Abstract
We describe a case of a 59-year-old woman with a medical history of upper leg pain and chronic lymphatic leucaemia (CLL), with known diffuse bone marrow infiltration and without signs of lymphatic or extra-lymphatic disease activity on positron emission tomography CT (PET-CT). She presented with multiple fractures of the pelvis, sacrum and left proximal femur as a result of a low energy fall. During admission, she sustained a non-traumatic fracture of the right proximal femur. Pathological fractures in patients with CLL are usually based on Richter’s transformation or multiple myeloma. However, in the current case, a PET-CT and a bone marrow biopsy showed no signs of this. We did see a normoparathyroid hypercalcaemia in our patient, most likely caused by a CLL-based release of local osteoclast stimulating factors. A combination of fludarabine/cyclofosfamide/rituximab was started as treatment in combination with allopurinol and sodium bicarbonate to prevent further osteolysis.
Background
There are only a few known cases of pathological fractures in chronic lymphatic leucaemia, almost all based on Richter's transformation or multiple myeloma.1 2 This case presents a patient with pathological fractures and CLL without Richter's transformation or multiple myeloma and with no signs of disease activity on a positron emission tomography CT (PET-CT scan).
Case presentation
A 59-year-old woman with a medical history of upper leg pain and chronic lymphatic leucaemia, presented with peripheral lymphocytosis and known diffuse bone marrow infiltration but without signs of lymphatic or extra-lymphatic disease activity on PET-CT (figure 1). No treatment had been started for the CLL. She had multiple fractures of the pelvis, sacrum and left proximal femur as a result of a low energy fall (figure 2A). During admission, she sustained a non-traumatic fracture of the right proximal femur (figure 2B).
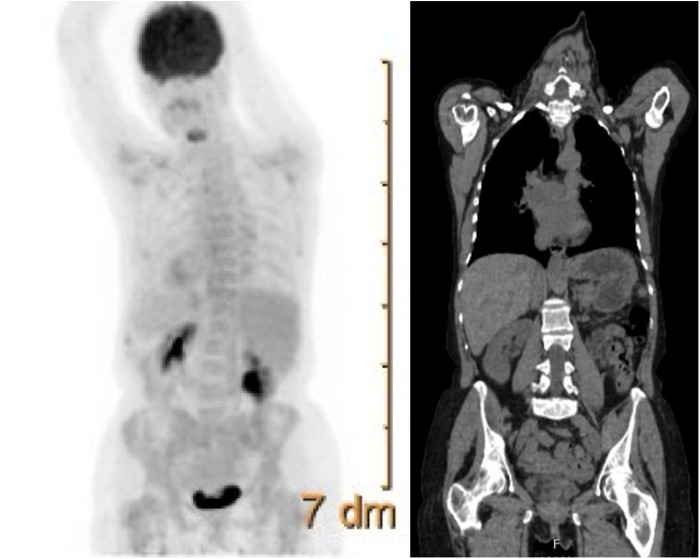
Figure 1.
Positron emission tomography-CT scan, showing diffuse bone marrow infiltration and without signs of lymphatic or extralymphatic disease activity.
Figure 2.
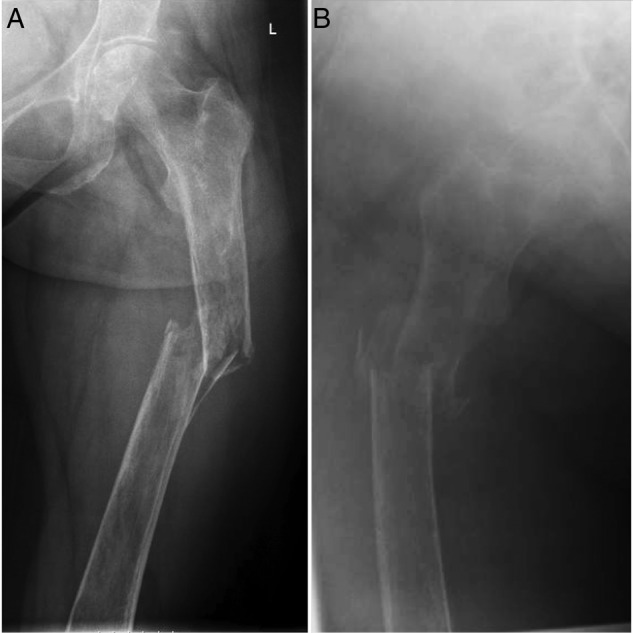
Anteroposterior view on conventional X-ray showing fracture of (A) the left femur and (B) the right femur.
Investigations
Bone marrow samples taken at the site of the fractures showed a localisation of chronic lymphatic leucaemia without signs of disease progression, Richter's transformation or multiple myeloma (figure 3A). The tumour cells showed a positive reaction with B-cell markers, including coexpression of CD5 and CD23. Cyclin D1 and BCL-6 were negative, and BCL-2 was positive. MUM1 stain showed expression in proliferation centres. Reactive T cells expressed both CD2 and CD3. There was no increase in Ki-67. There was no increase in the amount of prolymphocytes (figure 3B–D). The lesion predominantly showed expression of ZAP-70 of the B cells.
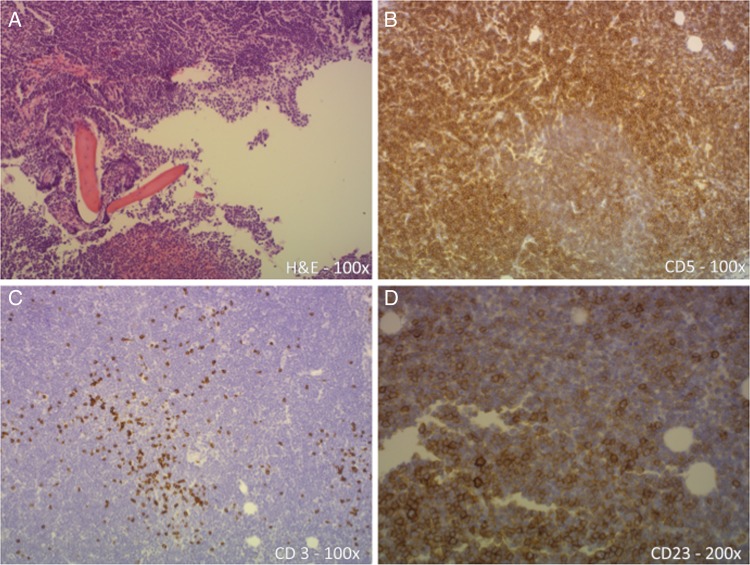
Figure 3.
Overview of pathology specimens: The H&E staining shows the trabeculae (A), surrounded by lymphocytic tumour cells, which completely infiltrate the original bone-marrow compartment. The CD5 staining shows diffuse positivity of all lymphoid cells (B), whereas the CD3 only accentuates the presence of a few reactive T cells (C). The majority of the CD5 positive lymphocytes are CD3 negative, indicating a neoplastic lymphoid infiltrate with aberrant expression of antigens. The CD23 staining is also diffusely positive (D), which in combination with positivity of CD5 and CD20 and the histomorphology is strongly compatible with CLL.
Treatment
The fracture of the left femur was treated by means of closed reduction and internal fixation using an Unreamed Femur Nail (UFN; Synthes GmbH, Zuchwil, Switzerland). The fracture of the right femur was treated by means of closed reduction and internal fixation using a Proximal Femur Nail (PFN-A; Synthes GmbH, Zuchwil, Switzerland). Multiple fractures of the ilium and sacrum were treated conservatively. Radiotherapy was considered, but regarded as likely ineffective, considering the presence of severe osteoporosis. Parathyroid hormone-related protein-associated hyperparathyroidism was excluded as a cause for osteoporosis (PTH-like protein <0.3 pmol/L) and the patient did not have a history of treatment with steroids.
The patient was subsequently treated with six cycles of intravenous rituximab with cyclophosphamide and oral fludarabine. To prevent further osteolysis, the patient was treated with allopurinol and sodium bicarbonate. Zoledronic acid was administered to treat the persisting hypercalcaemia.
Outcome and follow-up
The fractures in the pelvis showed consolidation in three out of four fractures after 6 months (figure 4A). Both femoral fractures showed proper consolidation after 6 months (figure 4B, C), though the right leg remained 2 cm shorter than the left leg. Owing to persisting pancytopenia following chemotherapy, another bone marrow biopsy was performed. This showed dysplastic changes matching reactive bone marrow, attributed to use of zoledronic acid, which has since been stopped.
Figure 4.
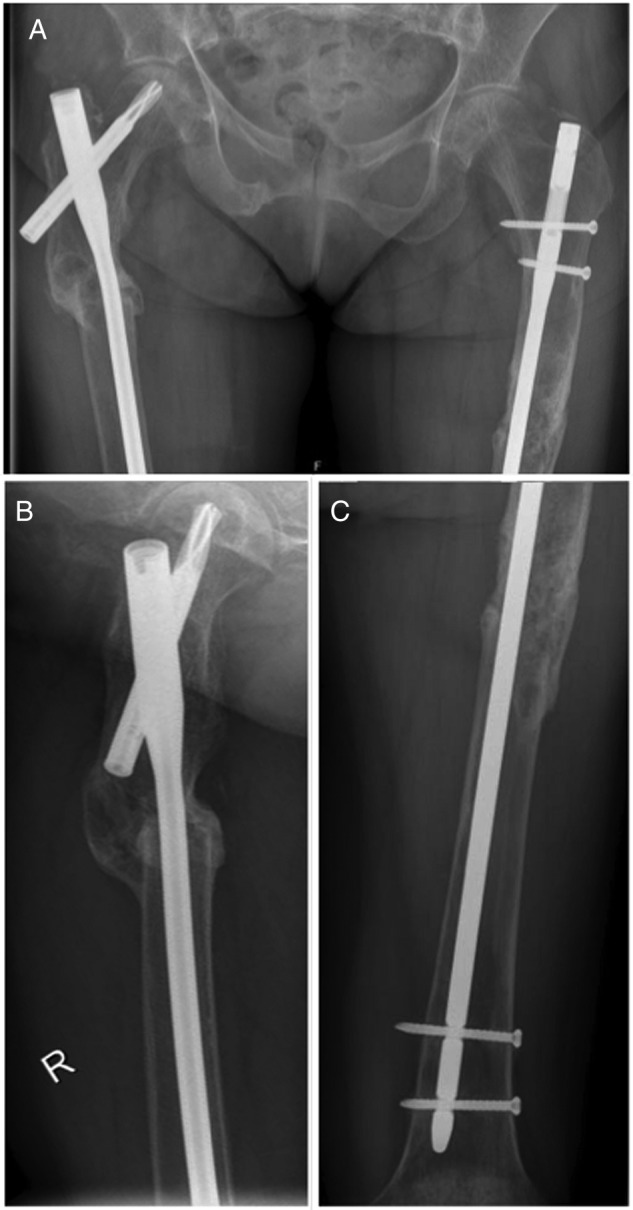
Follow-up images after 6 months, showing consolidation in three out of four pelvic fractures (A) and both femora (B, C).
The hypercalcaemia resolved after treatment with FCR and zoledronic acid, and ongoing oral calcium supplements. Bone densitometry revealed 30% improvement after 3 months of treatment.
Discussion
CLL is the most common leucaemia in western countries, with an incidence rate of 10 cases per 100 000 population per year.3 In chronic leucaemia, bony involvement is rare, while it is often seen in acute leucaemias,4 where it is known to affect, in order of frequency, the femurs, the humerus, the pelvis, the skull, the metacarpals, the ulna and the vertebrae.5
The metastatic spread of CLL to the bone resulting in pathological fractures is extremely rare,6 and has been reported in only a few cases.1–3 7 In most of these reported cases the CLL had progressed to Richter's syndrome1 or multiple myeloma.2
Since hypercalcaemia is seen in most known cases of pathological fractures in CLL, it has been postulated that these osteolytic fractures may be caused by osteoclast-activating factor (interleukin-1α).3 This idea is supported by a similar case in which histological examination of material from the fracture site showed high concentrations of osteoclasts.7
Furthermore, hypercalcaemia in patients with CLL and pathological fractures is correlated with a late stage of disease, and is a poor prognostic sign.6
The current case is unique, because there is no sign of progression to Richter's transformation or multiple myeloma, and no signs of disease activity on PET-CT scan. Also, the pathological fractures showed signs of consolidation as soon as 6 weeks after occurring. This is very early, taking into account the osteolytic nature of the lesions as well as the presence of severe osteoporosis, and has been accredited to treatment with allopurinol and sodium bicarbonate.
Owing to the present pancytopenia it could be argued that the disease should be classified as small lymphocyte lymphoma rather than CLL, but since the pancytopenia did not show until after FCR-therapy was started, combined with the absence of signs of lymphatic or extralymphatic disease activity, it was concluded that the disease should indeed be classified as CLL.
Considering our patient had many poor prognostic signs, including hypercalcaemia and pancytopenia as a result of chemotherapy, she responded very well to therapy with rituximab, cyclophosphamide, fludarabine 40 mg/m2 and zoledronate, and is remarkably still alive, more than a year after the reported events.
Learning points.
Pathological fractures, however rare, may be the initial presenting sign of chronic lymphatic leucaemia (CLL).
Pathological fractures can occur in patients with CLL even without disease progression or Richter's transformation.
Pathological fractures in patients with CLL may respond well to treatment with allopurinol and sodium bicarbonate to improve fracture consolidation.
Hypercalcaemia is present in most known cases of pathological fractures in CLL and is considered an indicator for poor prognosis.
Acknowledgments
The authors would like to acknowledge the help of W den Hartog MD and M de Gast of the Department of Pathology for their help with the pathology images.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Robak T, Kasznicki M, Bartkowiak J et al. Richter's syndrome following cladribine therapy for chronic lymphocytic leukemia first manifested at pathologic fracture of the femur. Leuk Lymphoma 2010;42;789–96. 10.3109/10428190109099341 [DOI] [PubMed] [Google Scholar]
- 2.Kough RH, Makary AZ. Chronic lymphocytic leukemia (CLL) terminating in multiple myeloma: report of two cases. Blood 1978;52:532–6. [PubMed] [Google Scholar]
- 3.Wright B, Wiesenfeld D, Seymour J. Bilateral fracture of the mandible in chronic lymphocytic leukaemia. Case report. Aust Dent J 1997;42:20–4. 10.1111/j.1834-7819.1997.tb00091.x [DOI] [PubMed] [Google Scholar]
- 4.Ducassou S, Ferlay C, Bergeron C et al. Clinical presentation, evolution, and prognosis of precursor B-cell lymphoblastic lymphoma in trials LMT96, EORTC 58881, and EORTC 58951. Br J Haematol 2011;152:441 10.1111/j.1365-2141.2010.08541.x [DOI] [PubMed] [Google Scholar]
- 5.Osgood EE. Monocytic leukaemia. Arch Int Med 1937;59:931 10.1001/archinte.1937.00170220007001 [DOI] [Google Scholar]
- 6.Abroud SL, Godeuk V, Schacter LP et al. Well-differentiated lymphocytic lymphoma with blood involvement, osteolytic bone lesions, and hypercalcaemia. Cancer 1985;56:2508–11. [DOI] [PubMed] [Google Scholar]
- 7.McMillan P, Mundy G, Mayer P, Hypercalcemia and osteolytic bone lesions in chronic lymphocytic leukaemia. BMJ 1980;281:1107 10.1136/bmj.281.6248.1107 [DOI] [PMC free article] [PubMed] [Google Scholar]