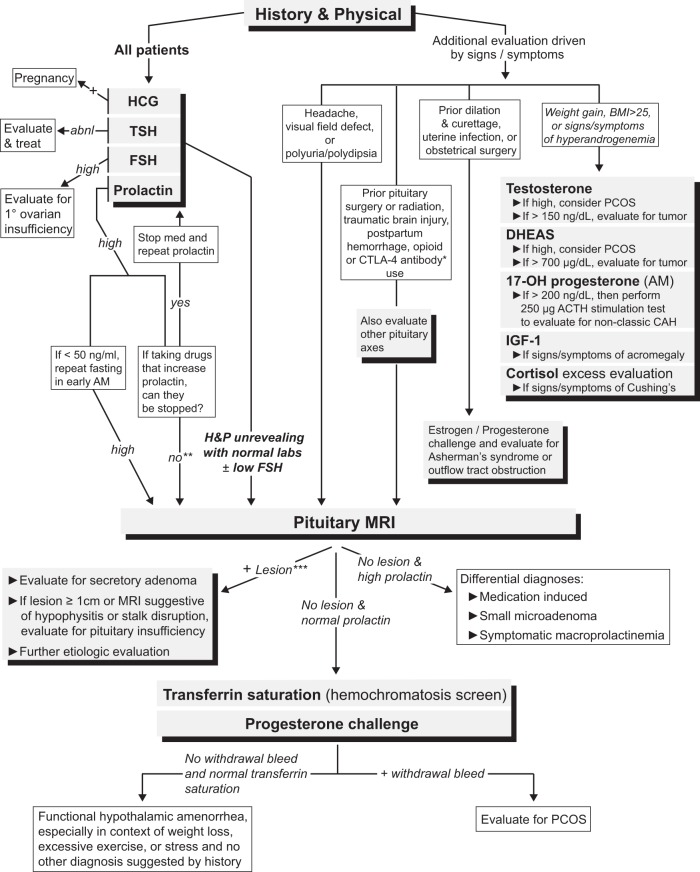
Figure 3.
A suggested diagnostic algorithm for evaluating patients with secondary amenorrhea, including non-neuroendocrine causes. Importantly, all patients presenting with secondary amenorrhea should have a history and physical examination performed and a basic laboratory evaluation consisting of serum human chorionic gonadotropin, TSH, FSH, and prolactin levels. *, Individuals who have been prescribed CTLA-4 antibody therapies (ipilimumab or tremelimumab) should have an MRI with pituitary cuts to evaluate for hypophysitis. **, Unless the cause of the hyperprolactinemia can be definitively attributed to the medication (for example, by stopping the medication and repeating the prolactin level), it is difficult to exclude the possibility of a prolactinoma or stalk disruption (due to a sellar lesion) causing the hyperprolactinemia. ***, If the lesion is small (<1 cm) and is found to be nonsecretory, we would recommend following the “No lesion and normal prolactin” pathway because this lesion is unlikely to be the cause of the amenorrhea. Abbreviations: abnl, abnormal; BMI, body mass index; DHEAS, dehydroepiandrosterone sulfate; PCOS, polycystic ovary syndrome; 17-OH progesterone, 17-hydroxyprogesterone; H&P, history and physical.