Abstract
Background and objective
antipyretic therapy for patients with sepsis has long been debated. The present study aimed to explore the beneficial effect of antipyretic therapy for ICU patients with sepsis.
Design
systematic review and trial sequential analysis of randomized controlled trials.
Database
Pubmed, Scopus, EBSCO and EMBASE were searched from inception to August 5, 2014.
Methods
Mortality was dichotomized as binary outcome variable and odds ratio (OR) was chosen to be the summary statistic. Pooled OR was calculated by using DerSimonian and Laird method. Statistical heterogeneity was assessed by using the statistic I2. Trial sequential analysis was performed to account for the small number of trials and patients.
Main results
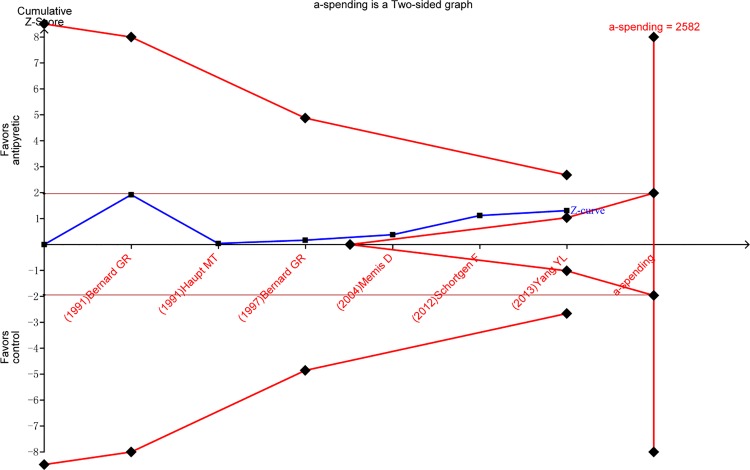
A total of 6 randomized controlled trials including 819 patients were included into final analysis. Overall, there was no beneficial effect of antipyretic therapy on mortality risk in patients with established sepsis (OR: 1.02, 95% CI: 0.50–2.05). The required information size (IS) was 2582 and our analysis has not yet reached half of the IS. The Z-curve did not cross the O’Brien-Fleming α-spending boundary or reach the futility, indicating that the non-significant result was probably due to lack of statistical power.
Conclusion
our study fails to identify any beneficial effect of antipyretic therapy on ICU patients with established diagnosis of sepsis. Due to limited number of total participants, more studies are needed to make a conclusive and reliable analysis.
Introduction
Fever is commonly seen in intensive care unit (ICU) patients and is often managed with antipyretics and external cooling.[1] Two primary causes of fever involve central nervous system and infection. The former is associated with the impairment of the central temperature regulation system (e.g. as those in patients with disorders of central nervous system or brain injury), and the latter involves inflammatory response to infectious agents. While therapeutic hypothermia has been proven to be beneficial for those caused by central nervous system, there is a great deal of controversy in the later condition.
Sepsis is defined as the systematic inflammatory response syndrome (SIRS) caused by suspected or documented infections, and it is often accompanied with fever. The management of fever induced by sepsis varies substantially across different institutions and hospitals.[2,3] Some clinicians believe that fever is potentially harmful because it increases oxygen consumption and further exacerbates the imbalance between oxygen supply and demand.[4] Therefore, they employ both antipyretic drugs and external cooling for fever control. With respect to the choice of methods for fever control, some investigators suggest that fever control with antipyretic drugs is potentially harmful because of the side effect of these drugs (e.g. hepatotoxicity of NSAIDS), and external cooling is preferable.[5] However, other investigators think that fever is a protective response elicited by human body to combat microorganisms and suppression of fever may delay the recovery.[6,7]Therefore they do not recommend routine use of fever control strategy in patients with sepsis.
There is no consensus on the management of fever in patients with sepsis. One systematic review has focused on the effect of antipyretic therapy on mortality in febrile ICU patients and the result was neutral.[8] The study population in that study is febrile ICU patients and the result may not be extrapolated to septic patients. Furthermore, new evidence has been published since that systematic review. Therefore, we conducted the systematic review and meta-analysis to investigate the effect of antipyretic therapy on mortality in patients with sepsis.
Methods
Study selection
Electronic databases including Pubmed, Scopus, EBSCO and EMBASE were searched from inception to August 5, 2014. The core search consisted terms related to sepsis and antipyretic therapy (“sepsis” or “septic” or “infection” AND “antipyretic” or “antipyretics” or “cooling” or “hypothermia”). The detailed searching strategy and the number of citations obtained from each database are listed in the appendix file (S1 Searching). There was no language restriction. References of reviews and relevant observational studies were searched by hand to identify potential relevant RCTs.
Studies to be included should meet the following criteria: 1) randomized controlled trial investigating the efficacy of antipyretic therapy; 2) study population was adult; 3) the medical condition included sepsis, severe sepsis or septic shock. Definition of sepsis should be explicitly made by the combination of SIRS and infection.[9,10] Studies investigating hypothermia in brain injury were excluded.
Data extraction
Data on the following information were extracted from included RCTs: the name of the first author, publication year, study population (sepsis, severe sepsis or septic shock), illness severity (reported by severity score such as APACHEII or SAPS), intervention (antipyretic medication or physical cooling), treatment period (how long did the intervention last), sample size, definition of mortality (the definition for primary outcome was chosen if a study reported more than one mortality), other study endpoints. For the calculation of pooled effect size, the numbers of subjects and events (e.g. death) in each arm were extracted.
Assessment of risk of bias
Risk of bias of each component studies were assessed by using Cochrane Collaboration Risk of Bias Tool.[11] The tool consisted of seven aspects corresponding to different components of RCT design.
Data synthesis
Mortality was dichotomized as binary outcome variable and odds ratio (OR) was chosen to be the summary statistic. Pooled OR was calculated by using a weighted average of the intervention effects estimated from individual studies. Because component studies included different septic patients in terms of illness severity, causes of sepsis, and infection site, we assumed that different studies estimated different, yet related, intervention effects. We performed random-effects meta-analysis by using DerSimonian and Laird method.[12] Statistical heterogeneity was assessed by using the statistic I2, which describes the percentage of the variability in effect estimates that is due to heterogeneity rather than sampling error (chance). An I2<30% indicates that the heterogeneity may not be important, and an I2>75% indicates considerable heterogeneity, and a value in between indicate moderate heterogeneity.[13]
Trial sequential analysis
Because meta-analysis containing a small number trials and a small number of patients is subject to spurious findings, we performed trial sequential analysis to adjust for the threshold for which results were considered statistically significant.[14] Information size was calculated by making the following assumptions: relative risk reduction was 20%; mortality rate in control arm was 30%; and the statistical power was 75%. Due to the heterogeneity of included trials, heterogeneity-adjustment factor was employed for information size calculation. O’Brien-Fleming α–spending function is used to adjust for Z-values, because it produced conservative boundaries at early stage where only a small amount of data has been collected.[15] Futility testing is performed by using β-spending function to explore whether the non-significance is due to lack of power or due to underlying equivalence between two arms.
Reporting bias
Publication bias was assessed by using Egger’s regression test, in which the standard normal deviate (the odds ratio divided by its standard error) is regressed against the estimates precision.[16] The intercept of the regression line is an estimate of asymmetry: the larger its deviation from origin the more significant asymmetry. Funnel asymmetry may be caused by publication bias or small study effect.
Subgroup analysis
It is plausible that intervention effect may be more pronounced in more severely ill patients, therefore subgroup analysis was performed by restricting subjects to septic shock. Treatment time period as defined by the time in which study protocol was performed was another potential determinant of effect size, thus subgroup analysis was performed by treatment time>48 or <48 hours. Subgroups using different antipyretic treatment (antipyretic medication vs. external cooling) were analyzed.
Results
Searching results and component trials
The initial search identified 104 citations and 84 of them were excluded by reviewing the titles and abstracts. The remaining 20 articles were clinical studies, in which six studies investigated hypothermia in patients with brain injury, three involved infants or children, and five were observational studies. As a result, a total of 6 randomized controlled trials were included into final analysis (Fig. 1).[17–22] Three studies[17–19] included patients with sepsis, one[20] included severe sepsis and the remaining two[21,22] included septic shock. Studies included sepsis and septic shock did not mean that they excluded patients with septic shock but the term “sepsis” covered severe sepsis and septic shock. Therefore, the proportions of septic shock were reported for four studies.[17–20] Severity of patients was presented by using APACHE score or SAPS-3. Three studies[17–19] used ibuprofen as the antipyretic medication and one[20] used lornoxicam for antipyretic therapy. The remaining two studies[21,22] employed external cooling. The study protocol lasted for less than 48 hours in four studies[17–19,21] and for 72 hours in the remaining two studies[20,22]. With respect to definition of mortality, two studies[17,19] used 30-day mortality. Other secondary outcomes were various including shock reversal, serum concentrations of ibuprofen, organ failure, duration of mechanical ventilation, vasopressor use and tissue perfusion parameters (Table 1).
Fig 1. Flowchart of study selection.
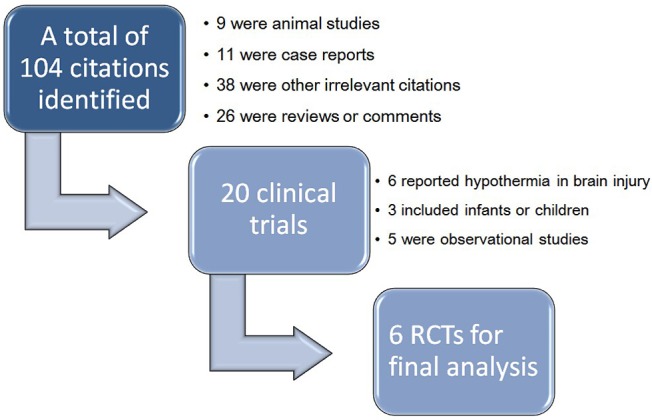
The initial search identified 402 citations after exclusion of duplicates. 382 of them were excluded by reviewing the titles and abstracts. The remaining 20 articles were clinical studies, in which six studies investigated hypothermia in patients with brain injury, three involved infants or children, and five were observational studies. As a result, a total of 6 randomized controlled trials were included into final analysis.
Table 1. Characteristics of included RCT studies.
| Studies | Study population | Shock (%; intervention vs control)† | Severity of illness† | Intervention | Treatment period | Sample size | Mortality | Other study endpoint |
|---|---|---|---|---|---|---|---|---|
| Bernard GR 1991[17] | Sepsis | 50 vs 36 | - | Ibuprofen | 12 hours | 30 | 30-day | Shock reversal; ibuprofen level |
| Haupt MT 1991[18] | Sepsis | 50 vs 31 | - | Ibuprofen | 22 hours | 29 | - | Concentration of ibuprofen |
| Bernard GR 1997[19] | Sepsis | 65 vs 63 | APACHEII: 16 vs 15 | Ibuprofen | 48 hours | 455 | 30-day | Organ-failure |
| Memiş D 2004[20] | Severe sepsis | 35 vs 40 | APACHEII: 17.1 vs 18 | lornoxicam | 72 hours | 40 | Hospital mortality | Mechanical ventilation |
| Schortgen F 2012[21] | Septic shock | All | SAPS-3: 77 vs 79 | External cooling | 48 hours | 200 | 14-day; | Vasopressor use; ICU mortality; hospital mortality |
| Yang YL 2013[22] | Septic shock | All | APACHEII: 23.8 vs 22 | External cooling | 72 hours | 65 | 28-day | Tissue perfusion |
Abbreviations: APACHEII, Acute Physiology and Chronic Health Evaluation II; ICU, intensive care unit; SAPS, Simplified Acute Physiology Score.
† Mean values were reported for the treatment and control arms, respectively
Assessment of risk of bias
Risks of bias were assessed using seven items corresponding to essential aspects of study design (Table 2). Random sequence generation was rated as low risk of bias in five studies[17–21] except for the study Yang YL 2013[22]. The allocation concealment was not explicitly reported in five studies[17–20,22]. Blinding of participants and outcome assessor was thought of low risk of bias because mortality was unlikely to be distorted by subjective sense. There was no selective reporting in most studies and no other risk of bias was thought to be present.
Table 2. Assessment of risk of bias†.
| Studies | Random sequence generation | Allocation concealment | Blinding of participants | Blinding of outcome assessor | Incomplete outcome data | Selective reporting | Other bias |
|---|---|---|---|---|---|---|---|
| Bernard GR 1991[17] | Low | Unclear | Low | Low | Low | Low | Low |
| Haupt MT 1991[18] | Low | Unclear | Low | Low | Low | Low | Low |
| Bernard GR 1997[19] | Low | Unclear | Low | Low | Low | Low | Low |
| Memiş D 2004[20] | Low | Unclear | Low | Low | Low | Unclear | Low |
| Schortgen F 2012[21] | Low | Low | Low | Low | Low | Low | Low |
| Yang YL 2013[22] | Unclear | Unclear | Low | Low | Low | Low | Low |
† Risk of bias were assessed according to the handbook of Cochrane. Each item was graded as “low”, “high” and “unclear”.
Evidence synthesis
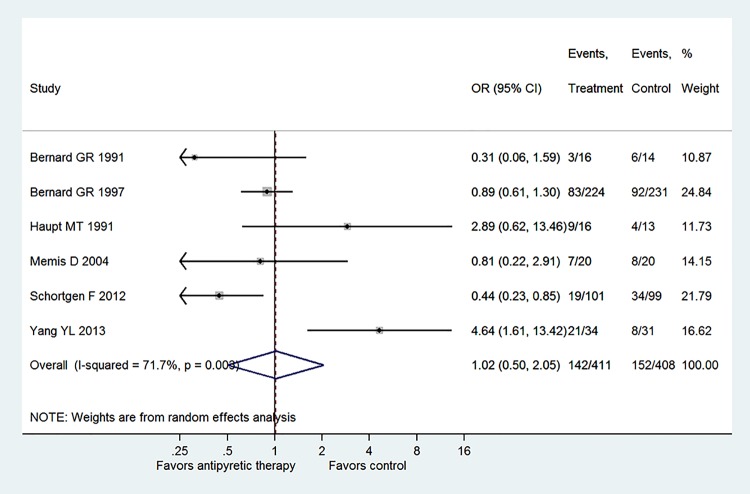
The six component trials included a total of 819 patients (Fig. 2). Only one study showed statistically beneficial effect of antipyretic therapy on mortality risk (OR: 0.44, 95% CI: 0.23–0.85), and other trials all showed neutral effect. There was significant heterogeneity among component trials as indicated by an I2 of 71.7% (p = 0.003). Overall, there was no beneficial effect of antipyretic therapy on mortality risk in patients with established sepsis (OR: 1.02, 95% CI: 0.50–2.05). The required information size (IS) was 2582 and our analysis has not yet reached half of the IS (Fig. 3). The Z-curve did not cross the O’Brien-Fleming α-spending boundary or reach the futility, indicating that the non-significant result was probably due to lack of statistical power.
Fig 2. Overall effect pooled across all included trials by using random-effects model.
Only one study showed statistically beneficial effect of antipyretic therapy on mortality risk (OR: 0.44, 95% CI: 0.23–0.85), and other trials all showed neutral effect. There was significant heterogeneity among component trials as indicated by an I2 of 71.7% (p = 0.003). A total of 819 patients were included in the meta-analysis, including 411 in the treatment group and 408 in the control group. Overall, there was no beneficial effect of antipyretic therapy on mortality risk in patients with established sepsis (OR: 1.02, 95% CI: 0.50–2.05).
Fig 3. Meta-analysis with repeated non-superiority, non-inferiority and two-sided significance testing boundaries.
The required information size (IS) was 2582 and our analysis has not yet reached half of the IS. The Z-curve did not cross the O’Brien-Fleming α-spending boundary or reach the futility, indicating that the non-significant result was probably due to lack of statistical power.
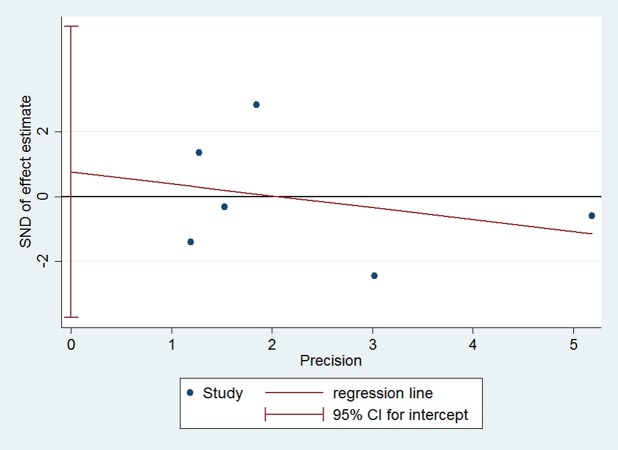
Publication bias
Publication bias was assessed by using Egger’s regression test (Fig. 4). The standard normal deviate (SND) is regressed against the estimates precision. The intercept of the regression line is 0.76 (95% CI: -3.74–5.25), indicating no statistically significant publication bias.
Fig 4. Publication bias was assessed by using Egger’s regression test.
The standard normal deviate (SND) is regressed against the estimates precision. The intercept of the regression line is 0.76 (95% CI: -3.74–5.25), indicating no statistically significant publication bias.
Subgroup analyses
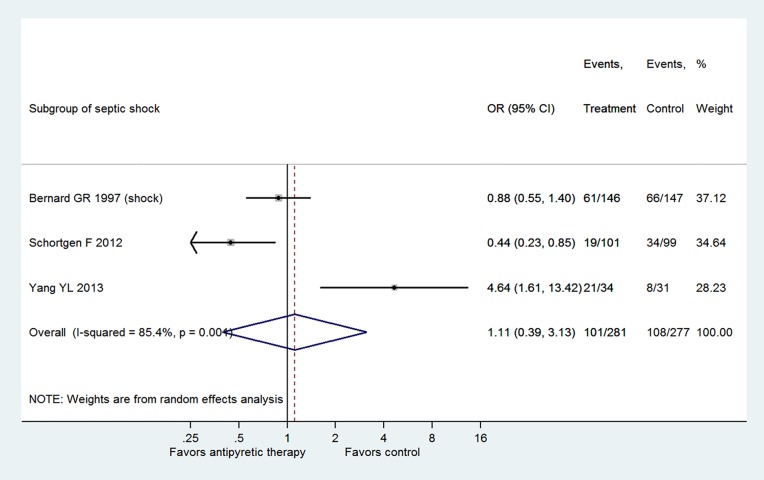
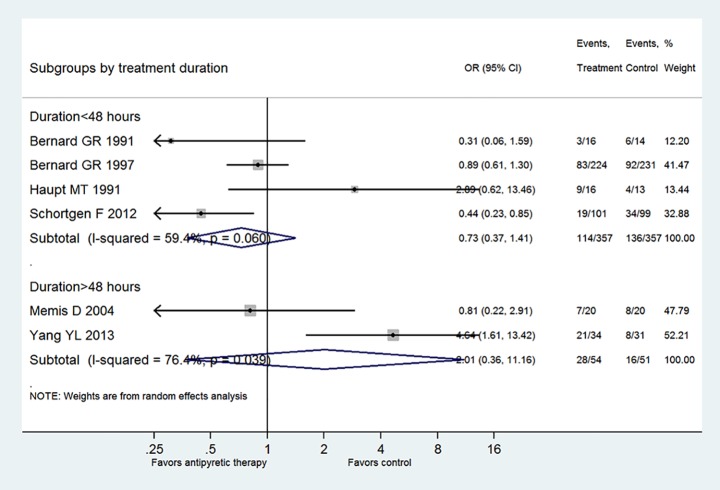
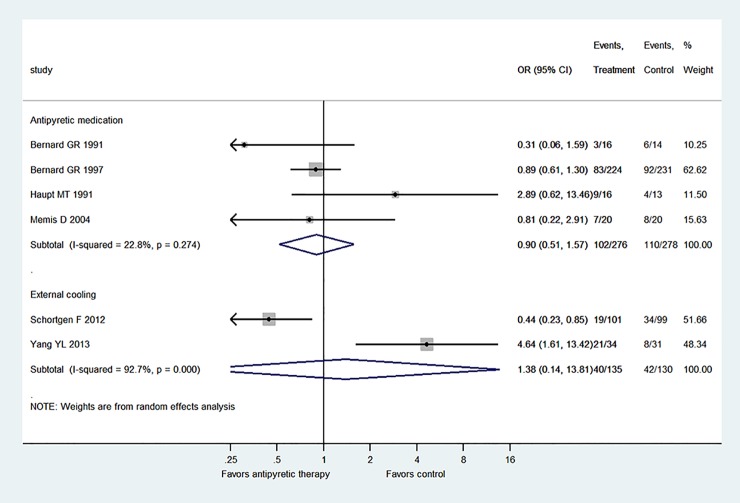
Fig. 5 shows the subgroup analysis by restricting to patients with septic shock. Three trials fulfilled this criterion and the result showed there was no beneficial effect of antipyretic therapy on reducing mortality rate (OR: 1.11, 95% CI: 0.39–3.13). Also, Fig. 6 displays the subgroup analysis stratified by the duration of antipyretic therapy. The result showed that there was no treatment effect with antipyretic therapy in neither the subgroup with treatment<48 hours (OR: 0.73, 95% CI: 0.37–1.41) nor the subgroup with treatment>48 hours (OR: 2.01, 95% CI: 0.36–11.16). Fig. 7 shows the subgroup analysis stratified by the mode of antipyretic therapy (antipyretic medication vs. external cooling). The result showed that there was no treatment effect with antipyretic therapy in neither the subgroup of antipyretic medication (OR: 0.90, 95% CI: 0.51–1.57) nor the subgroup of external cooling (OR: 1.38, 95% CI: 0.14–13.81).
Fig 5. Subgroup analysis by restricting to patients with septic shock.
Three trials fulfilled this criterion and the result showed there was no beneficial effect of antipyretic therapy on reducing mortality rate (OR: 1.11, 95% CI: 0.39–3.13).
Fig 6. Subgroup analysis stratified by the duration of antipyretic therapy.
The result showed that there was no treatment effect with antipyretic therapy in neither the subgroup with treatment<48 hours (OR: 0.73, 95% CI: 0.37–1.41) nor the subgroup with treatment>48 hours (OR: 2.01, 95% CI: 0.36–11.16).
Fig 7. Subgroup analysis stratified by the mode of antipyretic therapy (antipyretic medication vs. external cooling).
The result showed that there was no treatment effect with antipyretic therapy in neither the subgroup of antipyretic medication (OR: 0.90, 95% CI: 0.51–1.57) nor the subgroup of external cooling (OR: 1.38, 95% CI: 0.14–13.81).
Discussion
The study showed that antipyretic therapy was less likely to have beneficial effect for patients with established diagnosis of sepsis, and the result remained unchanged irrespective of the duration of treatment, mode of antipyretic therapy and shock status. However, the trial sequential analysis indicated that the null effect of the study was probably due to inadequate power as the Z-curve did not cross the futility line and the total sample size was less than half of the required information size. Therefore, future trials are still need to determine whether antipyretic therapy will be beneficial to septic patients.
One systematic review has been conducted by Niven DJ and coworkers,[8] in which critically ill patients with febrile were included as study population. Although this population included a large proportion of septic patient, it still differed from our study by including febrile patients that were not caused by infection. For instance, Niven’s systematic review included the study by Schulman CI that was conducted in trauma ICU and enrolled substantial number of patients of brain injury.[23] There is a large body of evidence suggesting potential beneficial effect of hyperthermia in inhibiting bacterial growth,[7,24,25] which has long been used as an argument against fever control in febrile patients with infection. This beneficial effect is not available in non-infectious febrile patients (e.g. fever caused by central nervous system), but the adverse effect of hyperthermia take predominance. The effect of antipyretic therapy for non-infectious febrile is less ambiguous,[26–28] but it is controversial in infectious febrile. Therefore, the present study aimed to solve this controversy. However, our study failed to identify any beneficial effect of antipyretic therapy in patients with sepsis, the same as that demonstrated by Niven DJ and coworkers.
The strength of the present study is that we employ trial sequential analysis, providing a better framework for the interpretation of the results. The meta-analysis included small number of population and small number of component trials, which is subject to random error and can cause spurious findings. Repeated update of meta-analysis involves a phenomenon commonly known as “multiplicity due to repeated significance testing”.[29] Required information size (number of patients) was calculated in our study and if this was reached, a reliable conclusion can be drawn from the meta-analysis. Unfortunately, the available evidence failed to reach half of the required information size. The solution to this problem is to use the α-spending function and trial sequential monitoring boundaries. The solution works to adjust the threshold for Z-value, allowing the type I error risk to restore the desired maximum risk.[30,31] The result of sequential trial analysis showed that the Z-curve did not cross the O’Brien-Fleming boundary, suggesting there was no evidence of benefits of the antipyretic therapy. Furthermore, the Z-curve did not cross the non-superiority boundary, indicating that the insignificance could be due to lack of statistical power.
In aggregate, our study failed to identify any beneficial effect of antipyretic therapy on ICU patients with established diagnosis of sepsis. Due to limited number of total participants, more studies are needed to make a conclusive and reliable analysis.
Supporting Information
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This author has no support or funding to report.
References
- 1. Young PJ, Saxena M (2014) Fever management in intensive care patients with infections. Critical Care 18: 206 10.1186/cc13773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cavaillon JM (2012) Good and bad fever. Crit Care 16: 119 10.1186/cc11237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Launey Y, Nesseler N, Malledant Y, Seguin P (2011) Clinical review: fever in septic ICU patients—friend or foe? Crit Care 15: 222 10.1186/cc10097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mohr NM, Doerschug KC (2013) Point: Should antipyretic therapy be given routinely to febrile patients in septic shock? Yes. Chest 144: 1096–1098; discussion 1101–1093. 10.1378/chest.13-0916 [DOI] [PubMed] [Google Scholar]
- 5. Dimopoulos G, Falagas ME (2009) Approach to the febrile patient in the ICU. Infect Dis Clin North Am 23: 471–484. 10.1016/j.idc.2009.04.001 [DOI] [PubMed] [Google Scholar]
- 6. Drewry AM, Hotchkiss RS (2013) Counterpoint: Should antipyretic therapy be given routinely to febrile patients in septic shock? No. Chest 144: 1098–1101; discussion 1101–1093. 10.1378/chest.13-0918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hasday JD, Fairchild KD, Shanholtz C (2000) The role of fever in the infected host. Microbes Infect 2: 1891–1904. [DOI] [PubMed] [Google Scholar]
- 8. Niven DJ, Stelfox HT, Laupland KB (2013) Antipyretic therapy in febrile critically ill adults: A systematic review and meta-analysis. J Crit Care 28: 303–310. 10.1016/j.jcrc.2012.09.009 [DOI] [PubMed] [Google Scholar]
- 9. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, et al. (2013) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 41: 580–637. 10.1097/CCM.0b013e31827e83af [DOI] [PubMed] [Google Scholar]
- 10. Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, et al. (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31: 1250–1256. [DOI] [PubMed] [Google Scholar]
- 11. Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG (2012) Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. Journal of Evaluation in Clinical Practice 18: 12–18. 10.1111/j.1365-2753.2010.01516.x [DOI] [PubMed] [Google Scholar]
- 12. DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Controlled Clinical Trials 7: 177–188. [DOI] [PubMed] [Google Scholar]
- 13. Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pogue JM, Yusuf S (1997) Cumulating evidence from randomized trials: Utilizing sequential monitoring boundaries for cumulative meta-analysis. Controlled Clinical Trials 18: 580–593. [DOI] [PubMed] [Google Scholar]
- 15. Thorlund K, Devereaux PJ, Wetterslev J, Guyatt G, Ioannidis JPA, et al. (2008) Can trial sequential monitoring boundaries reduce spurious inferences from meta-analyses? International Journal of Epidemiology 38: 276–286. 10.1093/ije/dyn179 [DOI] [PubMed] [Google Scholar]
- 16. Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bernard GR, Reines HD, Halushka PV, Higgins SB, Metz CA, et al. (1991) Prostacyclin and thromboxane A2 formation is increased in human sepsis syndrome. Effects of cyclooxygenase inhibition. Am Rev Respir Dis 144: 1095–1101. [DOI] [PubMed] [Google Scholar]
- 18. Haupt MT, Jastremski MS, Clemmer TP, Metz CA, Goris GB (1991) Effect of ibuprofen in patients with severe sepsis: a randomized, double-blind, multicenter study. The Ibuprofen Study Group. Crit Care Med 19: 1339–1347. [DOI] [PubMed] [Google Scholar]
- 19. Bernard GR, Wheeler AP, Russell JA, Schein R, Summer WR, et al. (1997) The Effects of Ibuprofen on the Physiology and Survival of Patients with Sepsis. New England Journal of Medicine 336: 912–918. [DOI] [PubMed] [Google Scholar]
- 20. Memiş D, Karamanlıoğlu B, Turan A, Koyuncu O, Pamukçu Z (2004) Effects of lornoxicam on the physiology of severe sepsis. Critical Care 8: R474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schortgen F, Clabault K, Katsahian S, Devaquet J, Mercat A, et al. (2012) Fever control using external cooling in septic shock: a randomized controlled trial. Am J Respir Crit Care Med 185: 1088–1095. 10.1164/rccm.201110-1820OC [DOI] [PubMed] [Google Scholar]
- 22. Yang YL, Liu DW, Wang XT, Long Y, Zhou X, et al. (2013) Body temperature control in patients with refractory septic shock: too much may be harmful. Chin Med J (Engl) 126: 1809–1813. [PubMed] [Google Scholar]
- 23. Schulman CI, Namias N, Doherty J, Manning RJ, Li P, et al. (2005) The effect of antipyretic therapy upon outcomes in critically ill patients: a randomized, prospective study. Surg Infect (Larchmt) 6: 369–375. [DOI] [PubMed] [Google Scholar]
- 24. Graham NM, Burrell CJ, Douglas RM, Debelle P, Davies L (1990) Adverse effects of aspirin, acetaminophen, and ibuprofen on immune function, viral shedding, and clinical status in rhinovirus-infected volunteers. J Infect Dis 162: 1277–1282. [DOI] [PubMed] [Google Scholar]
- 25. Kluger MJ, Kozak W, Conn CA, Leon LR, Soszynski D (1996) The adaptive value of fever. Infect Dis Clin North Am 10: 1–20. [DOI] [PubMed] [Google Scholar]
- 26. Schmutzhard E, Engelhardt K, Beer R, Brossner G, Pfausler B, et al. (2002) Safety and efficacy of a novel intravascular cooling device to control body temperature in neurologic intensive care patients: a prospective pilot study. Crit Care Med 30: 2481–2488. [DOI] [PubMed] [Google Scholar]
- 27. Sahuquillo J, Perez-Barcena J, Biestro A, Zavala E, Merino MA, et al. (2009) Intravascular cooling for rapid induction of moderate hypothermia in severely head-injured patients: results of a multicenter study (IntraCool). Intensive Care Med 35: 890–898. 10.1007/s00134-008-1357-4 [DOI] [PubMed] [Google Scholar]
- 28. Clifton GL, Allen S, Barrodale P, Plenger P, Berry J, et al. (1993) A phase II study of moderate hypothermia in severe brain injury. J Neurotrauma 10: 263–271; discussion 273. [DOI] [PubMed] [Google Scholar]
- 29. Borm GF, Donders AR (2009) Updating meta-analyses leads to larger type I errors than publication bias. J Clin Epidemiol 62: 825–830 e810. 10.1016/j.jclinepi.2008.08.010 [DOI] [PubMed] [Google Scholar]
- 30. Wetterslev J, Thorlund K, Brok J, Gluud C (2008) Trial sequential analysis may establish when firm evidence is reached in cumulative meta-analysis. J Clin Epidemiol 61: 64–75. [DOI] [PubMed] [Google Scholar]
- 31. Pogue J, Yusuf S (1998) Overcoming the limitations of current meta-analysis of randomised controlled trials. Lancet 351: 47–52. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.