Abstract
AIM
To evaluate usefulness of prophylactically intubating upper gastrointestinal bleeding (UGIB) patients.
METHODS
UGIB results in a significant number of hospital admissions annually with endoscopy being the key intervention. In these patients, risks are associated with the bleeding and the procedure, including pulmonary aspiration. However, very little literature is available assessing the use of prophylactic endotracheal intubation on aspiration in these patients. A comprehensive search was performed in May 2014 in Scopus, CINAHL, Cochrane databases, PubMed/Medline, Embase, and published abstracts from national gastroenterology meetings in the United States (2004–2014). Included studies examined UGIB patients and compared prophylactic intubation to no intubation before endoscopy. Meta-analysis was conducted using RevMan 5.2 by Mantel-Haenszel and DerSimonian and Laird models with results presented as odds ratio for aspiration, pneumonia (within 48 h), and mortality. Funnel plots were utilized for publication bias and I2 measure of inconsistency for heterogeneity assessments.
RESULTS
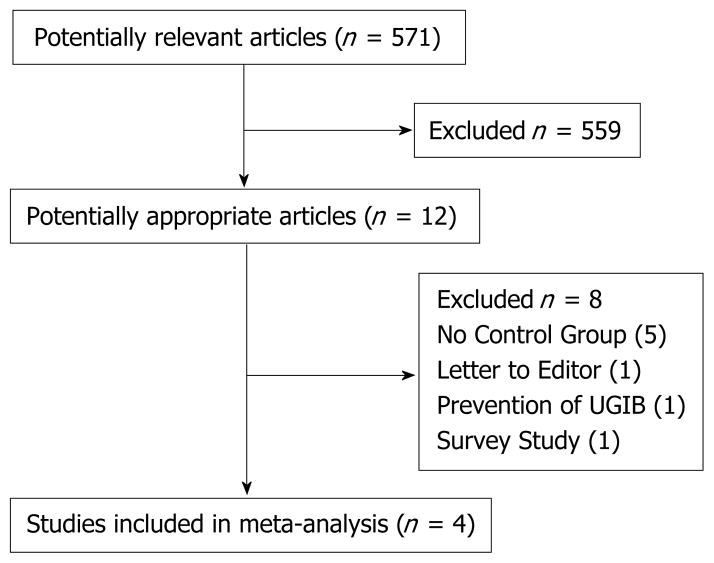
Initial search identified 571 articles. Of these articles, 10 relevant peer-reviewed articles in English and two relevant abstracts were selected to review by two independent authors (Almashhrawi AA and Bechtold ML). Of these studies, eight were excluded: Five did not have a control arm, one was a letter the editor, one was a survey study, and one was focused on prevention of UGIB. Therefore, four studies (N = 367) were included. Of the UGIB patients prophylactically intubated before endoscopy, pneumonia (within 48 h) was identified in 20 of 134 (14.9%) patients as compared to 5 of 95 (5.3%) patients that were not intubated prophylactically (P = 0.02). Despite observed trends, no significant differences were found for mortality (P = 0.18) or aspiration (P = 0.11).
CONCLUSION
Pneumonia within 48 h is more likely in UGIB patients who received prophylactic endotracheal intubation prior to endoscopy.
Keywords: Prophylactic endotracheal intubation, Upper gastrointestinal bleeding, Endoscopy, Complication, Pneumonia, Aspiration
INTRODUCTION
Upper gastrointestinal bleeding (UGIB) is still significant in the United States[1]. Health-resources utilization in those with UGIB is significantly higher than those without UGIB[2–5]. Although UGIB hospitalizations have decreased in the last decade, likely because the use of acid suppression therapy[6,7], mortality has not decreased and UGIB continues to be a significant cause of hospital admissions[8–13].
Many strategies have been implemented to reduce the morbidity, mortality, and cost associated with UGIB, including scoring systems, appropriate resuscitation, and improvements in endoscopic and non-endoscopic therapies[14–19]. In an attempt to reduce aspiration and aspiration pneumonia in patients presenting with UGIB, prophylactic tracheal intubation prior to performing endoscopy has been used, but is there any evidence to support such a practice. Tracheal intubation might prevent aspiration in selected cases but outcomes could be related to how experienced medical personnel performing the intubation is and how sick the patient is, i.e., with altered mental status or massive bleeding[20–22]. However, controversy does exist, even at our own institution, of the utility of prophylactic intubation in patients with UGIB. The largest reason for this controversy is that limited observational studies have addressed the utilization of tracheal intubation in the setting of UGIB[23–27]. These studies evaluated outcomes, including aspiration, mortality, aspiration pneumonia, and hospital length of stay. As our knowledge to answer the question of the utility of tracheal intubation in the setting of UGIB is still lacking, we conducted a meta-analysis to further evaluate such limited data.
MATERIALS AND METHODS
Search of literature
A complete search of Scopus, CINAHL, Cochrane databases, PubMed/Medline, and Embase was completed in May 2014. Search terms were used individually or in various combinations and included “endotracheal intubation”, “tracheal intubation”, “upper gastrointestinal bleeding”, “upper gastrointestinal hemorrhage”, “variceal hemorrhage”, “non-variceal hemorrhage”, “esophagogastroduodenoscopy”, “peptic ulceration”, “duodenal ulceration”, and “gastric ulceration”. Peer-reviewed studies on UGIB patients that compared prophylactic to no prophylactic intubation were selected and reviewed. References of relevant papers were searched as well for possible additional articles that were not identified in the original search. Search also included published abstracts in the major digestive disease conferences in the United States in the last 10 years. Three investigators reviewed all studies selected for inclusion criteria. Studies in children or in languages other than English were excluded from this meta-analysis.
Data extraction
All included studies were reviewed with two investigators (AA, MB). At least two of three primary outcomes were evaluated in all included studies. If a study had missing data on these subjects or clarification was needed, attempts were made to contact the authors to obtain the necessary information. Data from the studies chosen were extracted by two investigators individually and were settled by mutual agreement.
Statistical analysis
This meta-analysis followed principles of the MOOSE guidelines[28]. Meta-analysis was performed comparing the results of UGIB patients by calculating pooled estimates presented as odds ratio (OR) of outcomes with Mantel-Haenszel (if no heterogeneity) or DerSimonian and Laird models (if heterogeneity). Heterogeneity analyzed by calculating I2 measure of inconsistency (significant if P < 0.10 or I2 > 50%). A sensitivity analysis was done if heterogeneity was statistically significant. RevMan 5.2 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012) used for statistical analysis. Funnel plots were visually inspected for publication bias assessment.
Study quality assessment
The Effective Public Health Practice Project model was used to assess study quality[29]. This scale is based upon strong, moderate, or weak rankings for analysis, interventional integrity, withdrawal/dropout descriptions, data collection, blinding, confounders, design, and potential selection bias. Study quality is determined by how many weak ratings in each category (no weak ratings is strong, one weak is moderate, and ≥ 2 weak is weak).
Biostatistics
The corresponding author (Bechtold ML) is a biostatistician and has reviewed and approved all statistical data in the manuscript. Four of the authors (Hinds AM, Hammad HT, Nguyen DL, Bechtold ML) are extensively trained in the statistics used in meta-analysis.
RESULTS
Search of literature
Initially, 571 articles were discovered in the electronic databases (Figure 1). Ten relevant peer-reviewed articles in English and two relevant abstracts were selected for review by two independent authors (Almashhrawi AA and Bechtold ML). Of these studies, eight were excluded: Five did not have a control arm, one was a letter the editor, one was a survey study, and one was focused on prevention of UGIB. Therefore, four studies were identified as meeting inclusion criteria[24–27]. All the four studies included (N = 367) were retrospective cohorts. The studies were conducted throughout the United States and were published 2007 to 2014. All included studies examined the impact of prophylactic endotracheal intubation on UGIB outcomes (Table 1). The study quality was adequate based upon the Effective Public Health Practice Project model (Table 2).
Figure 1. Details of article search.
UGIB: Upper gastrointestinal bleeding.
Table 1.
Details of the studies
| Ref. | Study type | Country | Time | No. of patients | Group | n | Age (mean/median years) | Gender (% male) | Population (inclusion criteria) |
|---|---|---|---|---|---|---|---|---|---|
| Koch et al[25] | Retrospective | United States | 1995–2002 | 62 | PI | 42 | 49 | 74 | Bleeding varices |
| No PI | 20 | 48 | 65 | No radiographic or clinical respiratory issues | |||||
| Rehman et al[24] | Retrospective | United States | 2002–2006 | 98 | PI | 49 | 62b | 61 | Cirrhosis |
| No PI | 49 | 68b | 82 | Hematemesis Shock | |||||
| a Perisetti et al[26] | Retrospective | United States | 2000–2013 | 138 | PI | 69 | 61b | NA | Endoscopy with intubation |
| No PI | 69 | 66b | NA | Matched controls | |||||
| a Tang et al[27] | Retrospective | United States | 2008–2013 | 69 | PI | 43 | 53 | 69.8 | Endoscopy in suspected variceal bleeding |
| No PI | 26 | 55 | 61.5 |
Abstract;
Median.
PI: Prophylactic intubation; NA: Data not available.
Table 2.
Quality assessment of studies included in meta-analysis
| Ref. | Study design | Selection bias | Confounders | Blinding | Data collection methods | Withdrawals and dropouts | Intervention integrity | Analyses | Quality assessment |
|---|---|---|---|---|---|---|---|---|---|
| Koch et al[25] | Retrospective Moderate | Moderate | Moderate | Weak | Strong | NA | Moderate | Moderate | Moderate |
| Rehman et al[24] | Retrospective Moderate | Moderate | Strong | Weak | Strong | NA | Strong | Moderate | Moderate |
| Perisetti et al[26] | Retrospective Moderate | Moderate | Weak | Weak | Strong | NA | Moderate | Moderate | Weak |
| Tang et al[27] | Retrospective Moderate | Moderate | Strong | Weak | Strong | NA | Moderate | Moderate | Moderate |
NA: Data not available.
Pneumonia within 48 h
Pneumonia within 48 h was examined in three studies (N = 229)[24,25,27]. With prophylactic intubation, 20 of 134 (14.9%) patients with UGIB developed pneumonia. For those not being intubated, 5 of 95 (5.3%) patients with UGIB developed pneumonia within 48 h. Those UGIB patients who underwent prophylactic intubation had higher amount of pneumonia than those not prophylactically intubated with odds ratio of 3.13 (95%CI: 1.17–8.39; P = 0.02) with no statistically significant heterogeneity (I2 = 0%, P = 0.54) (Figure 2).
Figure 2. Forest plot demonstrating comparison of prophylactic intubation vs no intubation for patients with upper gastrointestinal bleeding for pneumonia within 48 h.
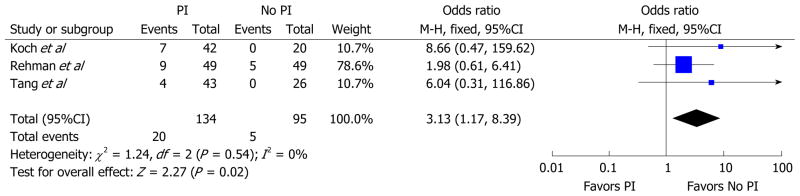
PI: Prophylactic intubation.
Mortality
Mortality was examined in four studies (N = 367)[24–27]. Mortality was noted in 39 of 203 (19.2%) patients with UGIB prophylactically intubated and 17 of 164 (10.4%) patients with UGIB not prophylactically intubated. No statistically significant higher mortality was noted for those patients prophylactically intubated (OR = 2.19; 95%CI: 0.69–6.95; P = 0.18) with statistically significant heterogeneity observed (I2 = 63%, P = 0.05) (Figure 3). Given significant heterogeneity, a sensitivity analysis was performed by excluding the Rehman et al[24] study which demonstrated a statistically significant higher mortality for those patients with prophylactically intubated as compared to those not intubated without significant heterogeneity with OR = 3.72 (95%CI: 1.55–8.92; P < 0.01).
Figure 3. Forest plot demonstrating comparison of prophylactic intubation vs no intubation for patients with upper gastrointestinal bleeding for mortality.
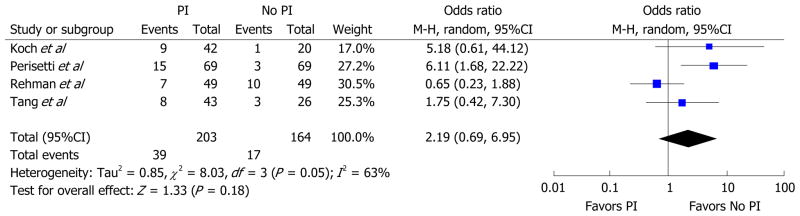
PI: Prophylactic intubation.
Aspiration
Aspiration was analyzed in four studies (N = 367)[24–27]. Aspiration was noted in 43 of 203 (21.2%) patients with UGIB prophylactically intubated and 13 of 164 (7.9%) patients with UGIB not intubated. Statistically non-significant higher aspiration was noted in patients with UGIB prophylactically intubated (OR = 3.99; 95%CI: 0.72–22.12; P = 0.11) with statistically significant heterogeneity (I2 = 77%, P = 0.01) (Figure 4). Given significant heterogeneity, a sensitivity analysis was performed by excluding the Perisetti et al[26] study which demonstrated a statistically significant more episodes of aspiration for those patients with prophylactically intubated as compared to those not intubated without significant heterogeneity (OR = 9.67; 95%CI: 3.40–27.52; P < 0.01; I2 = 0%, P = 0.94).
Figure 4. Forest plot demonstrating comparison of prophylactic intubation vs no intubation for patients with upper gastrointestinal bleeding for aspiration.
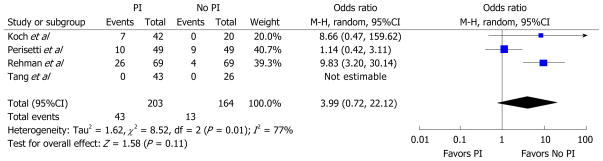
PI: Prophylactic intubation.
Publication bias
Publication bias was not observed in any outcomes in this meta-analysis based upon funnel plots.
DISCUSSION
In an effort to provide airway protection and reduce aspiration complications, providers may elect to perform tracheal intubation for patients presenting with UGIB. Unfortunately, there are no published guidelines to direct the use of endotracheal intubation in this group of patients, partly because of the lack of evidence-based recommendations. Emergent tracheal intubation is clearly indicated as a measure to protect airways in specific clinical presentations such as patients with altered mental status or those hemodynamically unstable. On the other hand, complications can arise directly from emergent tracheal intubations and the benefits of tracheal intubation should be weighed against the risks in each case individually. Schwartz et al[30] found that emergency intubation results in esophageal intubation in 8%, new pulmonary infiltrates identified post-intubation in 4%, and 3% died within 30 min of intubations, although those who died were those hemodynamically unstable before intubation. Only few studies evaluated this important subject and all were of retrospective design and varied in results[24–27].
Koch et al[25] evaluated the outcomes of 62 patients with 69 episodes of variceal bleeding who were either prophylactically intubated or not intubated prior to endoscopy and discovered significantly more aspiration in those who were prophylactically intubated. However, no differences were noted for mortality or length of stay[25]. Rehman et al[24] utilized 49 matched controls to 49 patients with UGIB and shock, cirrhosis, or hematemesis. Although cardiopulmonary complications are common in this population, no difference was discovered between the prophylactic intubation and no intubation in matched controls for mortality, length of stay, pneumonia, or aspiration[24]. Similarly, an abstract by Tang et al[27] in 69 patients with suspected variceal hemorrhage showed no significant differences between prophylactic intubation vs no prophylactic intubation for mortality, pneumonia, and length of stay. In contrast, an abstract by Perisetti et al[26] demonstrated that prophylactic intubation in patients with UGIB resulted in significantly more aspiration, length of stay, and mortality during hospitalization. Therefore, results has varied among the retrospective studies in regards to important outcomes such as aspiration, pneumonia, and mortality.
Due to this variability, we conducted this meta-analysis to evaluate the available evidence from four published retrospective studies that compared outcomes in UGIB patients who were prophylactically intubated and those who were not prophylactically intubated.
All studies evaluated mortality and aspiration[24–27], while only three studies evaluated pneumonia within 48 h as an outcome[24,25,27]. Our results show that there was a significant higher amount of pneumonia within 48 h in patients with UGIB who received endotracheal intubations prophylactically in comparison with those who were not intubated. In regards to aspiration and mortality, trends were noted toward worse outcomes in those patients who were prophylactically intubated but no statistically significant differences were noted. However, given significant heterogeneity, the sensitivity analyses demonstrated statistically significant worse outcomes for mortality and aspiration in those patients undergoing prophylactic intubation.
Strengths of our study are as follows. First, this is the first meta-analysis that evaluates outcomes difference between prophylactic intubation and no intubation in UGIB patients. Second, a large extensive search for relevant studies was conducted using several electronic search engines and three major gastroenterology and endoscopy conferences proceedings and abstracts for the period from 2004–2014. Third, each study included and evaluated at least two of the three outcomes studied in our meta-analysis. Four, the study populations were from different geographic areas in the United States and different time periods over 10 years, making it relevant to a large population. Fifth, no heterogeneity was identified in the pneumonia outcome. Finally, no publication bias was noted by the funnel plot. On the other hand, limitations were also apparent. First, a small number of studies were included. However, these studies are the only studies to-date on the subject. Second, all studies were observational with no randomized controlled trials on this issue which requires attention when forming conclusions from this meta-analysis and taken into consideration. Finally, significant heterogeneity was identified in two of the three outcomes (mortality and aspiration). Therefore, the DerSimonian and Laird model was utilized, limiting heterogeneity impact. Also, sensitivity analyses were performed which demonstrated statistically significant higher mortality and more aspiration in those patients undergoing prophylactic intubation. However, given the limited number of studies, subgroup analysis for sources of heterogeneity (such as location, timing, abstract exclusion) was not performed.
In conclusion, this meta-analysis demonstrates that patients with UGIB who received prophylactic endotracheal intubation have higher odds of having pneumonia within 48 h. Trends showing higher odds of mortality and aspiration in those prophylactically intubated were noted but no statistically significant differences were seen in comparison to those not intubated. Although these results must be interpreted with caution in light of the small number of studies in this meta-analysis leading to one or two studies having significant weight on the results, this study addresses prophylactic intubation in UGIB patients prior to endoscopy. Based upon these results, prophylactic tracheal intubation is not beneficial in patients with UGIB and should not be recommended.
Core tip.
Patients with upper gastrointestinal bleeding (UGIB) require endoscopic treatment with variable outcomes of aspiration, pneumonia, non-endoscopic interventions, and mortality. It is suggested that endotracheal intubation prior to endoscopy might reduce aspiration, pneumonia, and mortality. Few studies have evaluated this issue. We performed a meta-analysis of observational studies examining endotracheal intubation vs no intubation in UGIB patients. We found that patients intubated had higher incidence of pneumonia within 48 h. There was no significant increase in aspiration and mortality in the intubated group. This meta-analysis demonstrates the need for randomized controlled trials to assess the issue.
COMMENTS.
Background
Endoscopic treatment is the main treatment for upper gastrointestinal bleeding (UGIB) and preventing complications during endoscopy is important. Endotracheal intubation might be used to protect airways and prevent aspiration, pneumonia, and reduce mortality. This study shows no evidence to support this practice generally and appropriateness of endotracheal intubation should be determined for each case individually.
Research frontiers
The authors performed the first meta-analysis comparing prophylactic endotracheal intubation to no intubation for UGIB to evaluate for pneumonia (within 48 h), aspiration, and mortality.
Innovations and breakthroughs
This is the first meta-analysis comparing prophylactic endotracheal intubation to no intubation for UGIB. The authors found that there is no evidence to support universal use of prophylactic endotracheal intubation prior to endoscopy. On the contrary, significantly more episodes of pneumonia occurred with the intubated group, and trends for worse aspiration and mortality were seen as well in the intubated group although not statistically significant.
Applications
Endotracheal intubation should be determined on an individual case-by-case approach when considered prior to endoscopy for UGIB treatment. Further studies, preferably randomized controlled trials, are likely needed to fully assess the practice of prophylactic intubation in UGIB patients prior to endoscopy.
Terminology
Odds ratio: Statistical term for the odds an event did or did not occur. Mean difference: Statistical term of difference between the means for a given variable. Heterogeneity: Test for uniformity in composition of studies included. Publication bias: Phenomenon where positive studies are more likely to be published than negative studies, leading to possible misrepresentation of data in meta-analysis.
Peer review
This is a very early systematic review and meta-analysis investigating the impact of prophylactic tracheal intubation on iatrogenic pneumonia, all-cause mortality and aspiration arising from complications due to endoscopy for upper GI bleeding.
Footnotes
Author contributions: Almashhrawi AA, Nguyen DL and Bechtold ML were responsible for the conception and design of the study; Almashhrawi AA, Rahman R, Jersak ST and Hinds AM collected the data and organized data extraction sheets; Hammad HT, Nguyen DL and Bechtold ML statistically analyzed the data; Almashhrawi AA, Rahman R and Jersak ST drafted the manuscript with critical revision being performed by Asombang AW, Hammad HT, Nguyen DL and Bechtold ML.
Conflict-of-interest: The authors have no conflicts of interest for this manuscript.
Data sharing: No additional data are available.
Contributor Information
Ashraf A. Almashhrawi, Division of Gastroenterology and Hepatology, University of Missouri, Columbia, MO 65212, United States
Rubayat Rahman, Division of Gastroenterology and Hepatology, University of Missouri, Columbia, MO 65212, United States.
Samuel T. Jersak, Division of Gastroenterology and Hepatology, University of Missouri, Columbia, MO 65212, United States
Akwi W. Asombang, Division of Gastroenterology and Hepatology, University of Missouri, Columbia, MO 65212, United States
Alisha M. Hinds, Division of Gastroenterology and Hepatology, University of Missouri, Columbia, MO 65212, United States
Hazem T. Hammad, Division of Gastroenterology and Hepatology, University of Missouri, Columbia, MO 65212, United States
Douglas L. Nguyen, Division of Gastroenterology and Hepatology, University of California, Irvine, CA 92697, United States
Matthew L. Bechtold, Division of Gastroenterology and Hepatology, University of Missouri, Columbia, MO 65212, United States
References
- 1.Lewis JD, Bilker WB, Brensinger C, Farrar JT, Strom BL. Hospitalization and mortality rates from peptic ulcer disease and GI bleeding in the 1990s: relationship to sales of nonsteroidal anti-inflammatory drugs and acid suppression medications. Am J Gastroenterol. 2002;97:2540–2549. doi: 10.1111/j.1572-0241.2002.06037.x. [DOI] [PubMed] [Google Scholar]
- 2.Zaman A, Goldberg RJ, Pettit KG, Kaniecki DJ, Benner K, Zacker C, DiCesare J, Helfand M. Cost of treating an episode of variceal bleeding in a VA setting. Am J Gastroenterol. 2000;95:1323–1330. doi: 10.1111/j.1572-0241.2000.02020.x. [DOI] [PubMed] [Google Scholar]
- 3.Viviane A, Alan BN. Estimates of costs of hospital stay for variceal and nonvariceal upper gastrointestinal bleeding in the United States. Value Health. 2008;11:1–3. doi: 10.1111/j.1524-4733.2007.00208.x. [DOI] [PubMed] [Google Scholar]
- 4.Cryer BL, Wilcox CM, Henk HJ, Zlateva G, Chen L, Zarotsky V. The economics of upper gastrointestinal bleeding in a US managed-care setting: a retrospective, claims-based analysis. J Med Econ. 2010;13:70–77. doi: 10.3111/13696990903526676. [DOI] [PubMed] [Google Scholar]
- 5.Gleeson F, Clarke E, Lennon J, MacMathuna R, Crowe J. Outcome of accident and emergency room triaged patients with low risk non-variceal upper gastrointestinal haemorrhage. Ir Med J. 2006;99:114–117. [PubMed] [Google Scholar]
- 6.Laine L, Yang H, Chang SC, Datto C. Trends for incidence of hospitalization and death due to GI complications in the United States from 2001 to 2009. Am J Gastroenterol. 2012;107:1190–1195. doi: 10.1038/ajg.2012.168. quiz 1196. [DOI] [PubMed] [Google Scholar]
- 7.Zhao Y, Encinosa W. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet] Rockville (MD): Agency for Health Care Policy and Research (US); 2006 Feb–2008 Dec. Hospitalizations for Gastrointestinal Bleeding in 1998 and 2006: Statistical Brief #65. [Google Scholar]
- 8.Hreinsson JP, Kalaitzakis E, Gudmundsson S, Björnsson ES. Upper gastrointestinal bleeding: incidence, etiology and outcomes in a population-based setting. Scand J Gastroenterol. 2013;48:439–447. doi: 10.3109/00365521.2012.763174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Botianu A, Matei D, Tantau M, Acalovschi M. Mortality and need of surgical treatment in acute upper gastrointestinal bleeding: a one year study in a tertiary center with a 24 hours/day-7 days/week endoscopy call. Has anything changed? Chirurgia (Bucur) 2013;108:312–318. [PubMed] [Google Scholar]
- 10.Lanas A. Editorial: Upper GI bleeding-associated mortality: challenges to improving a resistant outcome. Am J Gastroenterol. 2010;105:90–92. doi: 10.1038/ajg.2009.517. [DOI] [PubMed] [Google Scholar]
- 11.Charatcharoenwitthaya P, Pausawasdi N, Laosanguaneak N, Bubthamala J, Tanwandee T, Leelakusolvong S. Characteristics and outcomes of acute upper gastrointestinal bleeding after therapeutic endoscopy in the elderly. World J Gastroenterol. 2011;17:3724–3732. doi: 10.3748/wjg.v17.i32.3724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marmo R, Koch M, Cipolletta L, Bianco MA, Grossi E, Rotondano G. Predicting mortality in patients with in-hospital nonvariceal upper GI bleeding: a prospective, multicenter database study. Gastrointest Endosc. 2014;79:741–749.e1. doi: 10.1016/j.gie.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Sostres C, Lanas A. Epidemiology and demographics of upper gastrointestinal bleeding: prevalence, incidence, and mortality. Gastrointest Endosc Clin N Am. 2011;21:567–581. doi: 10.1016/j.giec.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 14.Balaban DV, Strâmbu V, Florea BG, Cazan AR, Brătucu M, Jinga M. Predictors for in-hospital mortality and need for clinical intervention in upper GI bleeding: a 5-year observational study. Chirurgia (Bucur) 2014;109:48–54. [PubMed] [Google Scholar]
- 15.Tammaro L, Buda A, Di Paolo MC, Zullo A, Hassan C, Riccio E, Vassallo R, Caserta L, Anderloni A, Natali A. A simplified clinical risk score predicts the need for early endoscopy in nonvariceal upper gastrointestinal bleeding. Dig Liver Dis. 2014;46:783–787. doi: 10.1016/j.dld.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 16.Wang CH, Chen YW, Young YR, Yang CJ, Chen IC. A prospective comparison of 3 scoring systems in upper gastrointestinal bleeding. Am J Emerg Med. 2013;31:775–778. doi: 10.1016/j.ajem.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 17.Clarke MG, Bunting D, Smart NJ, Lowes J, Mitchell SJ. The surgical management of acute upper gastrointestinal bleeding: a 12-year experience. Int J Surg. 2010;8:377–380. doi: 10.1016/j.ijsu.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 18.Beggs AD, Dilworth MP, Powell SL, Atherton H, Griffiths EA. A systematic review of transarterial embolization versus emergency surgery in treatment of major nonvariceal upper gastrointestinal bleeding. Clin Exp Gastroenterol. 2014;7:93–104. doi: 10.2147/CEG.S56725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Targownik LE, Murthy S, Keyvani L, Leeson S. The role of rapid endoscopy for high-risk patients with acute nonvariceal upper gastrointestinal bleeding. Can J Gastroenterol. 2007;21:425–429. doi: 10.1155/2007/636032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thibodeau LG, Verdile VP, Bartfield JM. Incidence of aspiration after urgent intubation. Am J Emerg Med. 1997;15:562–565. doi: 10.1016/s0735-6757(97)90157-1. [DOI] [PubMed] [Google Scholar]
- 21.Waye JD. Intubation and sedation in patients who have emergency upper GI endoscopy for GI bleeding. Gastrointest Endosc. 2000;51:768–771. doi: 10.1016/s0016-5107(00)70104-0. [DOI] [PubMed] [Google Scholar]
- 22.Prather AD, Smith TR, Poletto DM, Tavora F, Chung JH, Nallamshetty L, Hazelton TR, Rojas CA. Aspiration-related lung diseases. J Thorac Imaging. 2014;29:304–309. doi: 10.1097/RTI.0000000000000092. [DOI] [PubMed] [Google Scholar]
- 23.Rudolph SJ, Landsverk BK, Freeman ML. Endotracheal intubation for airway protection during endoscopy for severe upper GI hemorrhage. Gastrointest Endosc. 2003;57:58–61. doi: 10.1067/mge.2003.46. [DOI] [PubMed] [Google Scholar]
- 24.Rehman A, Iscimen R, Yilmaz M, Khan H, Belsher J, Gomez JF, Hanson AC, Afessa B, Baron TH, Gajic O. Prophylactic endotracheal intubation in critically ill patients undergoing endoscopy for upper GI hemorrhage. Gastrointest Endosc. 2009;69:e55–e59. doi: 10.1016/j.gie.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koch DG, Arguedas MR, Fallon MB. Risk of aspiration pneumonia in suspected variceal hemorrhage: the value of prophylactic endotracheal intubation prior to endoscopy. Dig Dis Sci. 2007;52:2225–2228. doi: 10.1007/s10620-006-9616-0. [DOI] [PubMed] [Google Scholar]
- 26.Perisetti A, Khan H, Sahmoun A, Newman WMR. Role of prophylactic pre-esophagogastroduodenoscopy (EGD) endotracheal intubation (ETI) in upper gastrointestinal bleed (UGIB). A retrospective study. Am J Gastroenterol. 2013;108:S15–S16. (Abstract) [Google Scholar]
- 27.Tang Y, Wang Y, Wang WW. Elective endotracheal intubation prior to emergent EGD in patients with suspected variceal hemorrhage: An evaluation of outcome and complications. Gastrointest Endosc. 2014;79:AB515–AB516. (Abstract) [Google Scholar]
- 28.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 29.Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. J Eval Clin Pract. 2012;18:12–18. doi: 10.1111/j.1365-2753.2010.01516.x. [DOI] [PubMed] [Google Scholar]
- 30.Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults, A prospective investigation of 297 tracheal intubations. Anesthesiology. 1995;82:367–376. doi: 10.1097/00000542-199502000-00007. [DOI] [PubMed] [Google Scholar]