Abstract
Introduction:
With a focus on protecting vulnerable groups from initiating and continuing tobacco use, the FDA has been considering the regulation of menthol in cigarettes. Using a large sample of adult smokers with serious mental illness (SMI) in the San Francisco Bay Area, we examined demographic and clinical correlates of menthol use, and we compared the prevalence of menthol use among our study participants to that of adult smokers in the general population in California.
Methods:
Adult smokers with SMI (N = 1,042) were recruited from 7 acute inpatient psychiatric units in the San Francisco Bay Area. Demographic, tobacco, and clinical correlates of menthol use were examined with bivariate and multivariate logistic regression analyses, and prevalence of menthol use was compared within racial/ethnic groups to California population estimates from the 2008–2011 National Survey on Drug Use and Health.
Results:
A sample majority (57%) reported smoking menthol cigarettes. Multivariate logistic regression analyses indicated that adult smokers with SMI who were younger, who had racial/ethnic minority status, who had fewer perceived interpersonal problems, and who had greater psychotic symptoms also had a significantly greater likelihood of menthol use. Smokers with SMI had a higher prevalence of menthol use relative to the general population in California overall (24%).
Conclusions:
Individuals with SMI—particularly those who are younger, have racial/ethnic minority status, and have been diagnosed with a psychotic disorder—are vulnerable to menthol cigarette use. FDA regulation of menthol may prevent initiation and may encourage cessation among smokers with SMI.
Introduction
Tobacco use among persons with mental illness is a major public health concern. It is estimated that persons with psychiatric or addictive disorders consume nearly half the cigarettes sold in the United States, and are 2 to 4 times more likely than those in the general population to smoke.1,2 In particular, those with serious mental illness (SMI) suffer disproportionately from tobacco-related diseases and are dying, on average, 25 years prematurely.3 More targeted prevention and intervention strategies are critically needed to address the burden of tobacco-related consequences in this vulnerable group.4
Of recent interest and attention is consideration of tobacco control regulation to address menthol as a flavoring in cigarettes. Approximately 27% of all cigarettes sold nationally are menthol5 and adverse health effects of menthol cigarettes are documented.5 Menthol cigarettes have been aggressively marketed to disproportionately impacted groups, including Black Americans, Native Hawaiians, adolescents, and low-income communities6–8 and cost less than regular cigarettes within these communities.9 Research has documented higher menthol smoking among certain groups, including women, racial/ethnic minorities, young adults, those with less education and income, unmarried individuals, and lighter smokers.10–14
A 2013 report issued by the U.S. Food and Drug Administration (FDA) indicated that menthol cigarette use is associated with a greater likelihood of smoking initiation among youth as well as greater addiction, and a lower likelihood of successful quitting.15 With a focus on protecting at-risk groups from initiating and continuing tobacco use, the FDA has been considering whether regulation of menthol in cigarettes should be consistent with the ban on other flavorings, as mandated in the Family Smoking Prevention and Tobacco Control Act.16 From a public health perspective, if smokers with SMI have elevated menthol smoking relative to the general population, this finding would have significant policy implications, signifying another vulnerable group that may be less likely to initiate smoking, and more likely to quit smoking, if the FDA adds menthol to its ban on characterizing flavorings.
Surprisingly, despite the public health relevance of menthol cigarettes and the elevated prevalence of smoking by people with mental health problems, limited investigation has examined their intersection. Two epidemiologic studies and one clinical investigation reported on associations between menthol use and mental distress. Data analyzed from Florida’s Behavioral Risk Factor Surveillance System found menthol smokers had more days of poor mental health in the past month than nonmenthol smokers.14 In a national sample, menthol use was more likely among smokers with severe psychological distress compared to smokers with none or mild distress.17 In a study with 83 smokers diagnosed with schizophrenia and 53 control smokers,18 menthol cigarette smoking was more common among non-Hispanic Caucasians diagnosed with schizophrenia relative to non-Hispanic Caucasians without mental illness. Studies have not examined the prevalence of menthol use in a large clinical sample of adult smokers representing a range of psychiatric disorders.
The current study, examining the prevalence and correlates of menthol use among adult smokers with SMI, aimed to: (a) Identify sociodemographic, tobacco, and mental health factors associated with menthol use and (b) Examine whether menthol smoking prevalence is higher among smokers with SMI overall and among different racial/ethnic groups relative to adult smokers in the general population in California. Given preliminary findings reported in the literature, we hypothesized that menthol use would be more common among racial/ethnic minorities, younger adults, and smokers with greater psychiatric severity and that the prevalence of menthol use among adult smokers with SMI would be higher relative to smokers in the general population.
Methods
Study Participants and Setting
We pooled secondary data from baseline interviews with 1,042 men and women, all current smokers with SMI, recruited as inpatients from psychiatric hospitals in the San Francisco Bay Area between 2008 and 2013, for two clinical tobacco treatment trials. The recruitment sites were all acute care, short-stay, psychiatric units with complete smoking bans. The units were located in two academic, one community, and one public hospital. The smoking cessation intervention components were of the same design across the three trials and included a transtheoretical model-tailored computer-assisted intervention, a stage-matched manual, motivational enhancement and cognitive behavioral counseling tailored to the smokers’ stage of change, combined with nicotine replacement therapy (NRT).19,20 Participants were not recruited as motivated to quit smoking and recruitment rates were high in all three trials (69%–79%).
Eligibility included smoking at least five cigarettes per day (CPD) prior to hospitalization and at least 100 cigarettes in their lifetime, given the studies’ provision of NRT. Other inclusion criteria for all trials included plans to reside in the San Francisco Bay Area during the study period, fluency in written and spoken English, and demonstrated capacity to consent. Acutely psychotic, manic, or hostile patients with symptoms that did not resolve sufficiently during hospitalization and those with contraindication for NRT use, such as recent myocardial infarction, were excluded and provided alternative cessation treatment referrals. The Institutional Review Boards at the University of California, San Francisco; Stanford University; and the participating community hospitals approved of the study procedures, and participants provided informed consent.
Measures
Smoking Characteristics
In all three clinical trials, menthol smoking was assessed with the question, “Do you smoke menthol cigarettes?,” coded as “menthol smoker,” “nonmenthol smoker,” or “smokes both.” Consistent with prior population-level studies (including the NSDUH) and tobacco treatment trials, persons who responded menthol smoker or smokes both were categorized as “menthol smokers”.10,21 Cigarettes per day (CPD) were assessed by the question, “How many cigarettes do you usually smoke in a day?” Nicotine dependence was assessed using the 6-item Fagerström Test of Nicotine Dependence (FTND).22 Readiness to stop smoking was categorized into one of three stages of change: Precontemplation (no intention to quit in the next six months), Contemplation (intending to quit in the next six months), or Preparation (intention to quit in the next 30 days and with a 24-hour quit attempt in the past year).23
Mental Health Functioning
Psychiatric diagnoses of unipolar depression, bipolar disorder, and non-affective psychotic disorder were obtained using the computerized version of the Mini-International Neuropsychiatric Interview (eMINI)24 or by chart review. The eMINI is a brief structured psychiatric interview that screens mental disorders using criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV).25 The BASIS-24 assessed self-reported mental health functioning for the week prior to hospitalization; with subscale scores for depression/functioning, emotional lability, psychotic symptoms, and alcohol/drug use.26 The Medical Outcomes Short Form (SF-12) assessed physical and mental health functioning.27
Sociodemographic Variables
Sociodemographic factors known to be associated with menthol cigarette use in the general population were examined in the current study and included gender (categorized as male, female); race/ethnicity (Hispanic, non-Hispanic Caucasian, Black, Native Hawaiian/Pacific Islander/Asian American, and multiracial/other), years of education (range: no formal education [0 years] to doctoral degree [21 years]); income (categorized as < $10,000, $10,000-$19,999, $20,000-$39,999, $40,000 or more); and marital status (categorized as never married; divorced, separated, or widowed; married). Transgender individuals were excluded due to the small sample size (11 individuals).
NSDUH Comparison Data
Population menthol smoking prevalence estimates among adults in the general population were obtained from the 2008 to 2011 administrations of the National Survey on Drug Use and Health (NSDUH), an annual in-person interview that assesses a cross-section of individuals aged 12 and older for tobacco, alcohol, and illicit drug use, and mental health status.13,28,29 Data for the current comparative analyses were from adult smokers, 18 years and older, residing in California, who were assessed for menthol use (weighted N = 10,542). The NSDUH assessed menthol smoking among past month cigarette smokers in each administration using the question, “Were the cigarettes you smoked during the past 30 days menthol?”
Data Analysis
Descriptive analyses of sociodemographic, smoking-related, and mental health functioning measures were run to characterize our sample. Bivariate logistic regression analyses were conducted to examine how sociodemographic and smoking-related characteristics related to menthol smoking. Next, multivariate logistic regression analyses were conducted that simultaneously included sociodemographic characteristics, smoking-related variables, and mental health problems that were significantly associated with menthol smoking in bivariate analyses. The Asian American and Pacific Islander ethnic groups, and the American Indian and multiracial/other ethnic groups, were combined in the logistic regression models due to the small sample sizes of Pacific Islanders (n = 10) and American Indians (n = 20). Data were analyzed using SAS version 9.3.30 Lastly, the prevalence of menthol smoking was calculated by race/ethnicity for our sample of smokers with SMI and compared to NSDUH population estimates among smokers aged 18 and older residing in California.12,13,17,28
Results
Table 1 presents descriptive statistics for demographic variables, tobacco characteristics, and clinical characteristics by menthol use, along with results from bivariate multiple regression analyses examining differences by menthol cigarette use. Participants with SMI had a mean age of 39 years (SD = 13); averaged 13.5 years of education (SD = 2.8); 57% were never married, 27% were divorced, widowed, or separated, and 16% were married; and 51% had an annual household income < $10,000. The racial/ethnic composition was 48% non-Hispanic Caucasian, 23% Black, 15% Hispanic Caucasian, 5% Asian/Pacific Islander, and 9% multiracial/other. Primary psychiatric disorders were psychotic disorder (28%), bipolar disorder (30%), major depression (28%), and other (13%). The sample reported 43% nonmenthol use only, 28% menthol use only, and 29% both menthol and nonmenthol use.
Table 1.
Results From Bivariate Logistic Regression Predicting Current Menthol Smoking From Demographic, Tobacco, and Clinical Characteristics Among Smokers With Serious Mental Illness
| All N = 1,042 | Menthol smokers (n = 595) | Non-menthol smokers (n = 447) | OR a (95% CI) | p | |
|---|---|---|---|---|---|
| % or mean (SD) | % or mean (SD) | % or mean (SD) | |||
| Demographic characteristics | |||||
| Sex | |||||
| Male | 52.4 | 50.5 | 55.0 | 0.83 (0.65, 1.06) | .14 |
| Female | 47.6 | 49.5 | 45.0 | Reference | |
| Age | 38.9 (13.4) | 37.6 (13.3) | 40.5 (13.2) | 0.98 (0.98, 0.99) | .0005 |
| Race/ethnicity | |||||
| Black | 22.9 | 32.3 | 10.7 | 5.48 (3.81, 7.87) | <.0001 |
| Hispanic | 15.0 | 16.8 | 12.5 | 2.46 (1.69, 3.57) | <.0001 |
| Asian/Pacific Islander | 5.3 | 5.7 | 4.7 | 2.23 (1.26, 3.95) | .006 |
| Multiracial/other | 8.9 | 10.1 | 7.4 | 2.50 (1.58, 3.97) | <.0001 |
| White | 47.9 | 35.0 | 64.7 | Reference | |
| Years of education | 13.5 (2.8) | 13.2 (2.9) | 13.9 (2.6) | 0.91 (0.87, 0.95) | <.0001 |
| Income | |||||
| < $10,000 | 50.7 | 53.9 | 46.4 | 1.43 (1.05, 1.95) | .02 |
| $10,000–$20,999 | 24.9 | 23.8 | 26.2 | 1.13 (0.79, 1.62) | .70 |
| $21,000 or more | 24.4 | 22.2 | 27.4 | Reference | |
| Marital status | |||||
| Never married | 56.9 | 58.7 | 54.6 | 1.11 (.78, 1.57) | .25 |
| Divorced/separated/widowed | 27.4 | 25.8 | 29.4 | 0.91 (.62, 1.34) | .33 |
| Married/live with partner | 15.7 | 15.5 | 16.0 | Reference | |
| Smoking characteristics | |||||
| Usual cigarettes per day | 17.0 (10.7) | 17.0 (11.5) | 17.0 (9.60) | 1.00 (.99, 1.01) | .98 |
| FTND total score | 4.7 (2.2) | 4.76 (2.2) | 4.65 (2.24) | 1.02 (0.97, 1.08) | .43 |
| Smoke ≤ 30min of waking | 78.7 | 80.5 | 76.2 | 1.29 (0.96, 1.74) | .09 |
| Stage of change | |||||
| Precontemplation | 30.1 | 31.1 | 28.9 | 0.99 (0.71, 1.40) | .57 |
| Contemplation | 46.3 | 44.5 | 48.5 | 0.85 (0.62, 1.16) | .20 |
| Preparation | 23.6 | 24.4 | 22.6 | Reference | |
| Clinical characteristics | |||||
| Primary psychiatric diagnosis | |||||
| Psychotic disorder | 28.4 | 31.1 | 24.8 | 1.62 (1.17, 2.25) | .004 |
| Bipolar disorder | 29.9 | 29.4 | 30.7 | 1.24 (0.90, 1.71) | .18 |
| Other | 13.4 | 14.5 | 12.1 | 1.55 (1.03, 2.34) | .04 |
| Major depression | 28.2 | 25.0 | 32.4 | Reference | |
| CES-D-10 scoreb | 18.1 (7.7) | 17.5 (7.8) | 19.0 (7.5) | 0.98 (0.96, 0.99) | .003 |
| BASIS-24 scoresc | |||||
| Depression functioning | 2.5 (1.1) | 2.4 (1.1) | 2.6 (1.0) | 0.84 (0.75, 0.95) | .005 |
| Interpersonal relationships | 1.7 (1.0) | 1.7 (1.0) | 1.8 (1.0) | 0.87 (0.77, 0.98) | .03 |
| Self-harm | 1.5 (1.4) | 1.5 (1.4) | 1.5 (1.3) | 0.97 (0.88, 1.06) | .46 |
| Emotional lability | 2.1 (1.2) | 2.1 (1.2) | 2.0 (1.1) | 1.06 (0.95, 1.17) | .30 |
| Psychotic symptoms | 1.3 (1.2) | 1.4 (1.3) | 1.1 (1.2) | 1.21 (1.09, 1.34) | .0003 |
| Alcohol/drug abuse | 1.2 (1.1) | 1.2 (1.1) | 1.2 (1.1) | 0.99 (0.88, 1.10) | .82 |
| Overall summary score | 2.0 (0.8) | 2.0 (0.8) | 2.1 (0.7) | 0.87 (0.74, 1.03) | .10 |
| SF-12 scoresd | |||||
| Physical component score | 46.9 (12.6) | 46.8 (12.3) | 47.0 (13.0) | 1.00 (0.99, 1.00) | .76 |
| Mental component score | 31.4 (14.2) | 32.8 (14.1) | 29.5 (14.1) | 1.02 (1.01, 1.03) | .0003 |
BASIS-24 = Behavior and Symptom Identification Scale-24; CESD = Centre for Epidemiologic Studies Depression Scale; FTND = Fagerström Test of Nicotine Dependence; SF-12 = Short Form-12.
aOdds ratio (OR) = odds of being a menthol versus non-menthol smoker.
bRange = 0–30; ≥ 11 indicates significant depressive symptoms.
cRange = 0–4; higher scores indicate worse mental health.
dRange = 0–100, national normative value = 50, SD = 10; lower scores indicate worse functioning.
Results from bivariate logistic regression analyses predicting current menthol smoking from demographic, tobacco, and clinical characteristics are also presented in Table 1. Persons with SMI who were younger; with fewer years of education; lower income; and those who were Black, Hispanic, Asian/Pacific Islander, and multiracial/other versus Caucasian were significantly more likely to smoke menthol cigarettes. Smoking characteristics, including usual number of cigarettes per day, level of nicotine dependence, smoking within 30 minutes of waking, and stage of change were not significantly associated with menthol use. Those with a primary diagnosis of psychotic disorder or other disorder versus major depression were significantly more likely to smoke menthol cigarettes as were those reporting greater psychotic symptoms on the BASIS-24. In contrast, those with greater depression symptoms on the CES-D, greater problems with depression and interpersonal relationships on the BASIS-24, and poorer mental health functioning on the SF-12 were more likely to smoke only nonmenthol cigarettes.
Multivariate models that adjusted for age, race/ethnicity, years of education, income, psychiatric diagnosis, depression functioning, perceived interpersonal problems, and psychotic symptoms on the BASIS-24, and mental health functioning on the SF-12, indicated that those of younger age (adjusted odds ratio [AOR] = 0.98, 95% CI = 0.97, 0.99, p < .0001); Blacks (AOR = 5.52, 95% CI = 3.67, 8.32, p < .0001), Hispanics (AOR = 2.07, 95% CI = 1.39, 3.08, p = .0003), Asian Americans/Pacific Islanders (AOR = 2.00, 95% CI = 1.11, 3.62, p = .02), and identifying as multiracial/other (AOR = 2.17, 95% CI = 1.33, 3.56, p = .002) compared to Caucasians; those with fewer problems with interpersonal functioning (AOR = 0.85, 95% CI = 0.74, 0.98, p = .02); and those with greater psychotic symptoms (AOR = 1.15, 95% CI = 1.01, 1.31, p = .03) were significantly more likely to smoke menthol cigarettes.
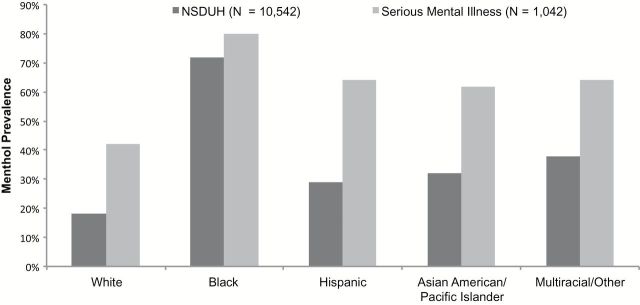
Prevalence of menthol use among adult California smokers in the NSDUH 2008–2011 surveys was 27.5% and did not differ appreciably by survey year (range 25% to 30%). Compared to the general population of adult smokers in California, menthol smoking prevalence was higher among adult smokers with SMI (57%), and this was found within all examined racial/ethnic groups (Figure 1). The differences were smallest among Blacks, for whom menthol prevalence in both the general population and among those with SMI exceeded 70%.
Figure 1.
Menthol smoking prevalence according to race/ethnicity among adults with serious mental illness and a California representative sample of adult smokers. California representative estimates of menthol smoking come from the 2008–2011 National Survey on Drug Use and Health17,28,29.
Discussion
The current study characterized menthol smoking among Black, Hispanic, Asian American/Pacific Islander, Caucasian, and multiracial/other smokers with SMI relative to smokers in the general population and assessed the demographic and clinical correlates of menthol smoking in this disproportionately impacted group. Results indicated that relative to the average adult smoker in California, adult smokers with SMI reported a higher prevalence of menthol cigarette smoking across all racial/ethnic groups.
Within the sample and controlling for a number of demographic and clinical characteristics, younger age, minority race/ethnicity, fewer perceived interpersonal problems, and greater psychotic symptoms were associated with a significantly increased likelihood of menthol cigarette smoking among smokers with SMI. This finding complements and extends prior research indicating a higher prevalence of menthol smoking among Caucasians with schizophrenia relative to Caucasians without mental illness, and greater menthol cigarette use among those with poorer mental health.14,17 With data analyzed from Florida, New Jersey, and now California, the associations between menthol use and mental illness/distress do not appear regionally-specific. Prior studies comparing to nonpsychiatric control groups have found greater depression and general distress among menthol versus nonmenthol users, while in the current sample, psychotic disorder and severity of psychotic symptoms showed stronger associations with menthol smoking than did depression. The lower depression scores among menthol users in the current study may reflect that the predominant disorder represented among menthol smokers was psychosis, which is not characterized by depression. When we examined the association between menthol smoking and psychiatric diagnosis separately for Caucasians and Blacks, psychotic disorder was only associated with a greater likelihood of menthol smoking (versus major depression) among Caucasian participants. This suggests that the association between psychosis and menthol smoking was not simply driven by a higher prevalence of psychotic disorders and menthol smoking among Blacks. The lack of significant association among Blacks is likely attributable to a ceiling effect, as the large majority of Blacks in our sample smoked menthol (80%), challenging the ability of any variable to predict variance in menthol smoking in this group. The finding of greater interpersonal problems among solely nonmenthol smokers was statistically significant though the mean difference between groups was only 0.1 on a 4-point scale.
The high prevalence of menthol smoking among persons with SMI relative to the general population is striking and likely influenced by multiple factors. Tobacco industry research on marketing of menthol cigarettes and consumer perceptions indicates that menthol cigarettes are marketed, and perceived by consumers, as healthier than nonmenthol cigarettes.31 Menthol may increase pleasure derived from inhaling cigarettes and reinforce smoking behaviors.32 In the only other study of a clinical sample of menthol smokers, menthol use among patients with schizophrenia was associated with elevated serum nicotine and cotinine levels and greater exhaled carbon monoxide levels compared to nonmenthol smokers.18 Although research is mixed with regard to elevated nicotine exposure levels from menthol,5 nicotine levels are elevated among smokers with psychosis,33 and menthol smoking may be a means to achieving higher nicotine levels in this population. Additional research is needed to investigate this possibility. Further, in the general population, menthol has been found to inhibit nicotine metabolism34 and is associated with upregulation of beta-2 nicotinic acetycholine receptors in the brain relative to nonmenthol cigarettes.35 Menthol’s anesthetic and bronchodilatory effects numb the throat, reduce the perceived harshness of cigarette smoke, open airways, and facilitate deeper inhalation of cigarette smoke, increasing exposure to cigarette-related carcinogens and providing an oral sensation that appeals to smokers36,37 and youth.12
Greater menthol use among persons with SMI overall, and among youth and racial/ethnic minorities in particular, could also be related to targeted marketing and advertising of menthol cigarettes. Persons with SMI have long been targeted by the tobacco industry,38 and greater access to price promotions and advertisements for menthol cigarettes may contribute to, or exacerbate, menthol smoking among this vulnerable group. Smokers are price sensitive,39 and the tobacco industry has targeted marketing of menthol cigarettes to poor neighborhoods across the United States.40 In California, the greatest prevalence of menthol price promotions is found in low-income communities and convenience stores (22.1%), gas stations (28.6%), and liquor stores (14.5%), with virtually no price promotions among supermarkets (0%), which are more common in wealthier neighborhoods.41 Further, tobacco companies also have aggressively marketed menthol cigarettes to urban Black communities6,8 and have used savvy marketing strategies to link menthol smoking with Black culture. Correspondingly, research has shown that Black adolescents are exposed to a greater number of menthol price promotions and lower menthol prices in tobacco retailers near their high schools,9 and are significantly more likely to recognize a menthol cigarette brand than nonmenthol brand.42 Smokers with SMI in the current study tended to be poor, with unstable living conditions, and it is possible that greater exposure to targeted marketing and cheaper menthol prices could contribute to the higher prevalence of menthol use in this group overall, and among racial/ethnic minorities in particular, via earlier initiation, greater risk of addiction, and lower rates of successful quitting.
The high prevalence of menthol cigarette smoking among smokers with SMI has important implications for prevention, intervention, and social policy. Smokers with SMI are responsive to tobacco control policies, such as smoking bans,43 and results from the current study suggest that a policy to include menthol in the FDA’s ban on characterizing flavorings in cigarettes may afford substantial public health benefits for this vulnerable group. Although little is known about attitudes toward regulating menthol among persons with SMI, nationally representative studies indicate the majority of Americans, including 68%–76% of Blacks, support an FDA ban of menthol cigarettes.44 In the current sample of adults with SMI, approximately half of menthol smokers were dual users, while the other half smoked menthol cigarettes exclusively. If menthol cigarettes were banned, it is unknown though anticipated that most dual-users would continue smoking nonmenthol cigarettes, while those who only smoke menthol cigarettes would be more likely to quit or cut down on smoking. The majority of studies addressing the likelihood of menthol smokers switching to nonmenthol cigarettes indicate that only a small proportion of menthol smokers report plans to switch to nonmenthol cigarettes. For example, 39% of adult menthol smokers reported that they would quit smoking if menthol cigarettes were no longer available, and only 12.5% reported that they would switch to a nonmenthol brand.45 Among young adult menthol smokers, 66% reported that they would quit smoking if menthol cigarettes were no longer available.46 A study that modeled the impact of a menthol ban, estimated a 10% reduction in overall smoking prevalence in the United States (and 25% reduction among Blacks) by 2050, averting 323,107 smoking-attributable deaths.47 Finally, although data from a large sample of adults suggested that smokers were less likely to support a ban on menthol than non-smokers (41% vs. 64%), there was a significant interaction with race such that, Black smokers were more likely to support banning menthol than non-Black smokers (71% vs. 38%).48 Taken together, the current findings support recent recommendations to ban the sale of menthol cigarettes in California41 and highlight the need for, and potential interest in, new tobacco control policies that reduce disparities in tobacco use among vulnerable populations.
Limitations
The current study and the NSDUH used different assessments of menthol use and the data from smokers with SMI were cross sectional; hence, inferences cannot be made about the risks and influences of menthol use over time. Further, smokers with SMI lived in the San Francisco Bay Area and may not be representative of smokers with SMI in the general California population. In our sample of smokers with SMI, 28% smoked menthol only, while 29% smoked both menthol and nonmenthol cigarettes. We are unable to tell from the current study what drives dual use (e.g., smoking anything that is available or price sensitivity), and additional research is needed to address this question.
Conclusions
The current study examined the prevalence and correlates of menthol cigarette use among a diverse sample of smokers with SMI. Findings indicate that menthol cigarette smoking is common and associated with greater psychotic symptoms, younger age, and racial/ethnic minority status. These cross-sectional data support the need for further investigation of menthol smoking as a potential vector contributing to tobacco-related disparities among individuals with SMI.
The FDA has the authority to regulate all tobacco products. Section 917(c) (4) of the Family Smoking Prevention and Tobacco Control Act included legislative language that prioritized an assessment of scientific findings regarding “…the impact of the use of menthol in cigarettes on the public health, including such use among children, African Americans, Hispanics, and other racial and ethnic minorities”.16 With a focus on protecting at risk groups, the FDA is currently considering regulation of menthol cigarettes,15 but there is no required timeline or deadline for regulatory action, and the Secretary of Health and Human Services has yet to make a regulatory decision.5 Results from the present study indicate that the FDA’s regulation of menthol cigarettes may have cessation and prevention benefits for individuals with SMI in general, and those with greater psychotic symptoms, younger age, and minority ethnicity/race in particular. If menthol is no longer allowed as a characterizing flavoring, smokers who use menthol, and menthol only smokers in particular, may be more likely to quit smoking, and those vulnerable to initiating smoking with menthol cigarettes may be less likely to start. Longitudinal data or natural experiments are needed to test whether restricting targeted menthol marketing or banning menthol cigarettes would support smoking cessation efforts in this priority population.
Funding
This work was supported by grants from the National Institute on Drug Abuse (#K23 DA018691, #P50 DA09253, #T32 DA007250), the National Institute of Mental Health (#RO1 MH083684), the National Cancer Institute (#R25 CA113710), and the National Heart, Lung, and Blood Institute (#T32 HL007034-37).
Declaration of Interests
None declared.
Acknowledgments
We thank Neal Benowitz, MD, for his consultation on research questions of interest regarding menthol cigarette use and mental illness.
References
- 1. Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Genl Psychiatry. 2004;61:1107–1115. [DOI] [PubMed] [Google Scholar]
- 2. Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: a population-based prevalence study. J Am Med Assoc. 2000;284:2606–2610. [DOI] [PubMed] [Google Scholar]
- 3. Manderscheid RW, Druss B, Freeman E. Data to manage the mortality crisis. Int J Ment Health. 2008;37:49–68. [Google Scholar]
- 4. Schroeder SA, Morris CD. Confronting a neglected epidemic: tobacco cessation for persons with mental illnesses and substance abuse problems. Annu Rev Public Health. 2010;31:297–314. [DOI] [PubMed] [Google Scholar]
- 5. Tobacco Products Scientific Advisory Committee to the Food and Drug Administration. Menthol Cigarettes and Public Health: Review of the Scientific Evidence and Recommendations. Washington, DC; 2011. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/TobaccoProductsScientificAdvisoryCommittee/UCM269697.pdf Accessed May 2012. [Google Scholar]
- 6. Gardiner PS. The African Americanization of menthol cigarette use in the United States. Nicotine Tob Res. 2004;6:S55–S65. [DOI] [PubMed] [Google Scholar]
- 7. Glanz K, Sutton NM, Jacob Arriola KR. Operation storefront Hawaii: tobacco advertising and promotion in Hawaii stores. J Health Commun. 2006;11:699–707. [DOI] [PubMed] [Google Scholar]
- 8. Yerger VB, Przewoznik J, Malone RE. Racialized geography, corporate activity, and health disparities: tobacco industry targeting of inner cities. J Health Care Poor Uuderserved. 2007;18(4 Suppl):10–38. [DOI] [PubMed] [Google Scholar]
- 9. Henriksen L, Schleicher NC, Dauphinee AL, Fortmann SP. Targeted advertising, promotion, and price for menthol cigarettes in California high school neighborhoods. Nicotine Tob Res. 2011;14:116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Caraballo RS, Asman K. Epidemiology of menthol cigarette use in the United States. Tob Induc Dis. 2011;9:S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fernander A, Rayens MK, Zhang M, Adkins S. Are age of smoking initiation and purchasing patterns associated with menthol smoking? Addiction. 2010;105:39–45. [DOI] [PubMed] [Google Scholar]
- 12. Rock VJ, Davis SP, Thorne SL, Asman KJ, Caraballo RS. Menthol cigarette use among racial and ethnic groups in the United States, 2004–2008. Nicotine Tob Res. 2010;12:S117–S124. [DOI] [PubMed] [Google Scholar]
- 13. Substance Abuse and Mental Health Services Administration. The NSDUH Report: Use of Menthol Cigarettes Rockville, MD: Substance Abuse and Mental Health Services Administration; 2009. http://oas.samhsa.gov/2k9/134/134MentholCigarettes.htm Accessed May 2012. [Google Scholar]
- 14. Webb-Hooper M, Zhao W, Byrne MM, et al. Menthol cigarette smoking and health, Florida 2007 BRFSS. Am J Health Behav. 2011;35:3–14. [DOI] [PubMed] [Google Scholar]
- 15.US Food and Drug Administration. Preliminary Scientific Evaluation of the Possible Public Health Effects of Menthol Versus Nonmenthol Cigarettes. 2013. http://www.fda.gov/tobaccoproducts/publichealthscienceresearch/menthol/default.htm. Accessed March, 2014.
- 16. House Report No. 1256. 111th Congress. 1st Session. Family Smoking Prevention and Tobacco Control Act 2008. http://www.gpo.gov/fdsys/pkg/PLAW-111publ31/html/PLAW-111publ31.htm Accessed March 2014.
- 17. Hickman NJ, Delucchi KL, Prochaska JJ. Menthol use among smokers with psychological distress: findings from the 2008 and 2009 national survey on drug use and health. Tob Control. 2012;23:7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Williams JM, Gandhi KK, Steinberg ML, Foulds J, Ziedonis DM, Benowitz NL. Higher nicotine and carbon monoxide levels in menthol cigarette smokers with and without schizophrenia. Nicotine Tob Res. 2007;9:873–881. [DOI] [PubMed] [Google Scholar]
- 19. Prochaska JJ, Hall S, Delucchi KL, Hall SM. Efficacy of initiating tobacco dependence treatment in inpatient psychiatry: a randomized controlled trial. Am J Public Health. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Prochaska JJ, Hall SE, Hall SM. Stage-tailored tobacco cessation treatment in inpatient psychiatry. Psychiatr Serv. 2009;60:848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Smith SS, Fiore MC, Baker TB. Smoking cessation in smokers who smoke menthol and non-menthol cigarettes. Addiction. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström test for nicotine dependence: a revision of the Fagerström tolerance questionnaire. Brit J Addict. 1991;86:1119–1127. [DOI] [PubMed] [Google Scholar]
- 23. Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psych. 1983;51:390–395. [DOI] [PubMed] [Google Scholar]
- 24. Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiat. 1998;59:22–33. [PubMed] [Google Scholar]
- 25. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Publication; 1994. [Google Scholar]
- 26. Eisen SV, Normand SL, Belanger AJ, Spiro A, III, Esch D. The Revised Behavior and Symptom Identification Scale (BASIS-R): reliability and validity. Med Care. 2004;42:1230–1241. [DOI] [PubMed] [Google Scholar]
- 27. Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. [DOI] [PubMed] [Google Scholar]
- 28. Substance Abuse and Mental Health Services Administration. 2009 National Survey on Drug Use and Health Rockville, MD; 2010. http://www.icpsr.umich.edu/files/SAMHDA/survey-inst/29621-0001-Questionnaire-specifications.pdf Accessed May 2012. [Google Scholar]
- 29. Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Mental Health Findings, NSDUH Series H-45, HHS Publication No. (SMA) 12-4725 Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. [Google Scholar]
- 30. SAS Institute Inc. SAS/STAT 9.3 User’s Guide. Cary, NC: SAS Institute Inc; 2011. [Google Scholar]
- 31. Anderson SJ. Marketing of menthol cigarettes and consumer perceptions: a review of tobacco industry documents. Tob Control. 2011;20:ii20–ii28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kreslake JM, Wayne GF, Connolly GN. The menthol smoker: tobacco industry research on consumer sensory perception of menthol cigarettes and its role in smoking behavior. Nicotine Tob Res. 2008;10:705–715. [DOI] [PubMed] [Google Scholar]
- 33. Strand JE, Nyback H. Tobacco use in schizophrenia: a study of cotinine concentrations in the saliva of patients and controls. Eur Psychiat. 2005;20:50–54. [DOI] [PubMed] [Google Scholar]
- 34. Benowitz NL, Herrera B, Jacob P. Mentholated cigarette smoking inhibits nicotine metabolism. J Pharmacol Exp Ther. 2004;310:1208–1215. [DOI] [PubMed] [Google Scholar]
- 35. Brody AL, Mukhin AG, La Charite J, et al. Up-regulation of nicotinic acetylcholine receptors in menthol cigarette smokers. Int J Neuropsychoph. 2012;1:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lindemann J, Tsakiropoulou E, Scheithauer MO. Impact of menthol inhalation on nasal mucosal temperature and nasal patency. Am J Rhinol. 2008;22:402–405. [DOI] [PubMed] [Google Scholar]
- 37. Wayne GF, Connolly GN. Application, function, and effects of menthol in cigarettes: a survey of tobacco industry documents. Nicotine Tob Res. 2004;6:S43–S54. [DOI] [PubMed] [Google Scholar]
- 38. Prochaska JJ, Hall SM, Bero LA. Tobacco use among individuals with schizophrenia: what role has the tobacco industry played? Schizophr Bull. 2008;34:555–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hyland A, Bauer JE, Li Q, et al. Higher cigarette prices influence cigarette purchase patterns. Tob Control. 2005;14:86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Weeks MO. Tobacco and media exposure in poor neighbourhoods: implications for the incidence of smoking among community residents. Int J Nurs Pract. 2011;17:534–538. [DOI] [PubMed] [Google Scholar]
- 41. Schleicher N, Johnson TO, Dauphinee AL, Henriksen L. Tobacco Marketing in California’s Retail Environment (2008–2011), Final report for the California Tobacco Advertising Survey (2011). Stanford, CA: Stanford Prevention Research Center; 2013. [Google Scholar]
- 42. Dauphinee AL, Doxey JR, Schleicher NC, Fortmann SP, Henriksen L. Racial differences in cigarette brand recognition and impact on youth smoking. BMJ Public Health. 2013;13:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lawn S, Pols R. Smoking bans in psychiatric inpatient settings? A review of the research. Aust N Z J Psychiatry. 2005;39:866–885. [DOI] [PubMed] [Google Scholar]
- 44. Winickoff J, McMillen R, Vallone D, et al. US attitudes about banning menthol in cigarettes: results from a nationally representative survey. Am J Public Health. 2011;101:1234–1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Pearson JL, Abrams DB, Niaura RS, Richardson A, Vallone DM. A ban on menthol cigarettes: impact on public opinion and smokers’ intention to quit. Am J Public Health. 2012;102:e107–e114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wackowski OA, Manderski MT, Delnevo CD. Young adults’ behavioral intentions surrounding a potential menthol cigarette ban. Nicotine Tob Res. 2014;16:876–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Levy DT, Pearson JL, Villanti AC, et al. Modeling the future effects of a menthol ban on smoking prevalence and smoking-attributable deaths in the United States. Am J Public Health. 2011;101:1236–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bolcic-Jankovic D, Biener L. Public opinion about FDA regulation of menthol and nicotine. Tob Control. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]