Abstract
Background
We sought to examine the beliefs and behaviors of emergency department (ED) providers related to preventing suicide by reducing suicidal patients’ access to lethal methods (“means restriction”) and to identify characteristics associated with asking patients about firearm access.
Methods
Physicians and nurses at eight EDs completed a confidential, voluntary survey.
Results
The response rate was 79% (n=631); 57% were female and 49% were nurses. Less than half believed “most” or “all” suicides are preventable. More nurses (67%) than physicians (44%) thought “most” or “all” firearm suicide decedents would have died by another method had a firearm been unavailable (P<0.001). The proportion of providers who reported they “almost always” ask suicidal patients about firearm access varied across five patient scenarios: suicidal with firearm suicide plan (64%), suicidal with no suicide plan (22%), suicidal with non-firearm plan (21%), suicidal in past month but not today (16%), and overdosed but no longer suicidal (9%). In multivariable logistic regression, physicians were more likely than nurses to “almost always” or “often” ask about a firearm across all five scenarios, as were older providers and those who believed their own provider type was responsible for assessing firearm access.
Conclusions
Many ED providers are skeptical about the preventability of suicide and the effectiveness of means restriction, and most do not assess suicidal patients’ firearm access except when a patient has a firearm suicide plan. These findings suggest the need for targeted staff education concerning means restriction for suicide prevention.
Keywords: Firearm, Hospital Care, Emergency Psychiatry, Screening, Attitudes
INTRODUCTION
In 2010, approximately 38,000 people in the U.S. committed suicide and another 465,000 were treated in emergency departments (ED) for non-fatal, self-inflicted injuries.[1] In the year before their death, 40% of suicide victims visit an ED at least once,[2, 3] and they are more likely to have multiple ED visits than those who die by other causes.[4] Such ED visits thus may represent an opportunity for intervention, although questions remain concerning how ED providers can best identify and care for patients with suicidal thoughts or behaviors[5, 6] and which ED-based interventions are most effective and efficient.
One way ED providers might prevent suicide is by assessing suicidal patient’s access to lethal means and counseling these patients with regard to lethal means restriction for suicide prevention.[7] In fact, lethal means restriction is one of only two approaches in suicide prevention that have been recognized as having a strong empirical foundation (the other is physician education in recognizing and treating depression).[8] In previous work, parents of at-risk youth seen in an ED were more likely to lock up firearms if they received injury prevention counseling by ED providers.[9, 10] Based on these results, ED means restriction education is included in the National Registry of Evidence-based Programs and Practices of the Substance Abuse and Mental Health Services Administration.[11] In addition, encouraging providers to routinely assess lethal means access among suicidal patients is a part of the 2012 National Strategy for Suicide Prevention.[12] Unfortunately, the few studies that have examined whether ED providers assess suicidal patients’ access to lethal means have all found lethal means assessment and counseling to be an infrequent event.[10, 13–16]
One prior study, at an urban academic hospital, explored possible reasons that ED practitioners only infrequently assess suicidal patients’ access to lethal means.[16] Some ED providers appeared to share the public’s skepticism about the effectiveness of means restriction,[16, 17] which may help explain their reluctance to inquire about access to lethal methods. The generalizability of these findings is limited, however, given the heterogeneity of EDs in the U.S.
The current study therefore examines the self-reported beliefs and behaviors of a larger sample of ED providers working at eight hospitals across the U.S. The current study also focuses more specifically on inquiring about access to firearms, the method used in more than half of all fatal suicidal acts in the U.S.,[1] and examines a broader range of clinically relevant patient scenarios.
MATERIALS AND METHODS
Study Design, Setting and Selection of Participants
The Emergency Department Safety Assessment and Follow-up Evaluation (ED-SAFE) project is a study of ED assessment and interventions for suicidal patients with eight sites located in seven states across the U.S. As part of the larger study, between June, 2010 and March, 2011, providers at participating EDs were asked to complete a survey about beliefs and behaviors concerning means restriction for suicide prevention. Additional questions concerning general knowledge, attitudes and practices related to suicidal ED patients will be reported elsewhere. Attending and resident physicians, mid-level providers, social workers and nurses working clinically at least half-time in the ED were eligible to participate, as well as those in leadership positions even if they worked fewer clinical hours.
Data Collection and Processing
The Emergency Medicine Network (www.emnet-usa.org) coordinated the study. Participants completed surveys in English online or on paper (a pre-addressed, postage-paid envelope was provided). Each provider had a unique numerical ID (assigned by the site); the coordinating center then notified the sites which providers had completed the survey so the sites could re-distribute surveys to non-responders. All responses were confidential, as the individual sites could not access the survey data and the coordinating center could not access the key linking provider names and IDs. Institutional review board approval with waived written informed consent was obtained at each site.
Methods of Measurement
Basic participant demographic characteristics were age, gender, self-described race (White; African-American; Asian; American Indian/Alaskan Native; Native Hawaiian/Other Pacific Islander; Other), and Hispanic ethnicity. For race, more than one response per participant was allowed; for multivariable analyses, we collapsed race and Hispanic ethnicity into two categories (non-Hispanic white only versus other). Provider variables included current position (Staff/Attending Physician; Resident Physician; Nurse; Other), years of work in medicine or nursing after completing medical or nursing school, and estimated number of suicidal patients seen per month.
Participants were asked about their beliefs and behaviors related to the care of suicidal and potentially-suicidal patients using multiple-choice questions. Regarding suicide prevention in general, providers were asked “What proportion of suicides do you consider preventable?” Response options were “none,” “a few,” “some,” “most,” “all.” Regarding means restriction as a suicide prevention strategy, providers were asked “Each month in the United States, over 1,000 people die by suicide using firearms. Had a firearm not been accessible to them, how many do you think would have found another way to die by suicide?” Response options were “few,” “some,” “most,” or “all.”
Additional questions assessed beliefs concerning who should be responsible for (1) assessing firearm access and (2) counseling patients and families about means restriction for suicide prevention, with multiple responses allowed for each (“ED nurse,” “ED physician,” “psychiatric nurse,” “psychiatrist,” “social worker/mental health counselor,” “other”). Because we hypothesized that behavior would vary by clinical scenario, we also asked how frequently providers ask if there are firearms at home for five patient examples: (1) suicidal in past month but not presently; (2) currently suicidal without a plan; (3) current suicide plan involving firearms; (4) current suicide plan not involving firearms; and (5) in the ED for an intentional overdose but no longer suicidal.
Outcome Measures and Data Analysis
We identified two primary outcome measures: the proportions of providers who (1) believed that “all” firearm suicide decedents would have died by another method had a firearm not been available; and (2) reported “almost always” or “often” assessing firearm access in all five of the patient scenarios. We omitted mid-level providers and social workers because of the small number in this subgroup (n=21), and we omitted an additional 4 (0.6%) observations with missing provider type. Because attending and resident physicians did not differ significantly from each other in their responses, we combined them for our main analyses.
For analysis, we first summarized characteristics of participants and their survey responses with medians with interquartile ranges (IQR) for continuous variables and proportions with 95 percent confidence intervals (95% CIs) for categorical variables. Next, we used unadjusted analyses to identify individual provider variables associated with each of our three outcomes of interest. To measure the strength of these associations, we calculated unadjusted odds ratios (ORs) with 95% CIs. For each of our primary outcomes of interest, we then performed separate logistic regression analyses to test for independent, statistically significant associations between the outcome variable of interest and provider characteristics (gender, age group, race, provider type, years in medicine, number of suicidal patients seen per month, and belief that one’s provider type should assess for firearm access). For the outcome related to firearm assessment in patient scenarios, an additional independent variable was belief in the effectiveness of means restriction (“few,” “some,” or “most” firearm suicides would have died by another method versus “all”). For each outcome the final multivariable model included predictor variables that were statistically significant in unadjusted analysis. All models (unadjusted and adjusted) models were created with the data clustered by study site.
RESULTS
Characteristics of Study Subjects
Of 799 eligible subjects at the eight sites, a total of 631 completed the survey, with an overall response rate of 79% (range: 72–87% among sites). Slightly more than half of respondents were women (57%), and the median age was 35 (range: 23–75; Table 1). The majority of participants identified themselves as white (94%) and non-Hispanic (97%). Excluding medical or nursing school, providers had been working in healthcare for a median of eight years (range: 0–50; IQR: 13) and estimated caring for a median of 15 suicidal patients a month (range: 1–300; IQR: 10; Table 1).
Table 1.
Characteristics of Responding ED Providers (n=631)
| median | IQR | ||
|---|---|---|---|
| Age in years | 35 | 30–44 | |
| Years of work in medicine/healthcare, excluding training | 8 | 3–16 | |
| Number of suicidal patients seen per month | 15 | 10–20 | |
| n | % | ||
| Sex | Male | 269 | 43 |
| Female | 359 | 57 | |
| Race | White | 590 | 94 |
| Black/African American | 10 | 1.6 | |
| Asian | 23 | 3.7 | |
| American Indian/Alaskan Native | 3 | 0.5 | |
| Native Hawaiian/Other Pacific Islander | 1 | 0.2 | |
| Other | 2 | 0.3 | |
| Hispanic or Latino origin | 17 | 2.7 | |
| Current clinical position | Nurse | 306 | 49 |
| Staff/Attending physician | 138 | 22 | |
| Resident physician | 187 | 30 | |
| Enrollment site | 1 | 93 | 15 |
| 2 | 28 | 4.4 | |
| 3 | 99 | 16 | |
| 4 | 80 | 13 | |
| 5 | 108 | 17 | |
| 6 | 70 | 11 | |
| 7 | 117 | 19 | |
| 8 | 36 | 5.7 | |
Legend.
Abbreviation: IQR, Interquartile Range.
Provider Beliefs
Less than half of providers (44%) believed that “most” or “all” suicides are preventable, without statistically significant differences by provider type (Table 2). However, more nurses (13%) than physicians (5.5%) said that “all” firearm suicide decedents would have died by another method had a firearm not been available (P<0.001; Table 2). In multivariable logistic regression, physicians (OR 0.46, 85%CI 9.23–0.91) and those who believed their provider type should assess for firearms (OR 0.41, 95%CI 0.28–0.60) were less likely to report believing that “all” decedents would have died by another method (Table 3). No other provider characteristic was significant in unadjusted analysis.
Table 2.
Self-reported provider beliefs concerning lethal means restriction for suicide prevention, by provider type (n=631)
| Nurse | Physician | Total | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| What proportion of suicides do you consider preventable? | ||||||
| All/most | 128 | 42 | 148 | 46 | 276 | 44 |
| Some/few | 170 | 56 | 169 | 52 | 339 | 54 |
| None | 6 | 2.0 | 7 | 2.2 | 13 | 2.1 |
| Each month in the U.S., over 1,000 people die by suicide using firearms. Had a firearm not been accessible to them, how many do you think would have found another way to die by suicide*** | ||||||
| Few | 4 | 1.3 | 14 | 4.3 | 18 | 2.9 |
| Some | 92 | 30 | 165 | 51 | 257 | 41 |
| Most | 165 | 54 | 124 | 38 | 289 | 46 |
| All | 40 | 13 | 18 | 5.5 | 58 | 9.2 |
| Whose responsibility do you think it is to assess a patient’s access to firearms and other lethal means to commit suicide? | ||||||
| ED nurse | 175 | 57 | 186 | 57 | 361 | 57 |
| ED physician** | 199 | 65 | 249 | 77 | 448 | 71 |
| Psychiatric nurse* | 218 | 71 | 206 | 63 | 424 | 67 |
| Psychiatrist | 257 | 84 | 270 | 83 | 527 | 84 |
| Social Worker/Mental health counselor** | 229 | 75 | 215 | 66 | 437 | 69 |
| Other* | 41 | 13 | 23 | 7.1 | 69 | 11 |
| Whose responsibility do you think it is to counsel patients and their families to limit access to firearms and other lethal means to commit suicide? | ||||||
| ED nurse* | 175 | 51 | 130 | 40 | 285 | 45 |
| ED physician | 183 | 60 | 201 | 62 | 384 | 61 |
| Psychiatric nurse** | 223 | 73 | 200 | 62 | 423 | 67 |
| Psychiatrist | 267 | 87 | 276 | 85 | 543 | 86 |
| Social Worker/Mental health counselor** | 235 | 77 | 214 | 66 | 449 | 71 |
| Other | 37 | 12 | 33 | 10 | 70 | 11 |
| How often do you personally counsel patients or their families to remove or lock up any guns at home?*** | ||||||
| Almost always | 16 | 5.2 | 23 | 7.1 | 39 | 6.2 |
| Often | 17 | 5.6 | 48 | 15 | 65 | 10 |
| Sometimes | 51 | 17 | 95 | 29 | 146 | 23 |
| Hardly ever | 220 | 72 | 158 | 49 | 378 | 60 |
Legend.
Abbreviation: CI, Confidence Interval.
P<0.05,
P<0.01,
P<0.001 under Chi Square.
Numbers may not add to total or 100% because of missing data (not shown if <5%)
Table 3.
Factors Associated with Belief that All Firearm Suicides Would Have Died by Another Method if No Firearm Was Available (n=622)
| Characteristic | Belief that “All” Would Have Died n (%) |
Unadjusted Odds Ratio (95% CI) |
Multivariable Odds Ratio† (95% CI) |
|---|---|---|---|
| Age (years) | -- | 1.02 (0.99–1.05) | |
| Years of work in medicine/healthcare, excluding training | -- | 1.01 (0.99–1.04) | |
| Number of suicidal patients seen per month | -- | 1.00 (0.99–1.01) | |
| Gender | |||
| Male | 22 (8.3) | 1.0 (Ref.) | |
| Female | 36 (10) | 1.25 (0.49–3.17) | |
| Self-described race & ethnicity | |||
| Other | 4 (7.1) | 1.0 (Ref.) | |
| Non-Hispanic White only | 54 (9.6) | 1.38 (0.38–5.07) | |
| Provider type | |||
| Nurse | 40 (13) | 1.0 (Ref.) | 1.0 (Ref.) |
| Physician | 18 (5.6) | 0.38 (0.21–0.73)** | 0.46 (0.23–0.91)* |
| Belief that my provider type should assess for firearms | |||
| No | 32 (16) | 1.0 (Ref.) | 1.0 (Ref.) |
| Yes | 26 (6.2) | 0.35 (0.24–0.53)*** | 0.41 (0.27–0.63)*** |
Legend.
Abbreviation: CI, Confidence Interval. Unadjusted and multivariable models all analyzed with clustering by study site.
P<0.05,
P<0.01,
P<0.001 under Chi Square.
Includes only variables significant in unadjusted analysis
Provider Behaviors
Over half of responding ED nurses and physicians thought it was the responsibility of an ED nurse (57%) or ED physician (71%) to ask about a patient’s access to firearms and other lethal means to commit suicide, with some differences by responding provider type (Table 2). The greatest proportion thought it was the responsibility of a psychiatrist (84%), although large proportions thought it was also the responsibility of a psychiatric nurse (67%) or social worker or mental health counselor (69%; Table 2). When asked who was responsible for counseling patients and families about restricting access to firearms and other lethal means for suicide, again the greatest proportions thought it was the responsibility of a psychiatrist (86%), psychiatric nurse (67%), or social worker or mental health counselor (71%). Fewer respondents saw this as a responsibility for an ED nurse (45%), or ED physician (61%), also with some differences by responding provider type (Table 2). Concerning their own behavior, 49% of physicians and 72% of nurses said they “hardly ever” personally counsel patients or families to remove or lock up guns at home (Table 2).
Scenarios
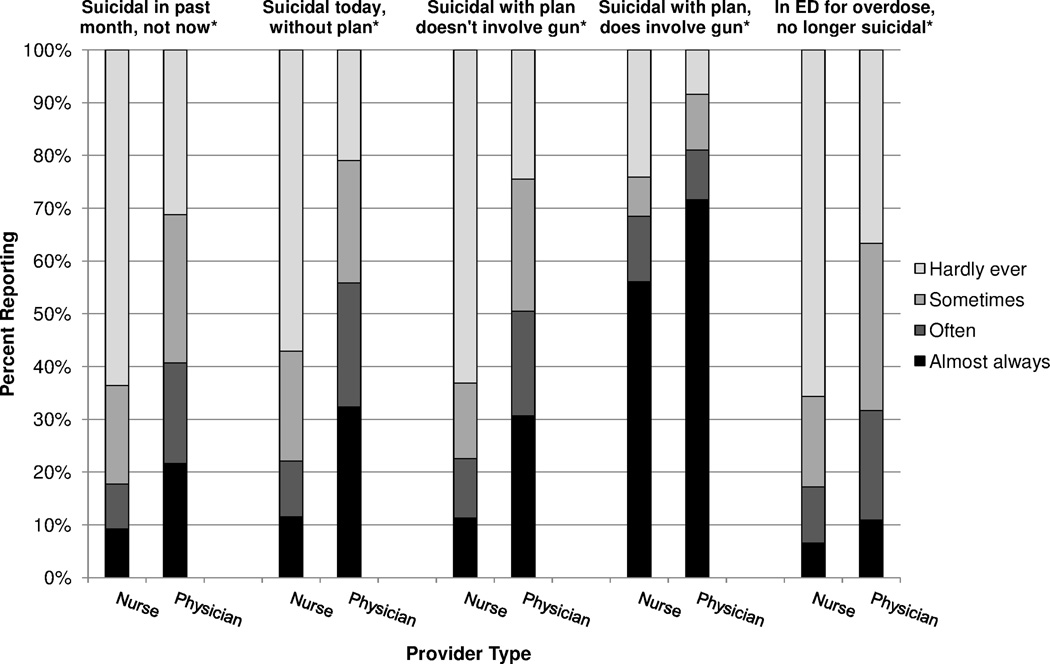
The survey included the question “I ask if there are firearms at home…” with five scenarios involving suicidal patients (Figure 1). For all scenarios, significantly more physicians than nurses reported “almost always” asking about firearms, and the frequency of reporting asking about firearms varied by scenario. The smallest proportions reported “almost always” or “often” asking in cases where a patient reported feeling suicidal over the past month but not presently (nurses 18%; physicians 41%;) or was in the ED for a multi-drug ingestion but no longer felt suicidal (nurses 17%; physicians 32%). Nurses were also significantly less likely than physicians to “almost always” or “often” ask about firearms at home in cases where a patient was suicidal without a plan (22% vs. 56%) or with a non-firearm plan (22% vs. 51%). A majority of both nurses (67%) and physicians (81%) said they “almost always” or “often” ask about firearms at home in cases where a patient is suicidal with a plan involving a firearm.
Figure 1. Response to the question "I ask if there are firearms at home" for various patient scenarios, by provider type (n=631).
*P<0.001 under Pearson chi-square test.
In multivariable logistic regression analysis of factors associated with “almost always” or “often” asking about firearms in all five patient scenarios, the final model included age, gender, provider type, and belief that one’s provider type should assess firearm access (Table 4), although gender was no longer significant after adjustment for other variables. Increasing age was associated with an increased likelihood of reporting “almost always” or “often” asking about firearms (OR 1.04, 95%CI 1.02–1.06 per year). Those who thought their provider type should assess firearm access were more likely to report “almost always” or “often” asking about firearms (OR 4.21, 95%CI 2.05–8.63), as were physicians (OR 1.94, 95%CI 1.17–3.22). Years in medicine, number of suicidal patients seen per month, race/ethnicity and belief in the effectiveness of means restriction were not significant in unadjusted analyses and therefore not included in the final model.
Table 4.
Unadjusted and Multivariable Logistic Regression Analysis of Factors Associated with Reporting “Almost Always” or “Often” Assessing Firearm Access in Patients across all Five† Scenarios (n=582)
| Characteristic | Almost Always/ Often Ask (n=103) |
Unadjusted Odds Ratio (95% CI) |
Multivariable Odds Ratio‡ (95% CI) |
|---|---|---|---|
| Age (years) | -- | 1.02 (1.01–1.04)*** | 1.04 (1.02–1.06)*** |
| Years of work in medicine/healthcare, excluding training | -- | 1.01 (0.99–1.02) | |
| Number of suicidal patients seen per month | -- | 1.00 (1.00–1.00) | |
| Gender | |||
| Male | 59 (22) | 1.0 (Ref.) | 1.0 (Ref.) |
| Female | 43 (13) | 0.50 (0.36–0.69)*** | 0.65 (0.39–1.06) |
| Self-described race & ethnicity | |||
| Other | 5 (11) | 1.0 (Ref.) | |
| Non-Hispanic White only | 98 (17) | 1.72 (0.64–4.70) | |
| Provider type | |||
| Nurse | 31 (11) | 1.0 (Ref.) | 1.0 (Ref.) |
| Physician | 72 (23) | 2.45 (1.71–3.53)*** | 1.94 (1.17–3.22)* |
| Belief that my provider type should assess for firearms | |||
| No | 13 (6.6) | 1.0 (Ref.) | 1.0 (Ref.) |
| Yes | 90 (22) | 3.92 (2.14–7.19)*** | 4.21 (2.05–8.63)*** |
| Belief in effectiveness of means restriction | |||
| Few/some/most would die by other method | 97 (18) | 1.0 (Ref.) | |
| All would die by other method | 6 (11) | 0.57 (0.27–1.18) | |
Legend.
P<0.01,
P<0.001 under Chi Square. Unadjusted and multivariable models all analyzed with clustering by study site.
In patients with (1) SI in past month but none presently; (2) current SI but without suicide plan: (3) suicide plan not involving firearm; (4) suicide plan involving firearm; (5) intentional overdose but no longer suicidal.
Includes only variables statistically significant in unadjusted analysis.
DISCUSSION
In this survey of over 600 nurses and physicians at eight EDs around the U.S., less than half of providers thought suicide was preventable. Previous work has demonstrated that some providers see suicide as an “acceptable” choice in incurable illness,[18] but this alone cannot explain our finding. Instead, our results reinforce concerns about gaps in provider training,[19, 20] bias in treating patients with mental health issues,[21] and skepticism about the effectiveness of suicide prevention approaches.[5, 20, 22] This is especially relevant at a time when widespread screening for suicide is becoming more common in EDs in response to the Joint Commission patient safety goal to “identify patients at risk for suicide,” by conducting “a risk assessment that identifies specific patient characteristics and environmental features that may increase or decrease the risk for suicide.”[23] With increasing ED detection of suicidal patients through screening, and the reality that not all suicidal ED patients will receive a formal evaluation by a mental health professional,[24, 25] it is critical that ED providers have adequate knowledge, skills and resources to provide optimal, compassionate care. While others have documented ED provider bias towards suicidal patients,[5] little was known about the extent to which ED providers assess and counsel patients with regard to lethal means restriction for suicide prevention.
Consistent with a prior single-center study,[16] we found that nurses were more skeptical than physicians about the effectiveness of means restriction as a suicide prevention method and less likely to provide means restriction counseling. This may stem from differences in physician and nursing training;[21] in this sample, age, gender, years of experience and number of suicidal patients seen per month were not significantly associated with means restriction beliefs. Many ED suicide screening and intervention protocols rely on the primary nurse, so it will be especially important to address nurse knowledge and beliefs concerning suicide with focused educational modules.[26]
In this study, over half of ED providers thought that ED physicians or nurses should assess suicidal patients’ access to firearms and other lethal means. However, in most of the scenarios less than half of providers said they “almost always” or “often” ask about firearm access. Even in cases in which a patient is suicidal and has a firearm suicide plan, while nearly two-thirds of providers said they “almost always” ask about firearms, 23% of nurses and 8% of physicians said they “hardly ever” ask. The fact that more providers asked in cases of a firearm suicide plan may suggest a tendency towards concrete thinking to deal with the specific problem at hand; i.e., providers may have heightened concern for patients with firearm suicide plans and therefore ask additional questions. However, although the likelihood of repeated suicidal acts is greater for persons with suicidal ideation and plans (versus suicidal ideation without plans),[27] subsequent suicidal attempts are as common among those with and without plans, because suicidal ideation without plans is more common than ideation with plans. Thus it is important that ED providers be encouraged to ask all suicidal patients about access to firearms and other lethal means, regardless of the presence or absence of a particular plan.
Whatever the reasons for asking or not asking in different scenarios, however, our findings highlight the need for focused provider training in means restriction. In a previous survey, only 42% of responding primary care physicians reported asking depressed or suicidal patients about firearm access, but those with continuing medical education training on the subject were more likely to do so.[28] Similarly, surveys of social workers found that those with prior training were more likely to assess firearm access.[29, 30] There has been little formal research on means restriction education for ED providers. Informal training such as distributing brochures to providers may be insufficient to significantly change provider behavior,[14, 30] but an in-person training has been associated with increases in the proportion of providers who report that they routinely counsel suicidal patients on reducing lethal means access.[31]
The study has a few limitations. First, providers at the eight participating EDs may differ from those at other EDs. Although the providers had a range of years of experience, the EDs were located in seven geographically disparate states (some with high and some with low rates of firearm ownership) and had different protocols and practices. All analyses were clustered by site; notably, we examined models without clustering and the primary results were not substantially changed. Next, we relied on provider self-report about behavior without independent verification, so recall or reporting bias could be issues. We chose to rely on self-report to ensure confidentiality and thereby increase the likelihood of truthfulness and participation. An additional limitation relates to the survey question about “personally counseling patients or their families to remove or lock up any guns at home,” as the question did not specifically refer to “suicidal” patients. However, the survey cover letter and other questions were all about suicidal ED patients, so respondents likely assumed the question referred to suicidal patients rather than patients in general. Also, survey questions about assessment or counseling did not refer specifically to admitted or discharged patients; providers may spend more time assessing or counseling those patients who will go home, with the thought that admitted patients will receive focused attention as inpatients. In addition, survey questions also did not refer specifically to patients who do or do not receive a full evaluation by a mental health professional, as providers may spend less time assessing or counseling those who have further evaluation. These issues will be important to examine in future work. Finally, we cannot make any conclusions about temporal or causal relationships from this cross-sectional study, but our findings are still useful in informing future design of research and care protocols.
CONCLUSIONS
Our study provides important new information concerning ED provider beliefs and behaviors related to lethal means restriction and care of suicidal patients in the ED. There have been several calls for ED providers to ask suicidal patients about firearms,[32–34] and a specific objective in the 2012 National Strategy for Suicide Prevention is to “encourage providers who interact with individuals at risk for suicide to routinely assess for access to lethal means.”[12] With growing patient caseloads and demands on ED providers, it is not reasonable to expect ED physicians or nurses to conduct lengthy assessments or counseling sessions for suicidal patients. The best option for ED efficiency and optimal patient care is to have available professionals with expertise in mental health and self harm,[35] such as psychiatrists, psychologists or social workers. However, brief risk assessment—including assessment of access to lethal means—and possibly brief interventions are reasonable skills for ED providers to master, and additional work is needed to enhance graduate and continuing medical or nursing education.
Supplementary Material
ACKNOWLEDGMENTS
We would like to acknowledge the time and effort of the research coordinators and research assistants from the 8 participating sites. ED-SAFE Investigators: Michael Allen, MD (University of Colorado Denver); Edward Boyer, MD, PhD (University of Massachusetts); Jeffrey Caterino, MD (Ohio State University Medical Center); Robin Clark, PhD (University of Massachusetts); Mardia Coleman (University of Massachusetts); Barry Feldman, PhD (University of Massachusetts); Amy Goldstein, PhD (National Institute of Mental Health); Talmage Holmes, PhD (University of Arkansas for Medical Sciences Medical Center); Maura Kennedy, MD (Beth Israel Deaconess Medical Center); Frank LoVecchio, DO (Maricopa Medical Center); Sarah A. Ting, PhD (Massachusetts General Hospital); Lisa Uebelacker, PhD (Memorial Hospital of Rhode Island); Wesley Zeger, DO (University of Nebraska Medical Center)
Funding: This project was supported by Award Number U01MH088278 from the National Institute of Mental Health, a Young Investigator Grant from the American Foundation for Suicide Prevention, and by grants from the Joyce and Bohnett Foundations. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health, the National Institutes of Health, or the other funders.
Footnotes
Presentations: Oral presentation at 2012 American Public Health Association annual meeting (October, 2012).
CONTRIBUTIONS: IM, CAC, and EDB conceived the study, designed the overall survey, and obtained research funding. MEB, MM and CB provided input on the survey questions related to lethal means assessment and counseling. AFS, IM, CAC, and EDB undertook recruitment of participating centers and managed the data, including quality control. MEB supervised the conduct of the survey and data collection at one participating site. AFS, IM, CAC, and EDB serve on the ED-SAFE Steering Committee. MEB, MM, CB, IM, CAC, and EDB designed the statistical analysis and MEB, MM and CB analyzed the data. MEB drafted the manuscript, and all authors contributed substantially to its revision. MEB and EDB take responsibility for the paper as a whole.
REFERENCES
- 1.Web-based injury statistics query and reporting system (WISQARS) Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Available at: http://www.cdc.gov/ncipc/wisqars/
- 2.Da Cruz D, Pearson A, Saini P, et al. Emergency department contact prior to suicide in mental health patients. Emerg Med J. 2011;28(6):467–471. doi: 10.1136/emj.2009.081869. [DOI] [PubMed] [Google Scholar]
- 3.Gairin I, House A, Owens D. Attendance at the accident and emergency department in the year before suicide: Retrospective study. Br J Psychiatry. 2003;183:28–33. doi: 10.1192/bjp.183.1.28. [DOI] [PubMed] [Google Scholar]
- 4.Morrison KB, Laing L. Adults' use of health services in the year before death by suicide in alberta. Health Rep. 2011;22(3):15–22. [PubMed] [Google Scholar]
- 5.D'Onofrio G, Jauch E, Jagoda A, et al. NIH roundtable on opportunities to advance research on neurologic and psychiatric emergencies. Ann Emerg Med. 2010;56(5):551–564. doi: 10.1016/j.annemergmed.2010.06.562. [DOI] [PubMed] [Google Scholar]
- 6.Horowitz LM, Ballard ED, Pao M. Suicide screening in schools, primary care and emergency departments. Curr Opin Pediatr. 2009;21(5):620–627. doi: 10.1097/MOP.0b013e3283307a89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yip PS, Caine E, Yousuf S, et al. Means restriction for suicide prevention. Lancet. 2012;379(9834):2393–2399. doi: 10.1016/S0140-6736(12)60521-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: A systematic review. JAMA. 2005;294(16):2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 9.Kruesi MJ, Grossman J, Pennington JM, et al. Suicide and violence prevention: Parent education in the emergency department. J Am Acad Child Adolesc Psychiatry. 1999;38(3):250–255. doi: 10.1097/00004583-199903000-00010. [DOI] [PubMed] [Google Scholar]
- 10.McManus BL, Kruesi MJ, Dontes AE, et al. Child and adolescent suicide attempts: An opportunity for emergency departments to provide injury prevention education. Am J Emerg Med. 1997;15(4):357–360. doi: 10.1016/s0735-6757(97)90124-8. [DOI] [PubMed] [Google Scholar]
- 11.National registry of evidence-based programs and practices: Emergency department means restriction education. Substance Abuse and Mental Health Services Administration; 2010. Available at: http://www.nrepp.samhsa.gov/ViewIntervention.aspx?id=15. [Google Scholar]
- 12.U.S. Department of Health and Human Services (HHS) Office of the Surgeon General and National Action Alliance for Suicide Prevention. 2012 National Strategy for Suicide Prevention: Goals and Objectives for Action. Washington, DC: HHS; 2012. Sep, Available at: http://www.sprc.org/sites/sprc.org/files/library/nssp.pdf. [PubMed] [Google Scholar]
- 13.Grossman J, Dontes A, Kruesi MJP, et al. Emergency nurses' responses to a survey about means restriction: An adolescent suicide prevention strategy. J Amer Psych Nurses Assoc. 2003;9(3):77–85. [Google Scholar]
- 14.Fendrich M, Kruesi MJ, Wislar JS, et al. Implementing means restriction education in urban eds. Am J Emerg Med. 1998;16(3):257–261. doi: 10.1016/s0735-6757(98)90096-1. [DOI] [PubMed] [Google Scholar]
- 15.Giggie MA, Olvera RL, Joshi MN. Screening for risk factors associated with violence in pediatric patients presenting to a psychiatric emergency department. J Psychiatr Pract. 2007;13(4):246–252. doi: 10.1097/01.pra.0000281485.96698.6d. [DOI] [PubMed] [Google Scholar]
- 16.Betz ME, Barber CW, Miller M. Firearm restriction as suicide prevention: Variation in belief and practice among providers in an urban emergency department. Inj Prev. 2010;16:278–281. doi: 10.1136/ip.2009.025296. [DOI] [PubMed] [Google Scholar]
- 17.Miller M, Azrael D, Hemenway D. Belief in the inevitability of suicide: Results from a national survey. Suic Life Threat Behav. 2006;36(1):1–11. doi: 10.1521/suli.2006.36.1.1. [DOI] [PubMed] [Google Scholar]
- 18.Anderson M. Nurses' attitudes towards suicidal behaviour--a comparative study of community mental health nurses and nurses working in an accidents and emergency department. J Adv Nurs. 1997;25(6):1283–1291. doi: 10.1046/j.1365-2648.1997.19970251283.x. [DOI] [PubMed] [Google Scholar]
- 19.Moorhead JC, Adams BE, Aghababian RV, et al. An assessment of emergency medicine residency graduates' perceptions of the adequacy of their residency training. Ann Emerg Med. 1989;18(6):701–704. doi: 10.1016/s0196-0644(89)80534-7. [DOI] [PubMed] [Google Scholar]
- 20.Larkin GL, Beautrais AL, Spirito A, et al. Mental health and emergency medicine: A research agenda. Acad Emerg Med. 2009;16(11):1110–1119. doi: 10.1111/j.1553-2712.2009.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Improving the quality of health care for mental and substance-use conditions: Quality chasm series. Washington, D.C.: Institute of Medicine, Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders; 2006. Available at: http://www.nap.edu/catalog/11470.html. [Google Scholar]
- 22.Berlim MT, Perizzolo J, Lejderman F, et al. Does a brief training on suicide prevention among general hospital personnel impact their baseline attitudes towards suicidal behavior? J Affect Disord. 2007;100(1–3):233–239. doi: 10.1016/j.jad.2006.09.035. [DOI] [PubMed] [Google Scholar]
- 23.Hospital National Patient Safety Goals. Joint Commission on Accreditation of Healthcare Organizations. 2011 Available at: http://www.jointcommission.org/assets/1/6/2011_NPSGs_HAP.pdf. [Google Scholar]
- 24.Baraff LJ, Janowicz N, Asarnow JR. Survey of california emergency departments about practices for management of suicidal patients and resources available for their care. Ann Emerg Med. 2006;48(4):452–458. 458 e1–458 e2. doi: 10.1016/j.annemergmed.2006.06.026. [DOI] [PubMed] [Google Scholar]
- 25.Kemball RS, Gasgarth R, Johnson B, et al. Unrecognized suicidal ideation in ED patients: Are we missing an opportunity? Am J Emerg Med. 2008;26(6):701–705. doi: 10.1016/j.ajem.2007.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Giordano R, Stichler JF. Improving suicide risk assessment in the emergency department. J Emerg Nurs. 2009;35(1):22–26. doi: 10.1016/j.jen.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 27.Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the national comorbidity survey. Arch Gen Psychiatry. 1999;56(7):617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- 28.Kaplan MS, Adamek ME, Rhoades JA. Prevention of elderly suicide. Physicians' assessment of firearm availability. Am J Prev Med. 1998;15(1):60–64. doi: 10.1016/s0749-3797(98)00019-1. [DOI] [PubMed] [Google Scholar]
- 29.Slovak K, Brewer TW. Suicide and firearm means restriction: Can training make a difference? Suic Life Threat Behav. 2010;40(1):63–73. doi: 10.1521/suli.2010.40.1.63. [DOI] [PubMed] [Google Scholar]
- 30.Slovak K, Brewer TW, Carlson K. Client firearm assessment and safety counseling: The role of social workers. Social Work. 2008;53(4):358–366. doi: 10.1093/sw/53.4.358. [DOI] [PubMed] [Google Scholar]
- 31.Johnson RM, Frank EM, Ciocca M, et al. Training mental healthcare providers to reduce at-risk patients' access to lethal means of suicide: Evaluation of the calm project. Arch Suicide Res. 2011;15(3):259–264. doi: 10.1080/13811118.2011.589727. [DOI] [PubMed] [Google Scholar]
- 32.Houry D. Suicidal patients in the emergency department: Who is at greatest risk? Ann Emerg Med. 2004;43(6):731–732. doi: 10.1016/j.annemergmed.2004.02.034. [DOI] [PubMed] [Google Scholar]
- 33.Buzan RD, Weissberg MP. Suicide: Risk factors and therapeutic considerations in the emergency department. J Emerg Med. 1992;10(3):335–343. doi: 10.1016/0736-4679(92)90340-y. [DOI] [PubMed] [Google Scholar]
- 34.Simon RI. Gun safety management with patients at risk for suicide. Suic Life Threat Behav. 2007;37(5):518–526. doi: 10.1521/suli.2007.37.5.518. [DOI] [PubMed] [Google Scholar]
- 35.Mitchell AJ, Dennis M. Self harm and attempted suicide in adults: 10 practical questions and answers for emergency department staff. Emerg Med J. 2006;23(4):251–255. doi: 10.1136/emj.2005.027250. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.