Figure 1.
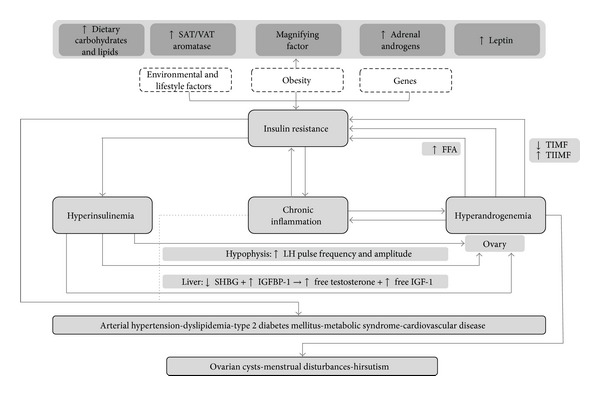
Interactions among insulin resistance, hyperinsulinemia, and hyperandrogenemia in the etiopathogenesis and progression of polycystic ovary syndrome and related comorbidities. SAT = subcutaneous adipose tissue; VAT = visceral adipose tissue LH = luteinizing hormone; SHBG = sex hormone binding globulin; IGFBP-1 = insulin-like growth factor binding protein-1; IGF-1 = insulin-like growth factor-1; FFA = free fatty acids; TIMF = type I muscle fibers; TIIMF = type II muscle fibers. Although details of the exact etiopathogenesis of PCOS are not clear, it appears to be a combination of environmental and genetic factors, which in consonance favor the development of IR. In turn, IR leads to compensatory Hyperinsulinemia, which substantially augments ovarian androgen synthesis by increasing LH pulse frequency at the hypophysis by stimulating GnRH gene transcription in hypothalamic cells. Insulin also triggers hyperandrogenemia by directly activating mitogenic pathways in ovarian cells and increasing transcription of StAR and several key steroidogenic enzymes. Hyperandrogenemia is the key disruption underlying the typical clinical features of PCOS. In addition, increased ovarian production of androgens may in turn worsen IR, thus perpetuating a vicious cycle of IR-hyperinsulinemia-hyperandrogenemia. Indeed, androgens may not only interfere with insulin signaling directly, but also trigger lipolysis, increasing FFA in circulation, favoring IR. Moreover, androgens seem to diminish highly oxidative and insulin-sensitive TIMF and increase glycolytic and less insulin-sensitive TIIMF, further favoring the development of IR. Additionally, obesity appears to magnify all events in this cycle, by increasing androgen synthesis not only in ovaries, but also in SAT and adrenal glands. Leptin also participates by disrupting ovarian physiology and favoring a chronic systemic inflammatory state. Ultimately, both IR and chronic inflammation thrive on all endocrine-metabolic disturbances pertaining PCOS, predisposing patients to the development of comorbidities, such as type 2 diabetes mellitus and cardiovascular disease.
