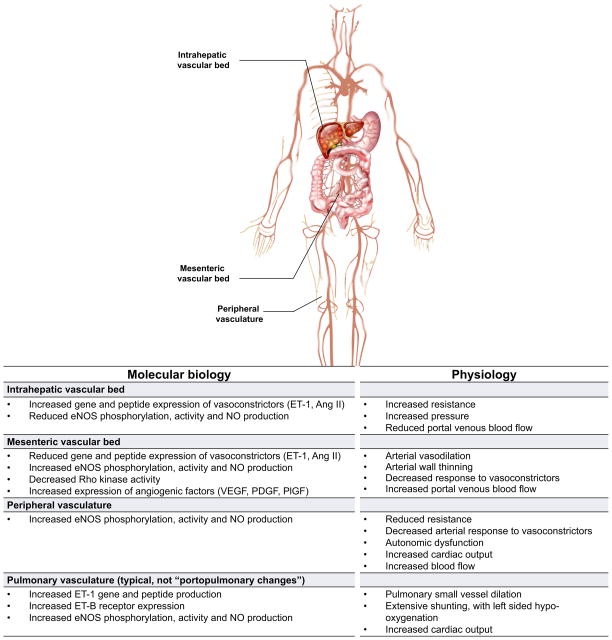
Fig. 1. Heterogeneity of vascular beds in portal hypertension.
Shown are prominent vascular beds and their associated pathophysiology. The intrahepatic vascular bed is typified by an increase in resistance to flow. Liver injury leads to abnormal endothelial function, with a reduction in the production of vasodilators by sinusoidal endothelial cells such as nitric oxide (NO); concomitantly, there is an increase in the synthesis of vasoconstrictors such as endothelin-1 (ET1) and angiotensin II (Ang II) by other cells in the sinusoid (see also Fig. 2). The mesenteric vascular bed is characterised by vasodilation by reduced resistance caused by upregulation of vasodilators such as NO, leading to increased flow to the portal vein. The net result of this physiology is an increase in intrahepatic resistance and portal blood flow from the splanchnic circulation, leading to increased portal pressure and portal hypertension. In peripheral vascular beds, increased eNOS activity and NO production typically leads to reduced resistance, low systemic pressure, and a hyperdynamic state typical of patients with cirrhosis. Abnormalities also exist in other vascular beds such as the pulmonary, brain, renal, and likely even others. Of note, increased intrahepatic resistance is only for the portal system, and the resistance of the hepatic artery is decreased. Therefore, due to the hepatic arterial buffer response, the total blood flow into the liver may be the same in cirrhosis [130]. ET-1, endothelin-1; Ang II, angiotensin II; NO, nitric oxide; eNOS, endothelial nitric oxide synthase; VEGF, vascular endothelial growth factor; PDGF, platelet derived growth factor; PlGF, placental growth factor.