trauma and injury severity score (survival rate, 94.9% vs. 90.5%; Z score, 2.83 vs. -1.96; W score, 6.7 vs. -0.8). A unified 119 service transport system, which includes helicopter transport, and the adoption of a trauma care system that allows active initial involvement of trauma medical personnel, could improve the treatment outcome of trauma patients.
Graphical Abstract
Keywords: Trauma, Transfer, Air Ambulances, Outcome
INTRODUCTION
The timely transport of trauma patients to an appropriate trauma center, known as "getting the right patient to the right place at the right time," is critical in increasing patients' chances of survival (1). As such, the trauma centers that can accommodate the majority of trauma patients and the emergency transport systems that can effectively transport such patients to the center need to be firmly established (2). To respond to this need, the Republic of Korea Government established a plan in 2011 to set up and operate 17 regional trauma centers around the country, and this plan is in the process of being implemented. Although the construction of regional trauma centers and the creation of effective treatment guidelines at the center level should receive due priority, establishing a network of efficient transport to the centers is equally critical. However, challenging circumstances, including the economic pressure under which Korea's complicated medical environment operates, have crippled the plans successful progress. As a result, only 2 regional trauma centers had opened nationwide as of July 2014. In this current atmosphere, a discussion of the transport systems for trauma victims may very well be secondary.
It is widely known that helicopters play an important role in transporting trauma victims. In particular, Korea's geographical characteristics (small land mass, high urban population density, and scattered rural areas in mountainous terrain) render helicopter transport a far more effective option than regular road transport. However, it is not being utilized effectively for reasons of cost and safety. According to the Emergency Medical Annual Report published by the National Emergency Medical Center (3), only 237 patients (0.001%) of a total of 139,072 major medical emergency patients (heart attack, stroke, and major trauma victims) were airlifted by helicopters in 2011. In 2011, the government launched the "Doctor Heli Project" for transporting medical emergency patients using helicopters leased from an airline company. Currently, it is operated by 4 different medical centers, but a nationwide expansion of the service is expected. Furthermore, as the service is not limited to the transportation of trauma victims, additional discussion is needed to facilitate networking with the regional trauma care centers planned for construction around the country.
Despite the current inadequate national helicopter transport performance, our medical center has been operating a trauma victim transport system using firefighting helicopters since March 2011; this has been in connection with the National Emergency Management Agency, local Fire and Disaster Headquarters, and the Aviation Team. The importance of efficient trauma victim transport is gaining recognition, particularly the need for regional trauma centers. The purpose of this study was to review the current trauma patient transport system at our institution and to compare patient outcomes by analyzing data accumulated over the past 3 yr.
MATERIALS AND METHODS
Patient data and transport setting
Study participants were blunt trauma patients who were transported to the emergency room at our center through the 119 emergency system during the period of March 2011-May 2014. The 119 service is an emergency service offered to residences living in the Republic of Korea by National Emergency Management Agency and is similar to the 911 system of the United States. In emergency events, such as road traffic accidents, fires and disasters, 119 service centers take the emergency calls and dispatch fire fighters and/or emergency medical technicians to the scene. Upon a victim or witness placing a 119 call, the Fire and Disaster Headquarters identifies the severity of the injury using the Field Triage Decision Scheme and determines whether to dispatch either a ground ambulance (GAMB) or the helicopter emergency medical service (HEMS). If the HEMS is deemed necessary, the trauma specialists of our hospital are immediately notified via a hotline. If it is decided that medical staff should be dispatched, the helicopter is sent from the local Fire and Disaster Headquaters/Aviation Team to the medical center in order to pick up the medical staff on duty (1-2 trauma surgeons and 1 trauma nurse), who will provide medical care on the scene and en route to the medical center. In the meantime, the remaining medical staff at the center make the necessary preparations for immediate medical tests and surgical treatment upon the patient's arrival.
This study was conducted using data from patients with blunt trauma. We excluded patients with penetrating trauma or unknown mechanisms of injury, patients transferred from other hospitals, deaths on arrival, victims for whom resuscitation was initiated on arrival but failed, and patients whose trauma and injury severity score (TRISS) (4) could not be calculated owing to insufficient data. Study participants were categorized into 2 groups depending on whether the mode of transport to the center was by GAMB (GAMB group) or by helicopter (HEMS group). The patient demographics, transport time, cause of injury, and Injury Severity Score (ISS) were compared between the GAMB and HEMS groups. The probability of survival (Ps) was calculated using the TRISS to compare the treatment outcomes of both groups with those of the major trauma outcome study (MTOS) (5).
Study instruments
The TRISS is a method of predicting the prognosis of trauma patients (4); it has become an internationally accepted tool for determining the impact of the HEMS on trauma mortality (6, 7, 8, 9, 10, 11). It combines a physiological scoring system, the revised trauma score (RTS) (12, 13), and the ISS. The MTOS (5, 14) is a study in which the TRISS, age, and mechanism of injury were used to calculate survival norms, using regression analysis, of 80,000 trauma patients in 139 North American hospitals. The norms were updated in 1990 (14). Patients with a Ps of 0.5 or less are expected to die and those with a Ps greater than 0.5 are expected to survive (10). The MTOS cohort has been widely used as a benchmark for comparing outcomes in trauma patients using the TRISS methodology. These data can be used to identify unexpected outcomes in both populations and individual patients.
Statistical analysis
We used SPSS version 19 (IBM corporation) for all statistical analyses. Continuous data are summarized by the median and interquartile range (IQR), unless otherwise specified. We compared patient demographics, ISS, and transport time using the Mann-Whitney U test or chi-square analysis, as appropriate. Comparisons between predicted and observed patient mortality were made using the Z, W, and M statistics (4). The Flora Z statistic estimates the deviation of mortality in the study group compared to the MTOS benchmark (4). The W statistic calculates the number of survivors more or less than the MTOS norm per 100 patients analyzed (15) and provides a clinical perspective for a statistically significant Z score (13). The M statistic evaluates the similarity of injury severity between the study group and the entire MTOS cohort (4).
Ethics statement
This study was approved by the institutional review board (IRB) of Ajou University Hospital (IRB No. MED-MDB-14-250). The requirement for informed consent was waived by the IRB because of the observational nature of this study.
RESULTS
During the study period, 1,626 patients met the inclusion criteria and were included in the analysis. Of these, 49% were victims of traffic accidents, which were the most common source of injury (Table 1). The median age was 47 yr (IQR, 31-61 yr) and 1,102 (67.8%) of the patients were male. There were 1,547 patients who were transported by GAMB (GAMB group) and 79 who were transported by helicopter (HEMS group). The transport mode of all of the HEMS group patients was determined via hotline communication between the Fire and Disaster Headquarters and the trauma specialists at the center. Critical care was provided at the scene of the injury and en route to the center through online instructions. Of the 79 patients in the HEMS group, 19 (24.1%) received critical care directly from medical staff dispatched to the field.
Table 1.
Blunt trauma injury mechanisms of 1,626 patients enrolled in the study
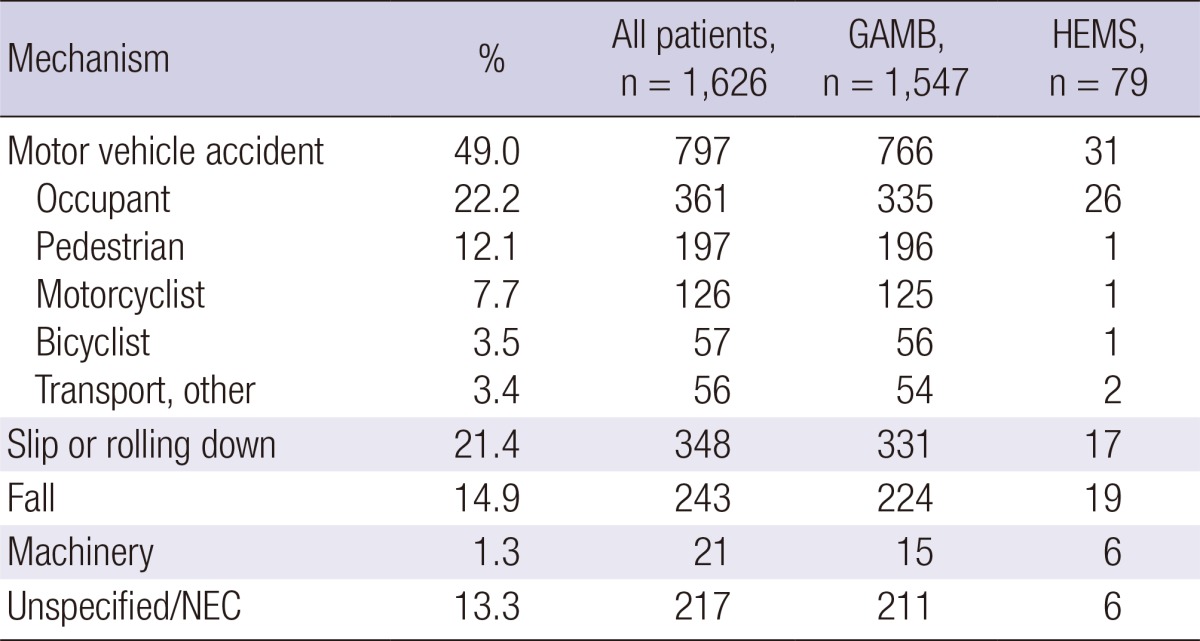
GAMB, ground ambulance; HEMS, helicopter emergency medical service; NEC, not elsewhere classifiable.
Table 2 displays the baseline characteristics of the GAMB and HEMS groups with respect to age, gender, ISS, and transport time. The HEMS group had a significantly higher proportion of men (78.5% vs. 67.2%) and a significantly longer median transport time (60 min vs. 47 min) than the GAMB group.
Table 2.
Baseline characteristics of the study population
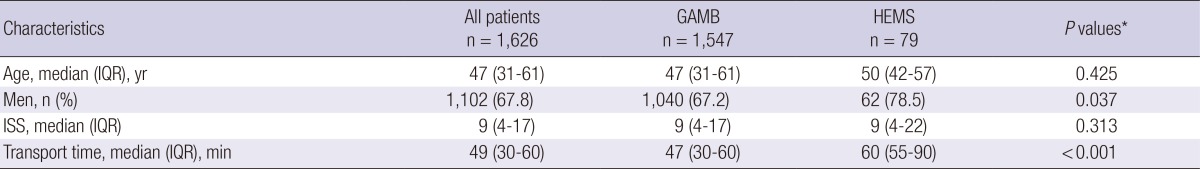
*We compared data between GAMB and HEMS using the Mann-Whitney U test or chi-square analysis, as appropriate. GAMB, ground ambulance; HEMS, helicopter emergency medical service; IQR, interquartile range; ISS, injury severity score.
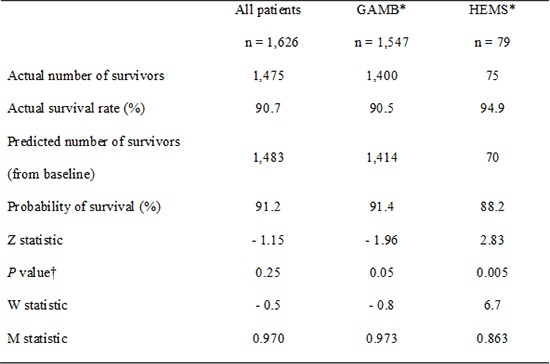
The Ps for study participants was determined using the TRISS method. The Z, W, and M statistics were calculated and compared with the MTOS norms (Table 3). The results of this analysis indicate that, overall, the Ps for patients in this study was slightly lower than that of the MTOS baseline (90.7% and 91.2%, respectively). Based on the W-score, it appears that 0.5 more patients died per 100 transports, but this difference was not statistically significant (Z statistic=-1.15, P=0.25). The M score for all patients was 0.970, matched with the MTOS baseline Ps increment (Table 4).
Table 3.
Comparison of survival between GAMB and HEMS groups and the MTOS using Z, W, and M statistics
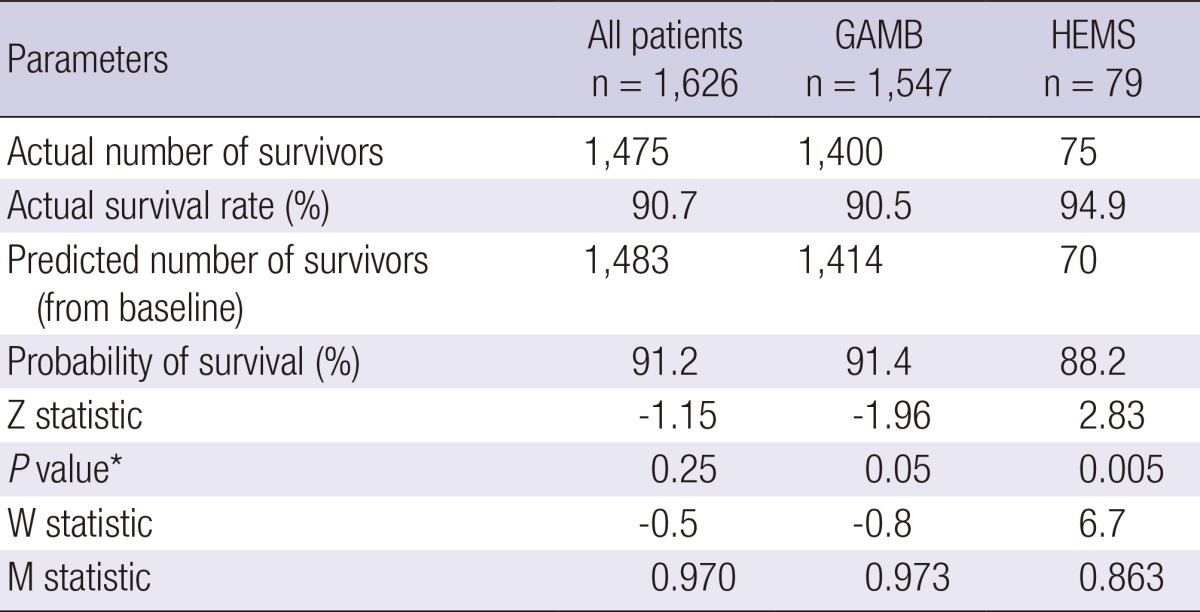
*The significance level for values of Z. MTOS, major trauma outcome study; GAMB, ground ambulance; HEMS, helicopter emergency medical service.
Table 4.
Comparison of survival probabilities of the Major Trauma Outcome Study cohort and our study population
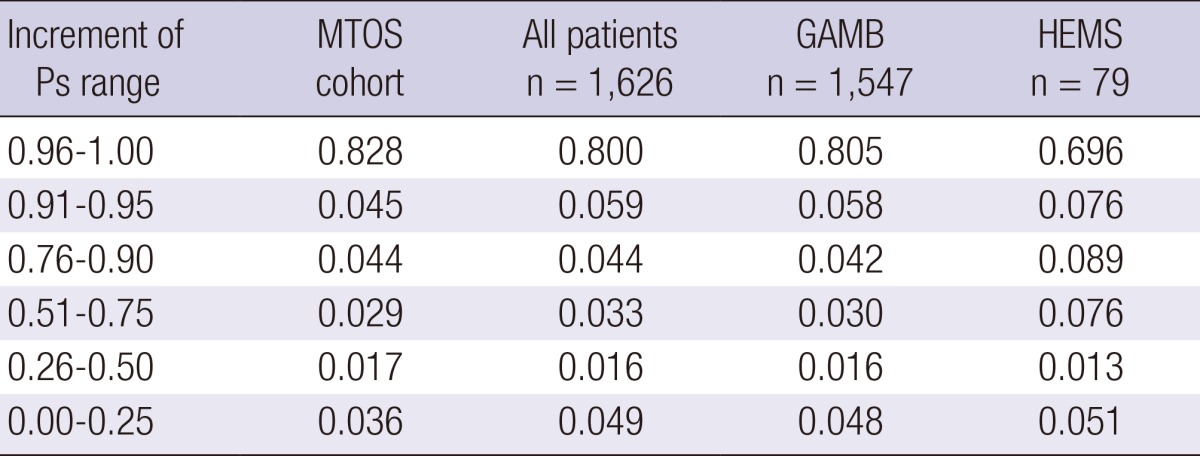
Ps, survival probability; MTOS, major trauma outcome study; GAMB, ground ambulance; HEMS, helicopter emergency medical service.
The Z, M, and W statistics were also compared for patients in the GAMB and HEMS groups (Table 3). In both groups, the outcomes were significantly different from the MTOS norms. The survival rate in the GAMB group was 90.5%, significantly lower than the MTOS norm (MTOS 91.4%; Z statistic=-1.96, P=0.05). When expressed using the W score, there were 0.8 more deaths per 100 transports. The M score in the GAMB group (0.973) was very similar to the MTOS baseline Ps increment (Table 4). In the HEMS group, the survival rate was 94.9%, which was statistically significantly different from that in the MTOS group (81.2%; Z statistic=2.83, P=0.005). When expressed as a W score, there were 6.7 more survivals per 100 transports. However, the M score of this group was 0.863, which was lower than the MTOS baseline Ps increment (Tables 3 and 4).
To summarize, blunt trauma victims who were transported directly to the center through the 119 system, and who arrived within an hour of the accident, had treatment outcomes similar to that of the MTOS norms. However, when the patients were divided into 2 groups by transport mode, the GAMB group had a shorter transport time (median 47 min vs. 60 min), but poorer outcomes (survival rate 90.5% vs. 94.9%; Z score -1.96 vs. 2.83; W score -0.8 vs. 6.7) than the HEMS group.
DISCUSSION
Timely transport and medical care within the golden hour is well known to increase trauma victims' chances of survival. However, an effective trauma care system in Korea has not yet been firmly established, and most trauma patients are transported to the nearest local hospital, as opposed to a trauma center. As a result, these patients fail to receive critical trauma care during the golden hour (16). In response to this need, 17 specialized trauma centers have been established around the country since 2011, to which trauma patients can be directly transported from the scene of an accident to receive specialized trauma care within the critical period. However, it might be a while before such a system becomes widely used because of a number of obstacles.
One of the many issues is the lack of a streamlined transport system from the scene of an accident to a trauma center. Currently, the nation's emergency medical care system lacks appropriate transport protocols, such that trauma patients are regularly transported to the nearest local hospital, a problem that has been pointed out several times (16, 17, 18, 19). Although fire department ambulances are most commonly used in the transport of trauma patients, a significant number of private ambulance transport services and other modes of transportation are also used, in which case no medical staff or intervention is provided until arrival at the nearest local hospital. Furthermore, necessary critical care for trauma patients, such as tracheal intubation and intravenous fluid maneuvers, are delayed. In our study, to minimize the potential confounding factors associated with transport time and transport processes, study participants were limited to blunt trauma victims who were transported to the center through the 119 system. These comprised 1,626 patients during the study period of 38 months. During this period of time, approximately 1,200 trauma patients were transported without use of the 119 system, indicating that about two-thirds of trauma patients in need of transport use the 119 system.
In our study population, the median transport time for all trauma patients appeared to be within 1 hr of the accident. Such findings show that transporting trauma patients from the scene of an accident to a final trauma center through the 119 system is currently a viable option for facilitating medical care within the golden hour. The median transport time in the GAMB group was 47 min, 13 min shorter than that observed in the HEMS group. This is similar to the median transport time of 40 min observed during similar research conducted by the center in 2011 (16). The transport time by helicopter was longer than ground transport time and this corresponded with the results of previous studies (20, 21, 22). The longer median transport time in the HEMS group (60 min) may be attributable to the time required to prepare for helicopter takeoff and landing (e.g., loading and scoping for the landing site). In addition, of the 79 patients in the HEMS group, medical staff boarded the craft to provide critical care on-site in 19 cases; this may have contributed to the longer transport time compared to the GAMB group. Another possible reason for this is distance from the scene to hospital. In general, helicopter transport is requested for the patient in a longer distance travel such as from rural or mountain area. On the other hand, ground transport would be used for the patient in urban area, which is relatively short distance to the hospital. To get a firm evidence for this, regional distribution was investigated, which was not successful due to the lack of supporting data. Nevertheless, the median transport time of both groups fell within the golden hour range, indicating that trauma victim transport was effective. Despite the longer median transport time, the HEMS group exhibited better treatment outcomes, which can be attributed to the immediate professional medical attention made available through the hotline, beginning at the point of accident reporting.
In order to effectively compare the treatment outcomes of trauma victims, the patients' injury severity needs to be quantified. The most commonly used measure is the ISS, based on the Abbreviated Injury Scale (23) introduced in 1971, which is known to correlate well with the mortality rate (24, 25). However, the ISS is an anatomical scoring system, which is limited owing to the exclusion of physiological predictors. The RTS, developed in 1989, uses physiological data, including systolic blood pressure, respiratory rate, and the Glasgow Coma Scale (12, 13). Despite the rather complex computation process, the RTS helped to establish the TRISS system, and it complements the ISS (4). The TRISS also has limitations, but it is currently accepted as the most effective measure for evaluating trauma outcome (26). In particular, it is the most widely used measure for comparing outcomes for the evaluation of the transport process, including the medical treatment provided en route (10, 11, 15, 20, 27, 28, 29, 30, 31, 32). Currently, however, research on emergency helicopter transport is lacking in Korea, and TRISS-based outcome analysis of helicopter-transported trauma patients is yet to be conducted.
Results of the TRISS analysis in this study matched the MTOS norms, indicating that a comparison of the GAMB and HEMS groups is warranted. Using the Z and W statistics suggested by the MTOS, we found that, although the Ps M score for the HEMS group was 0.88 or less, the treatment outcomes for all patients was not greatly different from the MTOS norm. When we compared the HEMS and GAMB groups, the HEMS group exhibited positive treatment outcomes whereas the GAMB group did not. In the study that introduced the TRISS method, Boyd et al. (4) stated that values of M<0.88 indicate a disparity in the injury severity between groups. The Z values associated with lower M values (<0.88) should be viewed with some skepticism. The low M value does not explain whether the study group was more or less severely injured than the baseline population. Therefore, the statistical significance of the HEMS group Z and W scores in the present study should not be taken at face value; some discretion is warranted. However, on considering the distribution and range of the Ps of all subjects (Table 4), the HEMS group Ps distribution did tend to be towards the lower end of the range; from this, it can be inferred that the patients with lower Ps, that is, with a greater severity of injury, displayed superior treatment outcomes. Although other variables may need to be considered, it can be presumed that the difference in outcome between the groups is due to the transport mode used. Transport mode was the only variable factor in this study, considering that all study subjects were transported to the center through the 119 system and received the same level of treatment by the same medical staff who followed the same protocol. In other words, the treatment outcome of patients that were transported within the golden hour, without stopping at another hospital, corresponds with the standards in the United States from 1980 to 1990, which established its trauma system prior to Korea (the MTOS was announced in 1990). However, our results suggest that when medical personnel became involved in treatment more expeditiously and aggressively, as is the case with the use of a helicopter, improved survival of up to 6.7 more patients for every 100 transports can be achieved.
The first major comparison of outcomes following air transport of trauma patients was published by Baxt and Moody (10) in 1983 and showed that air transport contributed to a 53% reduction in the death rate. Since then, numerous studies have been published on the benefits of medical emergency helicopter transport. According to a recent multicenter trial by Thomas et al. in 2002 (33), patients transported by helicopters exhibit up to a 24% reduction in mortality rate when controlling for severity of injury and medical center factors. A study by Biewener et al. (21) in 2004 showed a 50% reduction in the mortality rate when patients were transported to a trauma center by helicopter, as opposed to transfer to a regular medical center via GAMB. In 2007, Mitchell et al. (34) conducted a 5-yr TRISS analysis on a Canadian cohort of blunt trauma patients with an ISS above 12. In that study, patients transported by helicopter had a W score of 6.4. In Japan, the Doctor-Heli system has been used since 2000 for transporting severe trauma patients when the lead-time is expected to be 30 min or longer. Of the 2,888 trauma patients transported through the system in 2003, 168 patients (10%) were reported to have been transported directly to a trauma center from the scene, which resulted in an increased survival rate and decreased disability rate (35). Despite the relatively small sample size in comparison with the aforementioned research, our TRISS analysis in this study also demonstrates the effectiveness of helicopter transport. We observed a survival rate of 94.9%, which is significantly greater than the predicted survival rate of 88.2%. When expressed as a W score, we found that 6.7 more lives were saved per 100 transports, compared to the MTOS norm.
Other researchers have not found improved outcomes for helicopter-transported patients, and some have argued that the injuries suffered by these patients were not severe. Schiller et al. (36) in 1988, reported no difference in outcomes between blunt trauma patients transported by GAMB or by helicopter. Cunningham et al. (37) in 1997, reported advantages in helicopter transport, based on the ISS and trauma score, although they concluded that helicopter transport alone could not be used as a predictor of survival. Other researchers have reported that the majority of patients transported by helicopter suffer from minor injuries, resulting in overtriage. A meta-analysis conducted by Bledsoe et al. (38) showed that 1 out of 4 patients are discharged from the medical center within 24 hr, and 60%-70% of patients have non-life-threatening trauma injuries. Most of these studies were conducted in an urban setting, with generally more advanced treatment systems and shorter transport times than in rural areas, which may have had an effect on the results. In this urban medical center study, we found that the median transport time in the GAMB group was 47 min, shorter than the median time of 60 min in the HEMS group. While accident site and transport distance should be controlled for in the analysis, the HEMS group (n=79) had relatively few participants than the GAMB group (n=1,547), which prohibited a uniform comparison. Furthermore, the study was limited by inaccurate accident location data in the GAMB group. We estimate that, in general, GAMB group patients were transported from within the city limits, whereas many of the HEMS group patients were transported from mountainous or rural areas. A follow-up study is planned once helicopter transport cases accumulate over time, and it will include stringently collected medical record data to obtain accurate accident location and transport distance data. In this study, we attempted to compare transport distances by comparing non-distinguishable median values, without differentiation according to transport distance, which limits the interpretation of our results.
Recently, a large-scale study reported that helicopter transport of severe trauma victims was associated with a higher survival rate than that of patients transported by GAMB (39). This study included only the patients transported directly from the scene to our center, and thus the median ISS was not high. In other studies, which also included transport between facilities (40), 58.9% of the patients in the HEMS group exhibited scores of 15 and above. In particular, a high mean ISS of 25 was observed when medical staff were present in the aircraft. These data indicate that overtriage issues can be resolved at the scene with improved patient selection and classification. Currently, the country has 26 firefighting helicopters equipped with emergency medical service (EMS) capacity (http://www.prism.go.kr/homepage/researchCommon/retrieveResearchDetailPopup.do;jsessionid=F44FE4793B773F712B3725A35692BB65.node02?research_id=1351000-201100053). However, considering their low usage rate, a discussion of the costs associated with helicopter transport seems to be premature. Nevertheless, an effective transport network utilizing the 26 EMS firefighting helicopters in connection with the regional trauma centers will clearly contribute to improved survival rates.
Our medical center transported a total of 191 trauma victims by helicopters between March 2011 and May 2014. Of these patients, 79 blunt trauma victims directly transported from the scene were included in this study; interfacility transported and penetration wound patients were excluded, which made the proportion of helicopter transported patients appear extremely low in comparison with other countries. However, a statistically higher survival rate than the MTOS norm was observed in our TRISS-based analysis. Our data indicate that establishing a streamlined medical emergency transport system centered on the 119 system, which already has the capacity for an integrated transport system, including helicopters, will effectively increase the chances of survival for trauma victims, especially considering the currently limited national resources. A system in which medical staff specialized in trauma care are actively involved, from classifying patients to providing critical care, appears to be a necessity because Korean EMS providers are not as qualified as those in other countries to provide adequate critical care. Therefore, an effective medical emergency transport network that utilizes the 119 reporting system needs to be established, in which trauma victims will be effectively and accurately identified and classified at the scene, and transported directly to the trauma centers currently under construction. If arrival within the golden hour is not expected or in cases of severe trauma patients, every effort should be made for efficient transport and successful resuscitation, with active involvement of the medical staff on board.
Footnotes
The authors have no conflicts of interest to disclose.
Conception and coordination of the study: Kim J, Heo Y, Lee JC, Jung K. Acquisition of data: Kim J, Baek S, Moon J, Youn SH, Jung K. Data review and interpretation of results: Kim J, Heo Y, Lee JC, Jung K. Statistical analysis: Kim J, Baek S, Jung K. Critical review and editing: Heo Y, Lee JC, Wang H. Manuscript preparation: Kim J, Baek S, Kim Y, Moon J, Youn SH, Huh Y, Jung K. Manuscript approval: all authors.
References
- 1.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 2.Kim Y. Preliminary study on the establishment of regional trauma center and an operation model in Korea. [accessed on 28 February 2011]. Available at http://www.prism.go.kr/homepage/researchCommon/retrieveResearchDetailPopup.do;jsessionid=111A8C834E2F00398316B1462BC82F2F.node02?research_id=1351000-201100048.
- 3.National Emergency Medical Center. Emergency Medical Service Annual Report. 2012. [accessed on 2 September 2013]. Available at http://www.nemc.or.kr/egen/inf.emb13.do.
- 4.Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the TRISS method. Trauma Score and the Injury Severity Score. J Trauma. 1987;27:370–378. [PubMed] [Google Scholar]
- 5.Champion HR, Copes WS, Sacco WJ, Lawnick MM, Keast SL, Bain LW, Jr, Flanagan ME, Frey CF. The Major Trauma Outcome Study: establishing national norms for trauma care. J Trauma. 1990;30:1356–1365. [PubMed] [Google Scholar]
- 6.Baxt WG, Moody P. The impact of a physician as part of the aeromedical prehospital team in patients with blunt trauma. JAMA. 1987;257:3246–3250. [PubMed] [Google Scholar]
- 7.Hamman BL, Cué JI, Miller FB, O'Brien DA, House T, Polk HC, Jr, Richardson JD. Helicopter transport of trauma victims: does a physician make a difference? J Trauma. 1991;31:490–494. doi: 10.1097/00005373-199104000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Burney RE, Passini L, Hubert D, Maio R. Comparison of aeromedical crew performance by patient severity and outcome. Ann Emerg Med. 1992;21:375–378. doi: 10.1016/s0196-0644(05)82653-8. [DOI] [PubMed] [Google Scholar]
- 9.Schmidt U, Frame SB, Nerlich ML, Rowe DW, Enderson BL, Maull KI, Tscherne H. On-scene helicopter transport of patients with multiple injuries--comparison of a German and an American system. J Trauma. 1992;33:548–553. doi: 10.1097/00005373-199210000-00010. discussion 53-5. [DOI] [PubMed] [Google Scholar]
- 10.Baxt WG, Moody P. The impact of a rotorcraft aeromedical emergency care service on trauma mortality. JAMA. 1983;249:3047–3051. [PubMed] [Google Scholar]
- 11.Bartolacci RA, Munford BJ, Lee A, McDougall PA. Air medical scene response to blunt trauma: effect on early survival. Med J Aust. 1998;169:612–616. doi: 10.5694/j.1326-5377.1998.tb123435.x. [DOI] [PubMed] [Google Scholar]
- 12.Champion HR, Sacco WJ, Carnazzo AJ, Copes W, Fouty WJ. Trauma score. Crit Care Med. 1981;9:672–676. doi: 10.1097/00003246-198109000-00015. [DOI] [PubMed] [Google Scholar]
- 13.Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A revision of the Trauma Score. J Trauma. 1989;29:623–629. doi: 10.1097/00005373-198905000-00017. [DOI] [PubMed] [Google Scholar]
- 14.Champion HR, Sacco WJ, Copes WS. Injury severity scoring again. J Trauma. 1995;38:94–95. doi: 10.1097/00005373-199501000-00024. [DOI] [PubMed] [Google Scholar]
- 15.Younge PA, Coats TJ, Gurney D, Kirk CJ. Interpretation of the Ws statistic: application to an integrated trauma system. J Trauma. 1997;43:511–515. doi: 10.1097/00005373-199709000-00021. [DOI] [PubMed] [Google Scholar]
- 16.Jung KW, Jang JM, Kim J, Baek SJ, Song SY, Gang CS, Lee KJ. Delayed transfer of major trauma patients under the current emergency medical system in Korea. J Korean Soc Traumatol. 2011;24:25–30. [Google Scholar]
- 17.Han SS, Jung K, Kwon J, Kim J, Choi SC, Lee KJ. Problems with transferring major trauma patients to emergency medical center of a university hospital from another medical center. J Korean Soc Traumatol. 2011;24:118–124. [Google Scholar]
- 18.Jung KY, Kim JS, Kim Y. Problems in trauma care and preventable deaths. J Korean Soc Emerg Med. 2001;12:45–56. [Google Scholar]
- 19.Kim Y, Jung KY, Cho KH, Kim H, Ahn HC, Oh SH, Lee JB, Yu SJ, Lee DI, Im TH, et al. Preventable trauma deaths rates and management errors in emergency medical system in Korea. J Korean Soc Emerg Med. 2006;17:385–394. [Google Scholar]
- 20.Baxt WG, Moody P, Cleveland HC, Fischer RP, Kyes FN, Leicht MJ, Rouch F, Wiest P. Hospital-based rotorcraft aeromedical emergency care services and trauma mortality: a multicenter study. Ann Emerg Med. 1985;14:859–864. doi: 10.1016/s0196-0644(85)80634-x. [DOI] [PubMed] [Google Scholar]
- 21.Biewener A, Aschenbrenner U, Rammelt S, Grass R, Zwipp H. Impact of helicopter transport and hospital level on mortality of polytrauma patients. J Trauma. 2004;56:94–98. doi: 10.1097/01.TA.0000061883.92194.50. [DOI] [PubMed] [Google Scholar]
- 22.Phillips RT, Conaway C, Mullarkey D, Owen JL. One year's trauma mortality experience at Brooke Army Medical Center: is aeromedical transportation of trauma patients necessary? Mil Med. 1999;164:361–365. [PubMed] [Google Scholar]
- 23.Rating the severity of tissue damage. I. The abbreviated scale. JAMA. 1971;215:277–280. doi: 10.1001/jama.1971.03180150059012. [DOI] [PubMed] [Google Scholar]
- 24.Becher RD, Meredith JW, Kilgo PD. Injury severity scoring and outcomes research. In: Mattox KL, Moore EE, Feliciano DV, editors. Trauma. 7th ed. New York: McGraw-Hill; 2013. [Google Scholar]
- 25.Baker SP, O'Neill B, Haddon W, Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 26.Glance LG, Osler TM, Dick AW. Evaluating trauma center quality: does the choice of the severity-adjustment model make a difference? J Trauma. 2005;58:1265–1271. doi: 10.1097/01.ta.0000169429.58786.c6. [DOI] [PubMed] [Google Scholar]
- 27.Cameron PA, Flett K, Kaan E, Atkin C, Dziukas L. Helicopter retrieval of primary trauma patients by a paramedic helicopter service. Aust N Z J Surg. 1993;63:790–797. doi: 10.1111/j.1445-2197.1993.tb00342.x. [DOI] [PubMed] [Google Scholar]
- 28.Jacobs LM, Gabram SG, Sztajnkrycer MD, Robinson KJ, Libby MC. Helicopter air medical transport: ten-year outcomes for trauma patients in a New England program. Conn Med. 1999;63:677–682. [PubMed] [Google Scholar]
- 29.Buntman AJ, Yeomans KA. The effect of air medical transport on survival after trauma in Johannesburg, South Africa. S Afr Med J. 2002;92:807–811. [PubMed] [Google Scholar]
- 30.Schwartz RJ, Jacobs LM, Juda RJ. A comparison of ground paramedics and aeromedical treatment of severe blunt trauma patients. Conn Med. 1990;54:660–662. [PubMed] [Google Scholar]
- 31.Schwartz RJ, Jacobs LM, Yaezel D. Impact of pre-trauma center care on length of stay and hospital charges. J Trauma. 1989;29:1611–1615. doi: 10.1097/00005373-198912000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Butler DP, Anwar I, Willett K. Is it the H or the EMS in HEMS that has an impact on trauma patient mortality? A systematic review of the evidence. Emerg Med J. 2010;27:692–701. doi: 10.1136/emj.2009.087486. [DOI] [PubMed] [Google Scholar]
- 33.Thomas SH, Harrison TH, Buras WR, Ahmed W, Cheema F, Wedel SK. Helicopter transport and blunt trauma mortality: a multicenter trial. J Trauma. 2002;52:136–145. doi: 10.1097/00005373-200201000-00023. [DOI] [PubMed] [Google Scholar]
- 34.Mitchell AD, Tallon JM, Sealy B. Air versus ground transport of major trauma patients to a tertiary trauma centre: a province-wide comparison using TRISS analysis. Can J Surg. 2007;50:129–133. [PMC free article] [PubMed] [Google Scholar]
- 35.Mashiko K. Trauma systems in Japan: history, present status and future perspectives. J Nippon Med Sch. 2005;72:194–202. doi: 10.1272/jnms.72.194. [DOI] [PubMed] [Google Scholar]
- 36.Schiller WR, Knox R, Zinnecker H, Jeevanandam M, Sayre M, Burke J, Young DH. Effect of helicopter transport of trauma victims on survival in an urban trauma center. J Trauma. 1988;28:1127–1134. doi: 10.1097/00005373-198808000-00004. [DOI] [PubMed] [Google Scholar]
- 37.Cunningham P, Rutledge R, Baker CC, Clancy TV. A comparison of the association of helicopter and ground ambulance transport with the outcome of injury in trauma patients transported from the scene. J Trauma. 1997;43:940–946. doi: 10.1097/00005373-199712000-00013. [DOI] [PubMed] [Google Scholar]
- 38.Bledsoe BE, Wesley AK, Eckstein M, Dunn TM, O'Keefe MF. Helicopter scene transport of trauma patients with nonlife-threatening injuries: a meta-analysis. J Trauma. 2006;60:1257–1265. doi: 10.1097/01.ta.0000196489.19928.c0. [DOI] [PubMed] [Google Scholar]
- 39.Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML. Helicopters and the civilian trauma system: national utilization patterns demonstrate improved outcomes after traumatic injury. J Trauma. 2010;69:1030–1034. doi: 10.1097/TA.0b013e3181f6f450. [DOI] [PubMed] [Google Scholar]
- 40.Moon J, Kim J, Jung K, Kim YH, Youn SH, Kim E, Heo Y, Lee CJ. Helicopter emergency medical services for trauma patient transport: a single center experience and literature review. J Acute Care Surg. 2014;4:24–27. [Google Scholar]


