Abstract
Purpose
To evaluate the influence of timing of salvage and adjuvant radiation therapy on outcomes after prostatectomy for prostate cancer.
Methods
Using the Surveillance, Epidemiology, and End Results-Medicare linked database, we identified prostate cancer patients diagnosed during 1995–2007 who had one or more adverse pathological features after prostatectomy. The final cohort of 6,137 eligible patients included men who received prostatectomy alone (n = 4,509) or with adjuvant (n = 894) or salvage (n = 734) radiation therapy. Primary outcomes were genitourinary, gastrointestinal, and erectile dysfunction events and survival after treatment(s).
Results
Radiation therapy after prostatectomy was associated with higher rates of gastrointestinal and genitourinary events, but not erectile dysfunction. In adjusted models, earlier treatment with adjuvant radiation therapy was not associated with increased rates of genitourinary or erectile dysfunction events compared to delayed salvage radiation therapy. Early adjuvant radiation therapy was associated with lower rates of gastrointestinal events that salvage radiation therapy, with hazard ratios of 0.80 (95% CI, 0.67–0.95) for procedure-defined and 0.70 (95% CI, 0.59, 0.83) for diagnosis-defined events. There was no significant difference between ART and non-ART groups (SRT or RP alone) for overall survival (HR = 1.13 95% CI = (0.96, 1.34) p = 0.148).
Conclusions
Radiation therapy after prostatectomy is associated with increased rates of gastrointestinal and genitourinary events. However, earlier radiation therapy is not associated with higher rates of gastrointestinal, genitourinary or sexual events. These findings oppose the conventional belief that delaying radiation therapy reduces the risk of radiation-related complications.
Introduction
There are over 230,000 new prostate cancer (PC) diagnoses in the United States each year [1], and one-third of affected men choose to undergo radical prostatectomy (RP) [2]. One in 5 PC patients recur after RP [3], and recurrence rates are higher, 40–60%, for patients with one or more adverse pathological features (APFs), including: extracapsular extension (ECE), seminal vesicle invasion (SVI) or positive surgical margin (PSM) [4]. For PC patients who are at higher risk of recurrence, adjuvant radiation therapy (ART) to the prostate bed may be offered based on adverse pathologic factors (APFs) alone without a detectable prostate specific antigen (PSA) blood level after surgery. ART has been shown in randomized trials to improve PSA-relapse free survival [5–7], distant metastasis-free survival and overall survival [8], compared to observation.
However, less than 20% of qualifying patients in the United States receive ART [9–11]. Many clinicians prefer to follow patients after RP and to deliver salvage radiation therapy (SRT) to the prostate bed when the PSA level rises [12], a potentially curative strategy [13]. The primary reasons cited for choosing selective SRT over ART include the perceived toxicity of post-RP RT, the potential overtreatment of patients with ART who may not have recurred after RP, the importance of delaying RT to allow time for recovery of urinary and sexual function after RP, and the presumed equivalence of ART and SRT strategies for cancer control [12]. A national survey of urologists and radiation oncologists demonstrated that providers’ perceptions of the risk of radiation-induced urinary complications significantly impacted the likelihood of recommending ART after RP for patients with APFs [14].
Although the risk of toxicity influences ART decisions, the available evidence on this topic is limited. In a randomized controlled trial of ART versus observation conducted by the Southwest Oncology Group (SWOG), which included conventional RT techniques, complete urinary incontinence was more common after ART than after RP alone (6.5% versus 2.8%, p = 0.11) [5]. However, two other randomized trials did not show an increase in urinary incontinence after ART compared to RP alone [6,15].
Given the relevance of toxicity risk, and the influence of radiation timing, to decisions regarding post-RP RT, it is important to provide additional evidence. Trials designed to directly compare ART to selective use of SRT are ongoing, but results are not expected for a decade or longer. This analysis of a population-based cohort was designed to evaluate the comparative effectiveness of early post-prostatectomy RT (ART), compared to prostatectomy alone and delayed RT (SRT), for prostate cancer patients who qualify for adjuvant RT based on APFs. Important secondary objectives include evaluation of predictors of RT utilization after prostatectomy, the influence of RT timing on risk of complication events, and the impact of delaying RT on survival among high-risk patients.
Materials and Methods
Data Source
The Surveillance, Epidemiology, and End Results (SEER) database contains data from population-based tumor registries in several regions of the United States and represents approximately 26% of the total United States population [16]. The SEER-Medicare linked database matches administrative claims data from Medicare with subjects from the SEER registry for United States citizens ages 65 years and older who are Medicare beneficiaries [17]. The SEER-Medicare database has been used previously to compare outcomes after intensity-modulated radiation therapy versus conformal radiation therapy in the post-prostatectomy setting [18,19]. The research was conducted according to the data use agreement of SEER-Medicare, and the manuscript was approved by SEER-Medicare prior to submission. Patient records were anonymized and de-identified prior to analysis.
Study Cohort
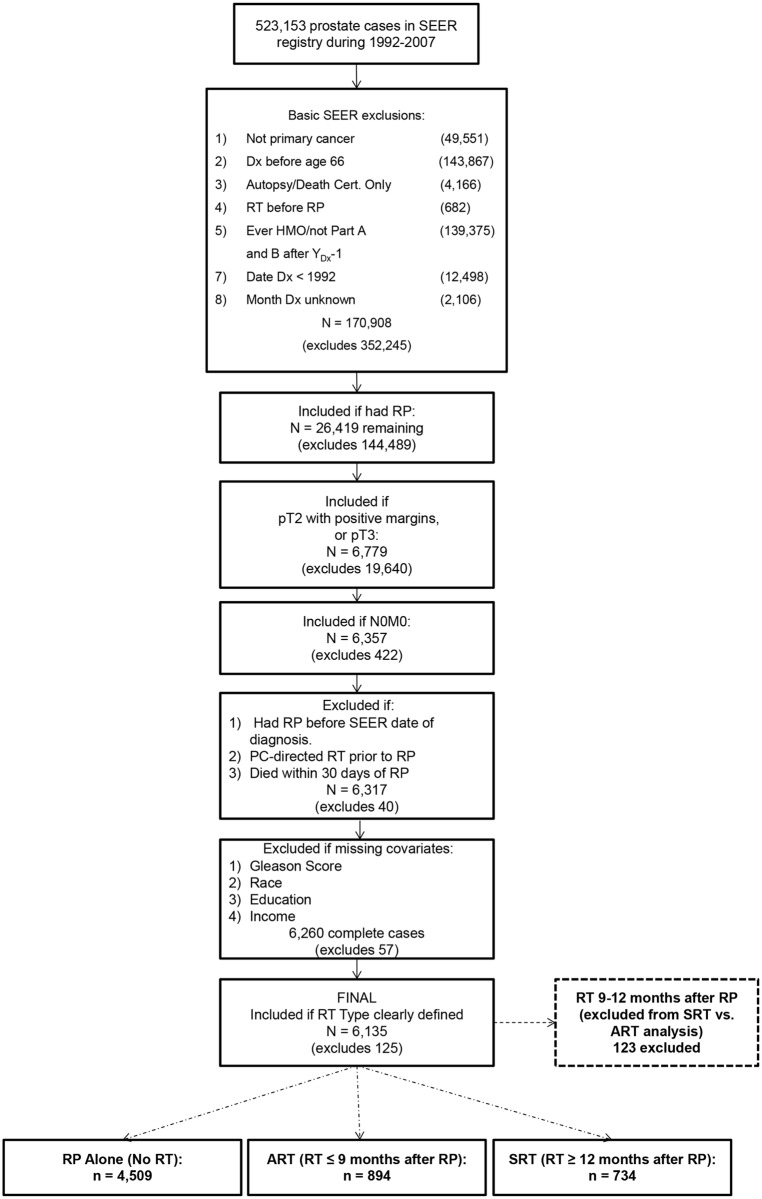
After Thomas Jefferson University institutional review board approval, the SEER-Medicare database was searched to identify 523,153 men who were diagnosed with prostate cancer between 1992 and 2007, who were enrolled continuously in both Parts A and B of Medicare, and who had at least 30 days of observation after RP. The cohort was reduced to 170,908 prostate cancer patients after excluding individuals with a previous cancer diagnosis, those who were diagnosed before age 66 years, men who were enrolled in a health maintenance organization (HMO) at any time starting 1 year prior to their prostate cancer diagnosis, and other reasons that would limit data availability (Fig. 1). Of these men, a total of 26,419 received RP. From this group, a cohort of 6,357 men were considered eligible for ART based on the presence of one or more APFs in the RP surgical specimen (pT3 or pT2 with positive margins) and no evidence of regional (N0) or distant (M0) metastases. A further 29 men were excluded due to prior PC-directed RT or due to a record for RP prior to diagnosis. Eleven were excluded due to death within 30 days of RP, as 30-days post-RP was the starting point for the complication events analyses. Subsequent exclusions were made due to missingness in potential confounders: tumor grade, race, education and income information. Treatment, complication and comorbidity information were extracted from the Medicare administrative claims, using Current Procedural Terminology (CPT), Healthcare Common Procedure Coding System (HCPCS) and associated International Classification of Diseases (ICD) codes (see S1 Table). The administrative claims codes used in the current analysis were adapted from several prior published reports [20–23]. Among these men, a total of 4,509 received RP alone, and 1,751 received RP followed by postoperative RT (Fig. 1).
Fig 1. Flow diagram designed to illustrate the development of the study cohort through stepwise exclusions using SEER registry data elements and administrative codes from the Medicare database.
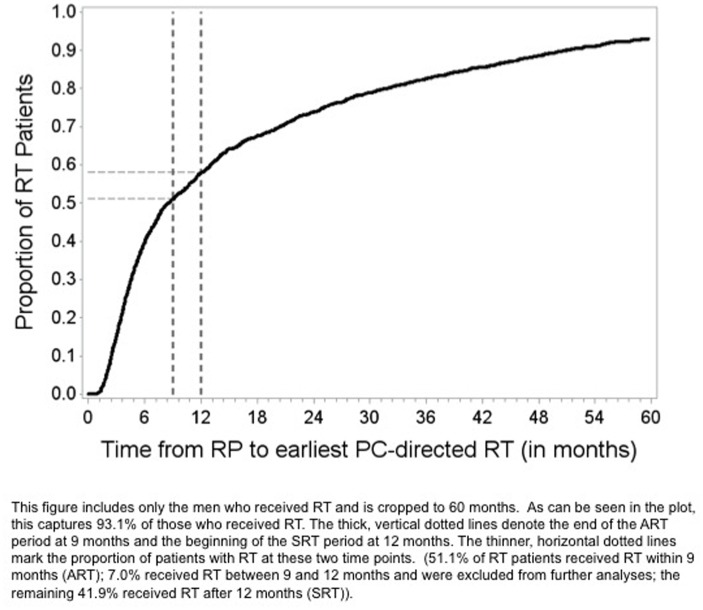
In order to evaluate the hypothesis that delaying the delivery of post-RP RT influences outcomes, the group of patients who received RT was further classified based upon length of time from RP to RT as ART (RT within 9 months of RP, n = 894) and delayed SRT (RT 12+ months after RP, n = 734). The SEER-Medicare database does not provide data regarding the intent of RT, nor technical details regarding the RT fields, so RT timing was used as a surrogate classifier of adjuvant versus salvage therapy. The investigators chose this ART/SRT classification system empirically based upon impressions regarding clinicians’ practices regarding ART timing, with support from the results of a prior national survey [14]. Patients receiving RT between 9 and 12 months after RP (n = 123) were excluded from analyses of ART and SRT to limit misclassification of ART versus SRT.
Outcomes
First complication events were evaluated after RP for each of four categories: erectile dysfunction (ED), gastrointestinal (GI), urinary incontinence (UI), and urinary non-incontinence (UN). Complication events were identified from Medicare claims based upon HCPCS/CPT-4 procedure codes and ICD-9 diagnosis codes (S1 Table); procedure code-defined and diagnosis code-defined events were analyzed separately. The observation period for events began 30 days after RP in order to ignore acute complications. Event rates for RP followed by RT include complications attributable to either or both interventions, while the RP alone cohort serves as a control for comparisons. Times to complication event were measured from 30 days post-RP to the first event date or censored at death or end of study, December 31, 2008. Overall and prostate cancer-specific survival times were measured from date of diagnosis to death or censoring at the end of study. Further details about control variables are provided in (S1 Text).
Statistical Analysis
Patient characteristics among RP alone, ART and SRT groups were compared using chi-square test. Multivariable analysis (MVA) with polytomous logistic regression was performed to evaluate predictors of ART utilization (versus either no RT or SRT). This model included the following covariates: race, Hispanic origin, marital status, census-tract % high school completion, census-tract median income, population density, SEER region, year of diagnosis, pT stage, tumor grade, margin status, age at diagnosis, comorbidity score, androgen deprivation therapy receipt, surgery type and indicators for having a history of ED, GI, UI and UN events (based on procedure and diagnosis codes combined) in the year prior to RP. From this model, a propensity score weight was calculated as the inverse predicted probability of being in one’s treatment group; this weight was then adjusted by the relative sample size of each treatment group.[24] Propensity score weighting was used to adjust for potential differences in baseline characteristics between patients in the RP alone and RP plus RT groups, and characteristics were compared again using the chi-square test.
First complication events (based on either procedure or diagnosis code) were reported in events/100 person years within each treatment group as fixed at the end of study. Adjustment for potential confounders was performed by propensity score weighting [25]. 95% confidence intervals of adjusted rate ratios were calculated via propensity-weighted Poisson regression incorporating an offset of complication-free survival time [26]. The investigators designed the Poisson regression model in order to estimate and compare event rates among the three cohorts. All comparison tests were 2-tailed, and the threshold for statistical significance was p = 0.05.
The primary analysis was comprised of multivariate Cox proportional hazards models of time to first event were performed for each class of events (ED, GI, UI, UN) with procedure code-defined and diagnosis code-defined classes being considered separately. Radiotherapy type—RP alone, ART or SRT—was included as a time-dependent variable [27]. The inclusion of RT as a time-dependent variable in these models allowed for an individual’s RT status to change over time. That is, all men began the study period in the RP alone group and then, over the course of the follow-up period, some men switch to the RP and ART group, others to the RP and SRT group, while others remain in the RP alone group for the duration. Considering the addition of ART and SRT separately allowed for the evaluation of the influence of RT timing on the probability of complication events. All models included the potential confounders contained in Table 1 and were weighted by the propensity score. Hazard ratios were calculated with 95% confidence intervals and p values were considered significant if < 0.05.
Table 1. Demographic and clinical characteristics of subjects who received radical prostatectomy (RP) alone, RP followed by adjuvant radiation therapy, or RP followed by salvage radiation therapy.
| Predictor | Total | Radiotherapy Use | p | ||||||
|---|---|---|---|---|---|---|---|---|---|
| RP only | ART (<9mo) | SRT (12mo+) | |||||||
| N | Col % | N | Col % | N | Col % | N | Col % | ||
| Total | 6,137 | 100 | 4,509 | 100 | 894 | 100 | 734 | 100 | |
| Pathological T-Stage | <0.001 | ||||||||
| T2 | 1,856 | 30.2 | 1,494 | 33.1 | 181 | 20.2 | 181 | 24.7 | |
| T3a | 3,140 | 51.2 | 2,294 | 50.9 | 467 | 52.2 | 379 | 51.6 | |
| T3b | 1,141 | 18.6 | 721 | 16.0 | 246 | 27.5 | 174 | 23.7 | |
| Margin Status | 0.259 | ||||||||
| Uninvolved | 3,175 | 51.7 | 2,308 | 51.2 | 468 | 52.3 | 399 | 54.4 | |
| Involved | 2,962 | 48.3 | 2,201 | 48.8 | 426 | 47.7 | 335 | 45.6 | |
| Gleason Score | <0.001 | ||||||||
| ≤7 | 4,233 | 69.0 | 3,384 | 75.0 | 431 | 48.2 | 418 | 56.9 | |
| 8+ | 1,904 | 31.0 | 1,125 | 25.0 | 463 | 51.8 | 316 | 43.1 | |
| Age at Diagnosis | 0.002 | ||||||||
| 66–69 | 3,234 | 52.7 | 2,306 | 51.1 | 507 | 56.7 | 421 | 57.4 | |
| 70–74 | 2,357 | 38.4 | 1,784 | 39.6 | 313 | 35.0 | 260 | 35.4 | |
| 75–79 | 546 | 8.9 | 419 | 9.3 | 74 | 8.3 | 53 | 7.2 | |
| Comorbidity Score | 0.027 | ||||||||
| 0 | 3,765 | 61.3 | 2,719 | 60.3 | 565 | 63.2 | 481 | 65.5 | |
| 1 | 1,637 | 26.7 | 1,222 | 27.1 | 231 | 25.8 | 184 | 25.1 | |
| 2+ | 735 | 12.0 | 568 | 12.6 | 98 | 11.0 | 69 | 9.4 | |
| Diagnosis Year | <0.001 | ||||||||
| 1995–1999 | 1,576 | 25.7 | 1,103 | 24.5 | 228 | 25.5 | 245 | 33.4 | |
| 2000–2004 | 2,696 | 43.9 | 1,940 | 43.0 | 382 | 42.7 | 374 | 51.0 | |
| 2005–2007 | 1,865 | 30.4 | 1,466 | 32.5 | 284 | 31.8 | 115 | 15.7 | |
| Race | 0.126 | ||||||||
| White | 5,509 | 89.8 | 4,051 | 89.8 | 793 | 88.7 | 665 | 90.6 | |
| Black | 368 | 6.0 | 281 | 6.2 | 51 | 5.7 | 36 | 4.9 | |
| Other/Unspecified | 260 | 4.2 | 177 | 3.9 | 50 | 5.6 | 33 | 4.5 | |
| Hispanic Ethnicity | 0.399 | ||||||||
| Non-Hispanic | 5,759 | 93.8 | 4,220 | 93.6 | 845 | 94.5 | 694 | 94.6 | |
| Hispanic | 378 | 6.2 | 289 | 6.4 | 49 | 5.5 | 40 | 5.4 | |
| Marital Status | 0.381 | ||||||||
| Not Married | 868 | 14.1 | 658 | 14.6 | 121 | 13.5 | 89 | 12.1 | |
| Married | 5,113 | 83.3 | 3,733 | 82.8 | 751 | 84.0 | 629 | 85.7 | |
| Unknown | 156 | 2.5 | 118 | 2.6 | 22 | 2.5 | 16 | 2.2 | |
| HS Education Attainment | 0.164 | ||||||||
| <75% | 1,068 | 17.4 | 804 | 17.8 | 156 | 17.4 | 108 | 14.7 | |
| 75–84.99% | 1,387 | 22.6 | 1,037 | 23.0 | 196 | 21.9 | 154 | 21.0 | |
| 85–89.99% | 1,196 | 19.5 | 878 | 19.5 | 164 | 18.3 | 154 | 21.0 | |
| 90%+ | 2,486 | 40.5 | 1,790 | 39.7 | 378 | 42.3 | 318 | 43.3 | |
| Median Household Income | 0.446 | ||||||||
| <35K | 1,233 | 20.1 | 928 | 20.6 | 169 | 18.9 | 136 | 18.5 | |
| 35K-44K | 1,305 | 21.3 | 966 | 21.4 | 175 | 19.6 | 164 | 22.3 | |
| 45K-59K | 1,526 | 24.9 | 1,105 | 24.5 | 240 | 26.8 | 181 | 24.7 | |
| 60K+ | 2,073 | 33.8 | 1,510 | 33.5 | 310 | 34.7 | 253 | 34.5 | |
| Population Density | 0.802 | ||||||||
| Urban | 6,030 | 98.3 | 4,432 | 98.3 | 879 | 98.3 | 719 | 98.0 | |
| Rural | 107 | 1.7 | 77 | 1.7 | 15 | 1.7 | 15 | 2.0 | |
| Treatment Region | 0.140 | ||||||||
| West | 3,771 | 61.4 | 2,766 | 61.3 | 557 | 62.3 | 448 | 61.0 | |
| Midwest | 1,100 | 17.9 | 825 | 18.3 | 134 | 15.0 | 141 | 19.2 | |
| Northeast | 573 | 9.3 | 406 | 9.0 | 100 | 11.2 | 67 | 9.1 | |
| South | 693 | 11.3 | 512 | 11.4 | 103 | 11.5 | 78 | 10.6 | |
| Radical Prostatectomy Type | <0.001 | ||||||||
| Open | 5,250 | 85.5 | 3,799 | 84.3 | 769 | 86.0 | 682 | 92.9 | |
| MIRP | 887 | 14.5 | 710 | 15.7 | 125 | 14.0 | 52 | 7.1 | |
| Androgen Deprivation Therapy | <0.001 | ||||||||
| No | 4,371 | 71.2 | 3,654 | 81.0 | 396 | 44.3 | 321 | 43.7 | |
| Yes | 1,766 | 28.8 | 855 | 19.0 | 498 | 55.7 | 413 | 56.3 | |
| History of ED | 0.180 | ||||||||
| No | 5,475 | 89.2 | 4,006 | 88.8 | 813 | 90.9 | 656 | 89.4 | |
| Yes | 662 | 10.8 | 503 | 11.2 | 81 | 9.1 | 78 | 10.6 | |
| History of GI | 0.031 | ||||||||
| No | 4,836 | 78.8 | 3,517 | 78.0 | 719 | 80.4 | 600 | 81.7 | |
| Yes | 1,301 | 21.2 | 992 | 22.0 | 175 | 19.6 | 134 | 18.3 | |
| History of UI | 0.102 | ||||||||
| No | 5,279 | 86.0 | 3,860 | 85.6 | 769 | 86.0 | 650 | 88.6 | |
| Yes | 858 | 14.0 | 649 | 14.4 | 125 | 14.0 | 84 | 11.4 | |
| History of UN | 0.978 | ||||||||
| No | 5,122 | 83.5 | 3,765 | 83.5 | 744 | 83.2 | 613 | 83.5 | |
| Yes | 1,015 | 16.5 | 744 | 16.5 | 150 | 16.8 | 121 | 16.5 | |
ART = adjuvant radiation therapy; SRT = adjuvant radiation therapy; HS = high school; MIRP = minimally-invasive radical prostatectomy; ED = erectile dysfunction; GI = gastrointestinal; UI = urinary incontinence; UN = urinary non-incontinence
The impact of radiation on overall and prostate cancer specific survival was evaluated using multivariable Cox proportional hazard models with radiation type (RP only, ART, or SRT) as a time-dependent covariate. The model was weighted by propensity score and adjusted for various clinical, demographic and socioeconomic covariates including: pT stage, tumor grade, surgical margins, age at diagnosis, surgery type, use of androgen deprivation therapy (ADT) at any time, race, ethnicity, median household income, education level, SEER region, year of diagnosis, marital status, population density, comorbidity score and history variables.
Results
The cohort was comprised of a total of 6,137 PC subjects who received RP and were eligible for ART. The cohort is further categorized as RP alone (n = 4,509), ART (n = 894) or SRT (n = 734). RT was delivered for a total of 26.5% of subjects at a median of 7.5 months (Fig. 2). ART was delivered for 894 of these subjects (14.6%). Among those who did not receive ART, 14.0% later received SRT. Median follow up from diagnosis was 64 months, 62.9 months, and 84.2 months for the RP alone, RP and ART, and RP and SRT cohorts, respectively. Clinical and demographic characteristics for the RP alone, RP and ART, and RP and SRT cohorts are summarized in Table 1. On univariable analysis, significant differences were found between treatment groups with regards to pT stage, tumor grade, age at diagnosis, comorbidity score, diagnosis year, surgery type, use of ADT at any time, and history of GI. However, after propensity-score weighting only year of diagnosis remained significant (results not shown).
Fig 2. Time from radiation therapy to radical prostatectomy (RP), in months, for the study cohort of men in the SEER-Medicare database who qualified for adjuvant radiation therapy based upon the presence of one of more adverse pathological feature in the prostatectomy specimen.
On MVA, predictors of ART utilization included: pT stage, tumor grade, margin status, comorbidity score, age at diagnosis, use of ADT, and year of diagnosis. ART was more likely in patients with more advanced disease with regards to pT stage or APFs than RP alone or SRT. The odds of ART use over RP alone were much higher in those who also received ADT at any time during the study period (RP alone vs. ART: OR = 0.23 (0.20, 0.28) p <0.001) (Table 2).
Table 2. Multivariable analysis with polytomous logistic regression performed to evaluate predictors of ART utilization versus no RT or SRT.
| RP alone vs. ART | SRT vs. ART | ||||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | p | |
| Race | 0.641 | ||||||
| Black vs. White | 1.04 | (0.73, 1.48) | 0.831 | 0.89 | (0.55, 1.43) | 0.627 | |
| Other/Unspecified vs. White | 0.79 | (0.55, 1.14) | 0.205 | 0.94 | (0.59, 1.51) | 0.809 | |
| Hispanic Ethnicity | 0.314 | ||||||
| Hispanic vs. Non-Hispanic | 1.30 | (0.92, 1.86) | 0.139 | 1.15 | (0.72, 1.82) | 0.561 | |
| Marital Status | 0.447 | ||||||
| Not Married vs. Married | 1.14 | (0.91, 1.43) | 0.266 | 0.92 | (0.68, 1.24) | 0.581 | |
| Unknown vs. Married | 0.90 | (0.55, 1.47) | 0.659 | 0.97 | (0.50, 1.88) | 0.920 | |
| HS Education Attainment | 0.117 | ||||||
| 75–84.99% vs. <75% | 1.08 | (0.82, 1.43) | 0.571 | 1.13 | (0.79, 1.62) | 0.513 | |
| 85–89.99% vs. <75% | 1.07 | (0.79, 1.47) | 0.655 | 1.42 | (0.95, 2.13) | 0.087 | |
| 90%+ vs. <75% | 0.89 | (0.65, 1.23) | 0.492 | 1.33 | (0.88, 2.03) | 0.178 | |
| Median Household Income | 0.538 | ||||||
| 35K-44K vs. <35K | 0.96 | (0.74, 1.26) | 0.790 | 1.01 | (0.71, 1.41) | 0.977 | |
| 45K-59K vs. <35K | 0.87 | (0.65, 1.15) | 0.322 | 0.83 | (0.58, 1.19) | 0.308 | |
| 60K+ vs. <35K | 1.05 | (0.76, 1.45) | 0.757 | 0.90 | (0.60, 1.36) | 0.616 | |
| Population Density | 0.985 | ||||||
| Rural vs. Urban | 0.98 | (0.53, 1.82) | 0.958 | 1.04 | (0.49, 2.22) | 0.923 | |
| Treatment Region | 0.156 | ||||||
| Midwest vs. West | 1.31 | (1.04, 1.66) | 0.023 | 1.23 | (0.92, 1.65) | 0.167 | |
| Northeast vs. West | 0.81 | (0.62, 1.06) | 0.120 | 0.90 | (0.63, 1.29) | 0.574 | |
| South vs. West | 1.00 | (0.76, 1.30) | 0.968 | 1.04 | (0.74, 1.48) | 0.809 | |
| Year of Diagnosis | <0.001 | ||||||
| 2000–2004 vs. 1995–1999 | 0.95 | (0.78, 1.17) | 0.633 | 0.99 | (0.77, 1.27) | 0.930 | |
| 2005–2007 vs. 1995–1999 | 0.85 | (0.67, 1.07) | 0.164 | 0.43 | (0.32, 0.60) | <0.001 | |
| Pathological T-Stage | <0.001 | ||||||
| T3a vs. T2 | 0.50 | (0.40, 0.63) | <0.001 | 0.64 | (0.47, 0.86) | 0.003 | |
| T3b vs. T2 | 0.31 | (0.23, 0.43) | <0.001 | 0.48 | (0.32, 0.73) | <0.001 | |
| Gleason Score | <0.001 | ||||||
| 8+ vs. ≤7 | 0.45 | (0.39, 0.53) | <0.001 | 0.69 | (0.56, 0.85) | <0.001 | |
| Margins Status | <0.001 | ||||||
| Involved vs. Uninvolved | 0.45 | (0.36, 0.56) | <0.001 | 0.63 | (0.48, 0.84) | 0.001 | |
| Age at Diagnosis | <0.001 | ||||||
| 70–74 vs. 65–69 | 1.36 | (1.16, 1.61) | <0.001 | 0.98 | (0.79, 1.21) | 0.840 | |
| 75–79 vs. 65–69 | 1.67 | (1.24, 2.25) | <0.001 | 0.97 | (0.65, 1.44) | 0.865 | |
| 80+ vs. 65–69 | 2.00 | (0.77, 5.19) | 0.152 | 0.71 | (0.18, 2.91) | 0.637 | |
| Comorbidity Score | 0.027 | ||||||
| 1 vs. 0 | 1.14 | (0.95, 1.37) | 0.149 | 0.96 | (0.76, 1.21) | 0.740 | |
| 2+ vs. 0 | 1.25 | (0.97, 1.61) | 0.079 | 0.85 | (0.60, 1.19) | 0.331 | |
| Androgen Deprivation Therapy | <0.001 | ||||||
| Yes vs. No | 0.23 | (0.20, 0.28) | <0.001 | 1.14 | (0.93, 1.42) | 0.215 | |
| Radical Prostatectomy Type | 0.064 | ||||||
| MIRP vs. Open | 1.10 | (0.85, 1.41) | 0.473 | 0.74 | (0.50, 1.08) | 0.116 | |
| History of ED | 0.130 | ||||||
| Yes vs. No | 1.24 | (0.95, 1.62) | 0.113 | 1.40 | (1.00, 1.97) | 0.049 | |
| History of GI | 0.363 | ||||||
| Yes vs. No | 1.07 | (0.88, 1.30) | 0.494 | 0.92 | (0.72, 1.19) | 0.538 | |
| History of UI | 0.989 | ||||||
| Yes vs. No | 1.00 | (0.79, 1.28) | 0.971 | 0.98 | (0.71, 1.36) | 0.920 | |
| History of UN | 0.761 | ||||||
| Yes vs. No | 1.08 | (0.87, 1.35) | 0.488 | 1.03 | (0.77, 1.37) | 0.841 | |
ART = adjuvant radiation therapy; SRT = adjuvant radiation therapy; RP = radical prostatectomy; HS = high school; MIRP = minimally-invasive radical prostatectomy; ED = erectile dysfunction; GI = gastrointestinal; UI = urinary incontinence; UN = urinary non-incontinence
Propensity score-adjusted complication rates were compared for RP alone, RP and ART, and RP and SRT (Table 3). The addition of ART or SRT after RP was not associated with higher rates of ED events, compared to RP alone. Rates of GI events were higher among patients who received ART or SRT than RP alone. ART was associated with higher rates of GU nonincontinence events than RP alone or RT followed by SRT (Table 3).
Table 3. Propensity score-adjusted complication rates, by class, for radical prostatectomy alone or in combination with ART (≤ 9 months after RP) or SRT (≥ 12 months after RP).
| No RT n* = 4,521 | ART n* = 908 | SRT n* = 724 | ART vs. No RT | SRT vs. No RT | ART vs. SRT | |
|---|---|---|---|---|---|---|
| Complication Class | Adjusted Rate (Events/100 Person Years) | Adjusted Rate (Events/ 100 Person Years) | Adjusted Rate (Events/ 100 Person Years) | Adjusted Rate Ratio (95% CI) | Adjusted Rate Ratio (95% CI) | Adjusted Rate Ratio (95% CI) |
| ED | ||||||
| Procedures | 2.07 | 1.80 | 2.02 | 0.87 (0.69, 1.09) | 0.98 (0.77, 1.24) | 0.89 (0.66, 1.21) |
| Diagnoses | 12.73 | 11.01 | 13.04 | 0.87 (0.78, 0.96) | 1.02 (0.91, 1.15) | 0.84 (0.73, 0.98) |
| GI | ||||||
| Procedures | 13.87 | 16.02 | 17.06 | 1.15 (1.05, 1.27) | 1.23 (1.11, 1.36) | 0.94 (0.83, 1.07) |
| Diagnoses | 9.90 | 12.68 | 12.96 | 1.28 (1.16, 1.42) | 1.31 (1.17, 1.46) | 0.98 (0.85, 1.12) |
| GU-Incontinence | ||||||
| Procedures | 5.88 | 6.58 | 6.74 | 1.12 (0.98, 1.27) | 1.15 (1.00, 1.32) | 0.98 (0.82, 1.16) |
| Diagnoses | 9.67 | 11.30 | 9.30 | 1.17 (1.05, 1.30) | 0.96 (0.85, 1.09) | 1.21 (1.05, 1.41) |
| GU- NonIncontinence | ||||||
| Procedures | 3.78 | 5.51 | 3.58 | 1.46 (1.26, 1.69) | 0.95 (0.79, 1.14) | 1.54 (1.24, 1.91) |
| Diagnoses | 7.39 | 9.39 | 8.46 | 1.27 (1.13, 1.43) | 1.14 (1.00, 1.31) | 1.11 (0.95, 1.30) |
*Propensity score-weighted sample sizes.
Multivariate Cox proportional hazards models with RT as a time-dependent covariate were performed for GI, ED, GU incontinence and GU non-incontinence events (see S2–S5 Tables), and summary results of comparisons are shown in Table 4. ART and SRT were associated with higher rates of GI and GU, but not ED, events than RP alone. Earlier treatment with ART was associated with lower rates of GI events than SRT, and no increase in GU events (Table 4).
Table 4. Summary of findings from multivariable models of complication with RT as time-dependent covariate.
| ART vs. RP alone | SRT vs. RP alone | ART vs. SRT | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Complication Class | n | HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p |
| ED | ||||||||||
| Procedures | 634 | 0.99 | (0.78, 1.24) | 0.896 | 0.54 | (0.26, 1.14) | 0.104 | 1.82 | (0.85, 3.91) | 0.125 |
| Diagnoses | 2,770 | 0.87 | (0.77, 0.99) | 0.033 | 0.77 | (0.55, 1.07) | 0.113 | 1.14 | (0.81, 1.61) | 0.460 |
| GI | ||||||||||
| Procedures | 3,146 | 1.17 | (1.06, 1.29) | 0.003 | 1.46 | (1.25, 1.69) | <0.001 | 0.80 | (0.67, 0.95) | 0.011 |
| Diagnoses | 2,582 | 1.35 | (1.21, 1.50) | <0.001 | 1.93 | (1.67, 2.23) | <0.001 | 0.70 | (0.59, 0.83) | <0.001 |
| GU-Incontinence | ||||||||||
| Procedures | 1,701 | 1.22 | (1.05, 1.41) | 0.008 | 1.40 | (1.12, 1.76) | 0.004 | 0.87 | (0.67, 1.12) | 0.281 |
| Diagnoses | 2,395 | 1.29 | (1.13, 1.46) | <0.001 | 1.33 | (1.04, 1.69) | 0.022 | 0.97 | (0.75, 1.26) | 0.818 |
| GU- Non-Incontinence | ||||||||||
| Procedures | 1,148 | 1.71 | (1.45, 2.01) | <0.001 | 1.42 | (1.02, 1.97) | 0.039 | 1.21 | (0.85, 1.71) | 0.293 |
| Diagnoses | 1,967 | 1.48 | (1.29, 1.68) | <0.001 | 1.46 | (1.15, 1.85) | 0.002 | 1.01 | (0.78, 1.31) | 0.926 |
Full models for each complication class displayed in Online Supplementary materials.
A total of 981 men died during the observation period; 229 of these deaths were attributed to prostate cancer in the SEER registry. Both overall and prostate cancer-specific survival was worse in the RT groups compared to RP alone. There was no significant difference between ART and non-ART groups (SRT or RP alone) for overall survival (HR = 1.13 95% CI = (0.96, 1.34) p = 0.148). Prostate cancer specific survival was significantly shorter for the ART group compared to the non-ART groups (HR = 1.88 95% CI = (1.35, 2.61) p < 0.001). There was no significant difference in the overall survival of those with ART compared to those with SRT (HR = 0.88 95%CI = (0.68, 1.13) p = 0.305). However, there was a significant difference in the prostate cancer-specific survival of the two RT groups, with a survival benefit seen in the ART group compared to the SRT group (HR = 0.64 95% CI = (0.42, 0.97) p = 0.036).
Discussion
In this analysis of a large, population-based cohort of patients from the SEER-Medicare database, 14.3% of patients eligible for ART after RP received RT within 9 months after RP and another 11.7% received delayed SRT; a further 2.0% received RT between 9 and 12 months after RP and were excluded from further analyses. Two sets of adjusted analyses, a Poisson regression model and multivariate Cox proportional hazards models with RT as a time-varying covariate, were performed to estimate the occurrence of events after post-RP RT in this cohort and to evaluate the influence of RT timing on outcomes. Observed rates of GI and some GU events, but not ED, were higher in the ART and SRT groups compared to RP alone. Adjusted analyses evaluating RT as a time-dependent covariate revealed that early treatment with ART was associated with lower rates of GI events, and no difference in GU or ED events. There was no overall survival difference observed between ART and non-ART groups.
The current study showed an increased risk of GI and GU, but not ED, events with the addition of ART or SRT after RP. The increase in GI and GU events is consistent with the published literature [12,28,29], and the potential benefits of ART and SRT must be balanced against the incremental risk of GI and GU side effects. The delivery of RT after RP was not associated with increased rate of procedures for ED-related events, which is consistent with the available evidence. It is not clear what the impact of RT is on erectile function after RP, and most men who receive post-RP RT have erectile dysfunction prior to RT [28]. The current study contributes to the existing evidence for post-RP RT by directly examining the influence of RT timing on the occurrence of complication events.
GI events occurred at a higher rate among patients who received SRT than in the ART group (Table 4). Although it is not plausible that prolonged interval between RP and RT would, on its own, cause this increase in events, it is possible that differences in radiation doses used for ART versus SRT may influence risk of GI events. There is evidence that higher SRT doses may result in higher biochemical disease free survival rates [30–32], but may also increase rates of grade 3 and higher GI complications [33]. Since the SEER-Medicare database lacks details regarding radiation doses and technical details, it is not possible for the current study to evaluate whether higher doses were delivered in the SRT group, and this observation warrants additional study.
The study’s external validity is enhanced by the large number of subjects, with a broad range of demographic factors and baseline medical comorbidities. However, there are significant limitations to the study that warrant consideration and attenuate conclusions from this work [34,35]. The SEER-Medicare database lacks details regarding specific intent of the RT courses delivered. Furthermore, there are no data regarding the specifics of the RT fields, and it is possible that some subjects received treatment to sites other than the prostate bed such as metastases. We addressed this issue by limiting the analysis to patients with APFs, who are at higher risk of PC recurrence after RP [4], by excluding patients with a previous primary cancer, and by identifying ART and SRT based upon Medicare claims records that included both procedure codes for RT and an associated diagnostic code for prostate cancer. The study years also spans a time period during which the use of intensity-modulated radiation therapy (IMRT) became more frequent [18], which one might hypothesize would influence the observed rates of events in the current study. However, prior reports have not shown a consistent difference in outcomes between IMRT versus 3-dimensional conformal RT using the SEER-Medicare database [18,19]. The study period also included the publication of the seminal randomized controlled trials of ART versus observation, which one might expect to increase rates of ART delivery. However, two previous reports have shown that the positive results from these trials did not influence the utilization of ART in the SEER database [10,11]. Perhaps most importantly, it should be noted that the procedural codes used to identify events are unlikely to capture mild or moderate side effects of RT that may affect patients’ quality of life related to GU, GI and sexual functional deficits. Therefore, the current comparative effectiveness research study is best viewed as providing evidence that complements the available data from previously published research.
In conclusion, the current study compared outcomes after RP alone, or with the addition of ART or SRT, for a large cohort of men who were eligible for ART after RP based upon the presence of APFs in the surgical specimen. The delivery of RT after RP was associated with increased rates of GI and GU, but not ED, events. Earlier treatment with ART did not increase rates of GU and ED events, when compared to delayed treatment with SRT. RT timing did appear to influence prostate cancer-specific survival. These findings regarding the effect of RT timing on risk of complication events for post-RP prostate cancer patients provide information that may be useful in making decisions regarding delivery of ART and SRT while awaiting the results of ongoing trials of ART versus SRT.
Supporting Information
Text and explanatory tables pertinent to the analyses are included.
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
This study used the linked SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the Applied Research Program, NCI; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database.
The collection of the California cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract N01-PC-35136 awarded to the Northern California Cancer Center, contract N01-PC-35139 awarded to the University of Southern California, and contract N02-PC-15105 awarded to the Public Health Institute; and the Centers for Disease Control and Prevention’s National Program of Cancer Registries, under agreement #U55/CCR921930–02 awarded to the Public Health Institute. The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of California, Department of Public Health the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors is not intended nor should be inferred.
Prior Presentation: This study was presented in part at the 55th Annual Meeting of the American Society for Radiation Oncology, Atlanta, GA, September 22–25, 2013.
Data Availability
Data are from SEER-Medicare, a third party. Data requests will be reviewed by SEER-Medicare and will need to comply with SEER-Medicare data use agreement. Requests for data may be sent to SEER-Medicare from the US National Cancer Institute webpage, or by contacting Elaine Yanisko, Information Management Services, Inc., 3901 Calverton Blv, Suite 200, Calverton, MD 2070 (yaniskoe@imsweb.com).
Funding Statement
This research was supported by a 2011 Prostate Cancer Foundation Ben Franklin Young Investigator Award (T. N. S.) and an American Cancer Society Institutional Research Grant #08-060-04 (T. N. S. and Kimmel Cancer Center, Thomas Jefferson University). The funders had no role in the following: the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
References
- 1. Siegel R, Ma J, Zou Z, Jemal A. Cancer Statistics, 2014. CA Cancer J Clin. 2014;64: 9–29. 10.3322/caac.21208 [DOI] [PubMed] [Google Scholar]
- 2. Penson DF, Chan JM, Urologic Diseases in America Project. Prostate cancer. J Urol. 2007;177: 2020–2029. [DOI] [PubMed] [Google Scholar]
- 3. Han M, Partin AW, Pound CR, Epstein JI, Walsh PC. Long-term biochemical disease-free and cancer-specific survival following anatomic radical retropubic prostatectomy. The 15-year Johns Hopkins experience. Urol Clin North Am. 2001;28: 555–565. [DOI] [PubMed] [Google Scholar]
- 4. Swanson GP, Riggs M, Hermans M. Pathologic findings at radical prostatectomy: Risk factors for failure and death. Urol Oncol. 2007;25: 110–114. [DOI] [PubMed] [Google Scholar]
- 5. Thompson IM Jr., Tangen CM, Paradelo J, Lucia MS, Miller G, Troyer D, et al. Adjuvant radiotherapy for pathologically advanced prostate cancer: a randomized clinical trial. JAMA. 2006;296: 2329–2335. [DOI] [PubMed] [Google Scholar]
- 6. Wiegel T, Bottke D, Steiner U, Siegmann A, Golz R, Storkel S, et al. Phase III postoperative adjuvant radiotherapy after radical prostatectomy compared with radical prostatectomy alone in pT3 prostate cancer with postoperative undetectable prostate-specific antigen: ARO 96–02/AUO AP 09/95. J Clin Oncol. 2009;27: 2924–2930. 10.1200/JCO.2008.18.9563 [DOI] [PubMed] [Google Scholar]
- 7. Bolla M, van Poppel H, Collette L, van Cangh P, Vekemans K, Da Pozzo L, et al. Postoperative radiotherapy after radical prostatectomy: a randomised controlled trial (EORTC trial 22911). Lancet. 2005;366: 572–578. [DOI] [PubMed] [Google Scholar]
- 8. Thompson IM, Tangen CM, Klein EA. Is there a standard of care for pathologic stage T3 prostate cancer? J Clin Oncol. 2009;27: 2898–2899. 10.1200/JCO.2008.20.9460 [DOI] [PubMed] [Google Scholar]
- 9. Schreiber D, Rineer J, Yu JB, Oisheski M, Nwokedi E, Schwartz D, et al. Analysis of pathologic extent of disease for clinically localized prostate cancer after radical prostatectomy and subsequent use of adjuvant radiation in a national cohort. Cancer. 2010;116: 5757–5766. 10.1002/cncr.25561 [DOI] [PubMed] [Google Scholar]
- 10. Hoffman KE, Nguyen PL, Chen MH, Chen RC, Choueiri TK, Hu JC, et al. Recommendations for post-prostatectomy radiation therapy in the United States before and after the presentation of randomized trial. J Urol. 2011;185: 116–120. 10.1016/j.juro.2010.08.086 [DOI] [PubMed] [Google Scholar]
- 11. Ghia AJ, Shrieve DC, Tward JD. Adjuvant radiotherapy use and patterns of care analysis for margin-positive prostate adenocarcinoma with extracapsular extension: Postprostatectomy adjuvant radiotherapy: A SEER analysis. Urology. 2010;76: 1169–1174. 10.1016/j.urology.2010.04.047 [DOI] [PubMed] [Google Scholar]
- 12. Nielsen ME, Trock BJ, Walsh PC. Salvage or adjuvant radiation therapy: counseling patients on the benefits. J Natl Compr Canc Netw. 2010;8: 228–237. [DOI] [PubMed] [Google Scholar]
- 13. Trock BJ, Han M, Freedland SJ, Humphreys EB, DeWeese TL, Partin AW, et al. Prostate cancer-specific survival following salvage radiotherapy vs observation in men with biochemical recurrence after radical prostatectomy. JAMA. 2008;299: 2760–2769. 10.1001/jama.299.23.2760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Showalter TN, Ohri N, Teti KG, Foley KA, Keith SW, Trabulsi EJ, et al. Physician beliefs and practices for adjuvant and salvage radiation therapy after prostatectomy. Int J Radiat Oncol Biol Phys. 2012;82: e233–e238. 10.1016/j.ijrobp.2011.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Thompson IM, Tangen CM, Paradelo J, Lucia MS, Troyer D, Messing E, et al. Adjuvant radiotherapy for pathological T3N0M0 prostate cancer significantly reduces risk of metastases and improves survival: long-term followup of a randomized clinical trial. J Urol. 2009;181: 956–962. 10.1016/j.juro.2008.11.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yu JB, Gross CP, Wilson LD, Smith BD. NCI SEER public-use data: Applications and limitations in oncology research. Oncology. 2009;23: 288–295. [PubMed] [Google Scholar]
- 17. Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF. Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care. 2002;40: IV–3–18. [DOI] [PubMed] [Google Scholar]
- 18. Goldin GH, Sheets NC, Meyer A-M, Kuo T-M, Wu Y, Sturmer T, et al. Comparative effectiveness of intensity-modulated radiotherapy and conventional conformal radiotherapy in the treatment of prostate cancer after radical prostatectomy. JAMA Intern Med. 2013;173: 1136–1143. 10.1001/jamainternmed.2013.1020 [DOI] [PubMed] [Google Scholar]
- 19. Crandley EF, Hegarty SE, Hyslop T, Wilson DD, Dicker AP, Showalter TN. Treatment-related complications of radiation therapy after radical prostatectomy: comparative effectiveness of intensity-modulated versus conformal radiation therapy. Cancer Med. 2014;3: 397–405. 10.1002/cam4.205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hu JC, Gu X, Lipsitz SR, Barry MJ, D’Amico AV, Weinberg AC, et al. Comparative effectiveness of minimally invasive vs open radical prostatectomy. JAMA. 2009;302: 1557–1564. 10.1001/jama.2009.1451 [DOI] [PubMed] [Google Scholar]
- 21. Giordano SH, Lee A, Kuo Y-F, Freeman J, Goodwin JS. Late gastrointestinal toxicity after radiation for prostate cancer. Cancer. 2006;107: 423–432. [DOI] [PubMed] [Google Scholar]
- 22. Sheets NC, Goldein GH, Meyer A-M, Wu Y, Chang Y, Sturmer T, et al. Intensity-modulated radiation therapy, proton therapy, or conformal radiation therapy and morbidity and disease control in localized prostate cancer. JAMA. 2012;307: 1611–1620. 10.1001/jama.2012.460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bekelman JE, Mitra N, Efstathiou JA, Liao K, Sunderland R, Yeboa DN, et al. Outcomes after intensity-modulated versus conformal radiotherapy in older men with nonmetastatic prostate cancer. Int J Radiat Oncol Biol Phys. 2011;81: e325–e334. 10.1016/j.ijrobp.2011.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leslie S, Thiebaud P. SAS Global Forum 2007, Propensity scores to adjust for treatment selection bias. SAS Institute Inc. 2007;Paper 184.
- 25. D’Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17: 2265–2281. [DOI] [PubMed] [Google Scholar]
- 26.Atkinson EJ, Crowson CS, Pedersen RA, Therneau TM. Technical Report Series No. 81, Poisson models for person-years and expected rates. 2008;Rochester, Minnesota: Mayo Clinic.
- 27.Powell TM, Bagnell ME. SAS Global Forum 2012, Your “survival” guide to using time-dependent Covariates. SAS Institute Inc. 2012; Paper 168.
- 28. Valicenti RK, Thompson IJ, Albertsen P, Davis BJ, Goldenberg SL, Wolf JS, et al. Adjuvant and salvage radiation therapy after prostatectomy: American Society for Radiation Oncology/American Urological Association Guidelines. Int J Radiat Oncol Biol Phys. 2013;86: 822–828. 10.1016/j.ijrobp.2013.05.029 [DOI] [PubMed] [Google Scholar]
- 29. Mishra MV, Champ CE, Den RB, Scher ED, Shen X, Trabulsi EJ, et al. Postprostatectomy radiation therapy: an evidence-based review. Future Oncol. 2011;7: 1429–1440. 10.2217/fon.11.120 [DOI] [PubMed] [Google Scholar]
- 30. King CR, Kapp D. Radiotherapy after prostatectomy: Is the evidence for dose escalation out there? Int J Radiat Oncol Biol Phys. 2008;71: 346–350. 10.1016/j.ijrobp.2007.10.008 [DOI] [PubMed] [Google Scholar]
- 31. King CR, Spiotto MT. Improved outcomes with higher doses for salvage radiotherapy after prostatectomy. Int J Radiat Oncol Biol Phys. 2008;71: 23–27. 10.1016/j.ijrobp.2007.09.047 [DOI] [PubMed] [Google Scholar]
- 32. Bernard JR Jr, Buskirk SJ, Heckman MG, Diehl NN, Ko SJ, Macdonald OK, et al. Salvage radiotherapy for rising prostate-specific antigen levels after radical prostatectomy for prostate cancer: Dose-response analysis. Int J Radiat Oncol Biol Phys. 2010;76: 735–740. 10.1016/j.ijrobp.2009.02.049 [DOI] [PubMed] [Google Scholar]
- 33. Ohri N, Dicker AP, Trabulsi EJ, Shi W, Showalter TN. Can early implementation of salvage radiotherapy for prostate cancer improve the therapeutic ratio?: A systematic review and regression meta-analysis with radiobiological modeling. Eur J Cancer. 2012;48: 837–844. 10.1016/j.ejca.2011.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Virnig B, Warren JL, Cooper GS, Klabunde CN, Schussler N, Freeman J. Studying radiation therapy using SEER-Medicare-linked data. Med Care. 2002;40: IV–49–54. [DOI] [PubMed] [Google Scholar]
- 35. Potosky AL, Warren JL, Riedel ER, Klabunde CN, Earle CC, Begg CB. Measuring complications of cancer treatment using the SEER-Medicare data. Med Care. 2002;40: 62–68. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Text and explanatory tables pertinent to the analyses are included.
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
Data are from SEER-Medicare, a third party. Data requests will be reviewed by SEER-Medicare and will need to comply with SEER-Medicare data use agreement. Requests for data may be sent to SEER-Medicare from the US National Cancer Institute webpage, or by contacting Elaine Yanisko, Information Management Services, Inc., 3901 Calverton Blv, Suite 200, Calverton, MD 2070 (yaniskoe@imsweb.com).