Abstract
Aim:
This study was conducted to assess the role of cytology in the diagnosis of lung lesions and to compare it with histopathology. It was also intended to evaluate the role of rapid on site evaluation (ROSE) as an adjunct to cytological diagnosis of lung lesions.
Materials and Methods:
The study included all the cases of lung lesions, which were diagnosed on cytology followed by histopathology over a period of 2½ years along with ROSE, wherever possible.
Results:
Cytology was done in total 782 cases of various lung lesions and of this cyto-histopathological correlation was available in 215 cases. ROSE was done in 93.4% of total cases and smears were considered on the site adequate in the first pass in 68.1% cases and in second pass adequacy increased to 93.4%. The diagnostic accuracy of cytology was 75.3%, and that of histology was 86.9% in the diagnosis of lung lesions. The diagnostic accuracy of cytology for squamous cell carcinoma (94.4%) and adenocarcinoma (96.5%) was higher than that of histology.
Conclusion:
Cytology is comparable to histology in the diagnosis of lung lesions and may even outperform biopsy in lung tumor diagnosis. The advantages of cytology may be further added by better sampling and preanalytical assessment for adequate diagnostic material and ROSE has proved to be an important, easy and cost effective adjunct in this regard. A multidisciplinary approach involving pulmonologist, radiologist and cytopathologist with ROSE, followed by vigilant morphological examination may increase diagnostic utility of cytology for lung lesions.
Keywords: Cytology, cyto-histopathological correlation, histology, lung lesions, rapid on site evaluation
Introduction
In the recent years with the emerging revolution of new targeted therapies in the treatment of lung lesions, the role of the pathologist has been affected dramatically. The utility of cytology in a precise diagnosis of lung lesions has also emerged as the subject of controversy.[1] This is especially important as recently International Association for the Study of Lung Cancer, American Thoracic Society and the European Respiratory Society has provided a standardized classification for lung cancer diagnosis considering small biopsies and cytology.[2] Although the cytological diagnosis in lung lesions may be limited due to potential sampling error but its importance cannot be underestimated as majority of lung tumors present in advanced unresectable stage. In addition, the role of the rapid on-site evaluation (ROSE) is also fast emerging as an important adjunct for cytological diagnosis, especially in image-guided needle aspirates. Therefore, the present study was conducted to assess the role of cytology in the diagnosis of lung lesions and to compare it with histopathological diagnosis. It was also intended to evaluate the role of ROSE as an adjunct to cytological diagnosis of lung lesions.
Materials and Methods
The study included all the cases of lung lesions which were diagnosed on cytology followed by histopathology over a period of 2½½ years in the Pathology Department of the Institute. Cases in which histopathology was not available were excluded from the study. The methods used for cytological diagnosis were broncho alveolar lavage (BAL), bronchial brushings, transbronchial needle aspirate (TBNA) and computed tomography/ultrasonography (CT/USG) guided fine needle aspiration cytology (FNAC) either alone or in combination. ROSE was done in the presence of cytopathologist in the procedural room of bronchoscopy or radiology itself, wherever possible. The smears for ROSE were assessed by using the rapid staining by toluidine blue. The stain was prepared by dissolving 0.5 g of crystalline toluidine blue in 20 mL of 95% ethanol and making the solution up to 100 mL by adding distilled water, filtered and refrigerated. A drop of stain was put on freshly prepared air-dried smear and was washed with water after 1-min and observed for adequacy of the smear. Adequacy of the smear was assessed by presence of at least five clusters of 6-8 epithelial cells and/or lymphoid cells with lymphoglandular bodies or as proposed by Burlingame et al.[3] Smears which showed only hemorrhage, necrosis or mucoid material were considered inadequate and were subjected to re-aspiration instantaneously.
Results
The cytological examination was done in total 782 cases of various lung lesions in the Pathology Department of the Institute over the study period, and out of these cyto-histopathological correlation was available in 215 cases. Figure 1 shows the various cytological procedures used for diagnosis of lung lesions either alone or in combination. Transthoracic FNAC was done either under CT guidance (19 cases), USG guidance (12 cases) and directly in 5 cases. Imprint smears were made from the biopsy in 2 cases. The ROSE was done in total 93.4% cases (201 cases) out of total 215 cases. The smears were considered on the site adequate in the first pass in 68.1% cases (137 cases) out of total 215. Those cases, which were considered inadequate on ROSE in the first pass were subjected to the second pass, and now the adequacy increased to 93.4%. Table 1 shows the comparison of different cytological methods for the diagnosis of various lung lesions. It shows that the diagnostic accuracy of bronchial brushings was 80.3%, followed by TBNA which was 75.7%. Table 2 shows the broad categorization of the various lung lesions on cytological examination. Malignancy was the most common broad category comprising of 51.5% of total cases. Table 3 shows the diagnostic accuracy of cytology and histology of broad categories of lung lesions. Table 4 shows the cytopathological correlation, discordance and diagnostic accuracy of various lung lesions. It shows that diagnostic accuracy of cytology for squamous cell carcinoma (SCC) (94.4%) and adenocarcinoma (AdCa) (96.5%) was higher than that of histology.
Figure 1.
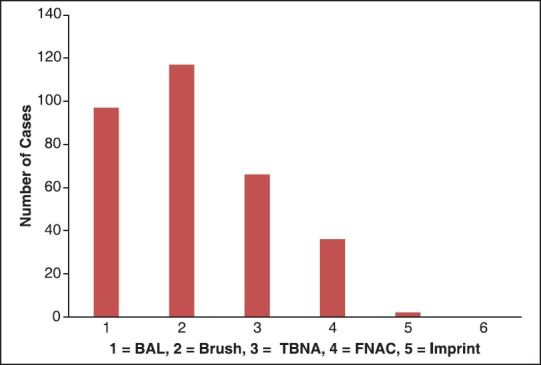
Bar chart showing different cytological methods used for obtaining cytological material for diagnosis of lung lesions
Table 1.
Comparison of different cytological methods for diagnosis of lung lesions
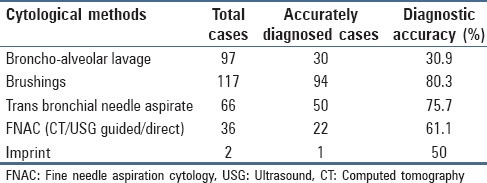
Table 2.
Broad categorization of lung lesions on cytological examination
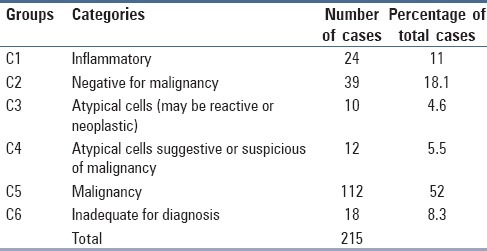
Table 3.
Diagnostic accuracy of cytology and histology of lung lesions
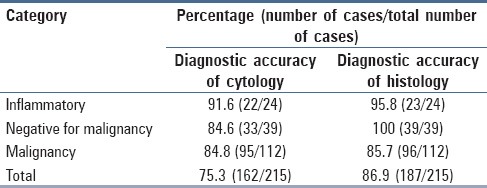
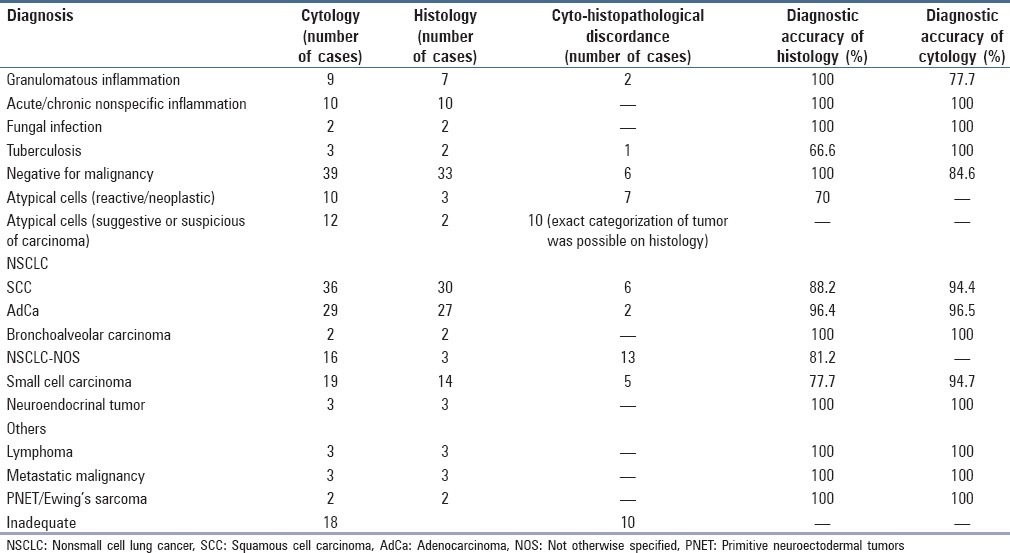
Table 4.
Cyto-histopathological corelation in lung lesions
Discussion
The role of cytology in the diagnosis of various lung lesions has been subject of debate especially with the emerging role of targeted therapy in the management of lung tumors. The therapeutic advances of non small cell lung cancer (NSCLC) includes tyrosine kinase inhibitors as first line therapy in lung AdCa with epidermal growth factor receptor mutations and bevacizumab is contraindicated in SCC as it is associated with life threatening hemorrhage.[4,5] This implies that it is necessary to precisely classify the NSCLC into AdCa or SCC so as to undergo targeted therapy. It further leads to question that whether cytology may be used as an answer to the precise diagnosis of lung lesions. The advantage of cytology as minimally invasive procedure with low complication rate requires no justification, but the procurement of adequate material for cytological diagnosis may limit its role. The assessment of sample adequacy preanalytically by utilization of the technique of ROSE, has proved advantageous in this regard. In the present study, 68.1% cases were considered adequate for evaluation on ROSE in the first pass but the remaining 31.9% cases were inadequate due to the presence of only hemorrhage, necrosis or mucoid material. Such cases were instantaneously subjected to re-aspiration (TBNA or FNAC) or brushing and now the adequacy increased to 93.4%. This shows that ROSE, which is simple, cost-effective technique may be immensely helpful in reducing the sampling error and thus increasing the accuracy of cytology in the diagnosis of lung lesions.[6] It may also yield preliminary diagnosis especially in distinguishing between nonneoplastic and neoplastic, if not the precise categorization, for lung lesions.[7] In the present study also preliminary distinction between neoplastic and non-neoplastic was possible on ROSE in a fair number of cases but the final diagnosis was given only after microscopic examination of routine conventional smears [Figure 2].
Figure 2.
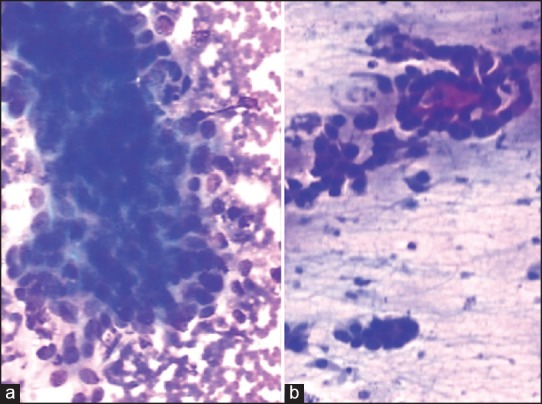
(a) Papillaroid fragment of adenocarcinoma on rapid on site evaluation on (ROSE) (toluidine blue, ×100) (b) Squamous cell carcinoma on ROSE (toluidine blue, ×100)
In addition, as fine-needle aspiration (FNA) or brush can be directed to different areas of lung lesions in comparison to biopsy so it is easy to get representative sample in heterogeneous lung lesion especially tumors. This may further add to the utility of cytology in the diagnosis of lung tumors as observed in Figure 3. The present study also showed the highest diagnostic accuracy of brushings (80.3%) in comparison to different cytological methods for lung lesions [Table 1]. Other studies have shown that for diagnosis of lung cancers FNA had an upper edge over core biopsy which may be related to better sampling.[8] Fischer et al.[9] observed that if fragments of one FNA pass are laid out in paraffin cell block at one plane, relatively larger number of tumor cells are displayed in each section compared with core biopsy of comparable weight. The close and vigilant appreciation of morphological features according to the set criteria may be highly useful for cytological differentiation of SCC and AdCa.[7] The Papanicolaou (Pap) staining for demonstrating keratinization and observation of acini and three dimensional clusters can be useful in this regard. Previous studies have also observed that Pap staining on cytological smears may highlight even minimal keratinization in comparison to hematoxyline and eosin staining of histological sections for diagnosis.[10] Crush artifact was also observed as an important limitation on biopsy in the present study with better nuclear cytoplasmic appreciation on cytology thus increasing its utility in the diagnosis of lung tumors [Figure 4].
Figure 3.
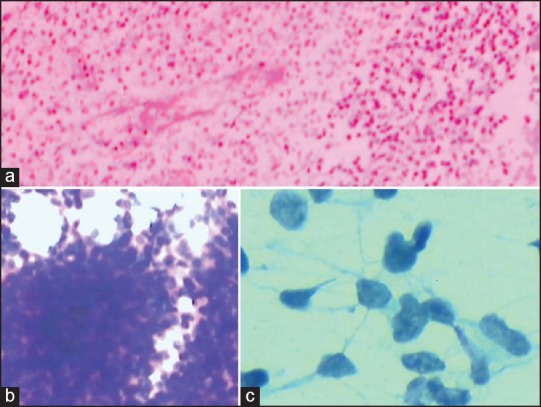
(a) Bronchial biopsy showed only necrosis and was inadequate for diagnosis (H and E, ×40) (b) same case on transbronchial needle aspirate cytology smears showed presence of cellular tumor fragments of primitive neuroectodermal tumor (PNET) (MGG, ×100) (c) Round cells showing nuclei with stippled chromatin and moderate pale cytoplasm in PNET were well appreciated on higher resolution on (Pap, ×400)
Figure 4.
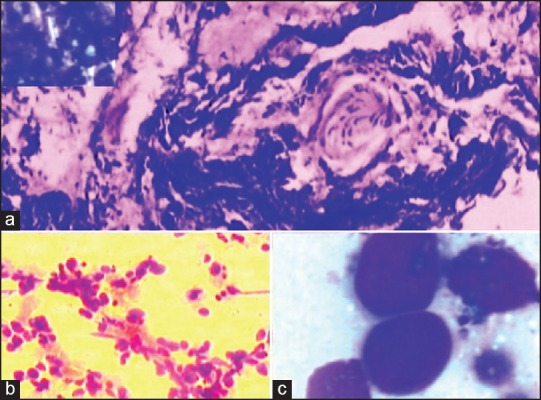
(a) Crush artifact on bronchial biopsy, inadequate for diagnosis (H and E, ×100) (b and c) same case on computed tomography guided fine needle aspiration on cytology smears show small cell carcinoma with evidence of nuclear moulding (b, H and E, ×100; c, MGG, ×400)
However, there were certain important limitations which were observed on cytology in the study. The large reactive endobronchial cells were misdiagnosed as malignant cells and thus giving false positive diagnosis. Aggregates of plump spindle cells or columnar cells were misinterpreted as epithelioid cells or inversely occasional sparse granulomas comprising of few epithelioid cells were missed thus limiting the accuracy of cytology for diagnosis of granulomatous inflammation. In addition, in 15.3% cases malignant cells were missed, and the cases were falsely diagnosed as negative for malignant cells. Cytological smears from BAL were mostly responsible for such type of misdiagnosis.
As molecular analysis was not done and immunocytochemistry was also limited to few cases, so the study does not highlight the advantages of cytology for these ancillary techniques. However, studies have shown the suitability of cytological specimens in immunochemistry mutational and micro RNA analysis for lung cancer but still the authors suggest that further analysis of these techniques on cytological specimens especially in resource limited settings for lung tumor management should be done.[7,9]
Conclusion
The study concludes that cytology is comparable to histology in diagnosis of lung lesions and may even outperform biopsy in lung tumor diagnosis. The advantages of cytology, in addition to being minimally invasive with low complication rate especially in patients with low general condition in lung lesions, may be further added by better sampling and preanalytical assessment for adequate diagnostic material. ROSE has proved to be an important, easy and cost effective adjunct in this regard. A multidisciplinary approach involving pulmonologist, radiologist and cytopathologist with ROSE followed by vigilant morphological examination may increase diagnostic utility of cytology for lung lesions. It is further suggested that studies involving the role of ancillary techniques in cytology may be carried out for lung tumor diagnosis and management especially in resource limited settings.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Travis WD, Brambilla E, Noguchi M, Nicholson AG, Geisinger K, Yatabe Y, et al. Diagnosis of lung cancer in small biopsies and cytology: Implications of the 2011 International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society classification. Arch Pathol Lab Med. 2013;137:668–84. doi: 10.5858/arpa.2012-0263-RA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Langer CJ, Besse B, Gualberto A, Brambilla E, Soria JC. The evolving role of histology in the management of advanced non-small-cell lung cancer. J Clin Oncol. 2010;28:5311–20. doi: 10.1200/JCO.2010.28.8126. [DOI] [PubMed] [Google Scholar]
- 3.Burlingame OO, Kessé KO, Silverman SG, Cibas ES. On-site adequacy evaluations performed by cytotechnologists: Correlation with final interpretations of 5241 image-guided fine-needle aspiration biopsies. Cancer Cytopathol. 2012;120:177–84. doi: 10.1002/cncy.20184. [DOI] [PubMed] [Google Scholar]
- 4.Johnson DH, Fehrenbacher L, Novotny WF, Herbst RS, Nemunaitis JJ, Jablons DM, et al. Randomized phase II trial comparing bevacizumab plus carboplatin and paclitaxel with carboplatin and paclitaxel alone in previously untreated locally advanced or metastatic non-small-cell lung cancer. J Clin Oncol. 2004;22:2184–91. doi: 10.1200/JCO.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 5.Rosell R, Carcereny E, Gervais R, Vergnenegre A, Massuti B, Felip E, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): A multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13:239–46. doi: 10.1016/S1470-2045(11)70393-X. [DOI] [PubMed] [Google Scholar]
- 6.Sindhwani G, Rawat J, Chandra S, Kusum A, Rawat M. Transbronchial needle aspiration with rapid on-site evaluation: A prospective study on efficacy, feasibility and cost effectiveness. Indian J Chest Dis Allied Sci. 2013;55:141–4. [PubMed] [Google Scholar]
- 7.Fassina A, Corradin M, Zardo D, Cappellesso R, Corbetti F, Fassan M. Role and accuracy of rapid on-site evaluation of CT-guided fine needle aspiration cytology of lung nodules. Cytopathology. 2011;22:306–12. doi: 10.1111/j.1365-2303.2010.00802.x. [DOI] [PubMed] [Google Scholar]
- 8.Diacon AH, Theron J, Schubert P, Brundyn K, Louw M, Wright CA, et al. Ultrasound-assisted transthoracic biopsy: Fine-needle aspiration or cutting-needle biopsy? Eur Respir J. 2007;29:357–62. doi: 10.1183/09031936.00077706. [DOI] [PubMed] [Google Scholar]
- 9.Fischer AH, Cibas ES, Howell LP, Kurian EM, Laucirica R, Moriarty AT, et al. Role of cytology in the management of non-small-cell lung cancer. J Clin Oncol. 2011;29:3331–2. doi: 10.1200/JCO.2011.35.2534. [DOI] [PubMed] [Google Scholar]
- 10.Rekhtman N, Brandt SM, Sigel CS, Friedlander MA, Riely GJ, Travis WD, et al. Suitability of thoracic cytology for new therapeutic paradigms in non-small cell lung carcinoma: High accuracy of tumor subtyping and feasibility of EGFR and KRAS molecular testing. J Thorac Oncol. 2011;6:451–8. doi: 10.1097/JTO.0b013e31820517a3. [DOI] [PubMed] [Google Scholar]


