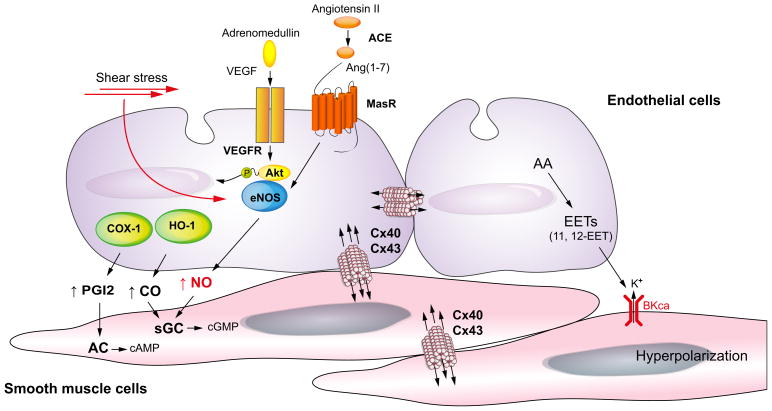
Fig. 4. Mechanisms of increased vasodilation in arteries of the splanchnic circulation in cirrhosis with portal hypertension.
In the splanchnic arterial circulation, agonists such as vascular endothelial growth factor (VEGF) and Ang(1-7) or physical stimuli such as shear stress activate endothelial nitric oxide (NO) synthase (eNOS). In cirrhosis, Ang(1-7) levels are significantly increased by upregulation of angiotensin-converting enzyme (ACE)-2. In addition, MasR, a receptor of Ang(1-7) is up-regulated in cirrhosis, resulting in an increase in eNOS activity and NO production. Besides NO, carbon monoxide (CO) produced by hemeoxygenase-1 (HO-1) causes vasodilation by activating soluble guanylate cyclase (sGC) to generate cyclic guanosine monophosphate (cGMP) in vascular smooth muscle cells. Prostacyclin (PGI2) is synthesised by cyclooxygenase (COX) and relaxes smooth muscle cells by stimulating adenylate cyclase (AC) to generate cyclic adenosine monophosphate (cAMP). Arachidonic acid (AA) metabolites [epoxyeicosatrienoic acids (EETs)] cause hyperpolarisation/relaxation, acting through voltage-gated potassium channel (BKCa) and gap junction [in particular connexins (Cx) 40 and 43].