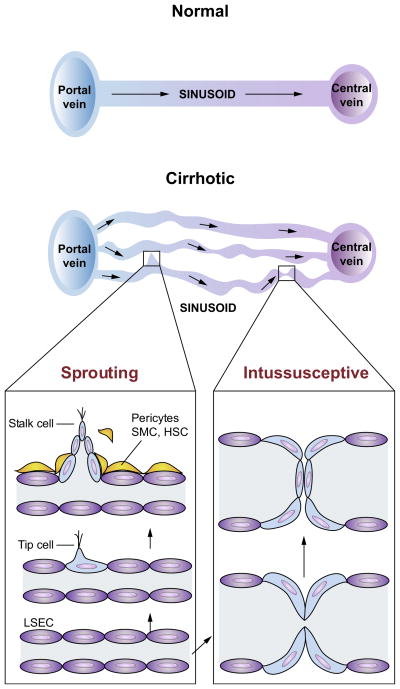
Fig. 3. Sprouting and intussusceptive angiogenesis in cirrhosis and portal hypertension.
Normal architecture of sinusoidal vasculature is shown in left panel with normal flow from portal venules, through sinusoidal microcirculation, to central veins. The sinusoidal vasculatures in the cirrhotic livers (right panel) are altered significantly, with increased number of sinusoidal vessels (angiogenesis) of various diameters and flow pattern. This is a simplified diagram of the sinusoidal microcirculation in liver cirrhosis. In cirrhosis, however, the relationship between the portal and central veins is not maintained because of fibrous septa and regenerative nodules, which disrupt the normal vascular architecture of portal venules, sinusoid and central vein. In sprouting angiogenesis, it is proposed that an endothelial ‘tip cell’ leads the vessel sprouts at the forefront and a trailing endothelial ‘stalk cell’ elongates behind the tip cell of a growing branch of vessels. Intussusceptive angiogenesis involves splitting vessels by the formation of translumenal pillars. Both forms of angiogenesis require the recruitment of pericytes or smooth muscle cells (SMCs). In cirrhotic livers, activated hepatic stellate cells (HSCs) are thought to serve as a role of pericytes and SMCs.