Abstract
Objectives
To quantify national complication rates, perioperative outcomes, and predictors for a broad range of urological procedures to demonstrate background rates and discuss benchmarking.
Methods
Urologic procedures from NSQIP (2006–2011) were analyzed to identify 30-day rates of 21 complications, outcomes (length of stay (LOS), reoperation, death), and predictors including resident involvement for 18 specific procedures. Multivariable logistic regression models assessed predictors for any complication and for Clavien IV or V complication.
Results
A total of 39,700 procedures were included with abdominopelvic operations more morbid than endoscopic, scrotal, incontinence, or prolapse procedures. Cystectomy had the highest morbidity (10.8 days LOS, 3.2% mortality) with 56% experiencing any complication followed by nephrectomy (21%), RPLND (20%), and RRP (19%). TURBT (11%) and TURP (10%) had highest rates for endoscopic procedures. Older age, ASA class, dependent functional status, AKI [OR2.70(1.89–3.87)], and ≥5 units preoperative transfusion [OR4.44(3.40–5.80)] were strongest predictors of any complication. Higher ORs of similar predictors along with COPD [OR1.52(1.21–1.92)] and steroid use [OR1.51(1.07–2.14)] were associated with Clavien IV or V complication. Resident involvement increased odds of any complication [OR1.18(1.09–1.29)], mostly for abdominopelvic and urogynecologic procedures, but not Clavien IV or V complication (p=0.55).
Conclusions
Complication rates of urological procedures based on the retrospective experience of few surgeons does not allow for appropriate benchmarking. Baseline rates and benchmarks derived from NSQIP may help hospitals better track deficient areas and improvements in quality of care. Many predictors were similar across procedures, although magnitudes differed, and resident trainees did not impact rates of serious complications (Clavien-Dindo grade IV or V).
Keywords: complications, quality of care, risk factors, surgical outcomes, urologic surgery
Introduction
As many as 400,000 premature deaths per year in the United States are due to preventable harm in hospitals with 10 to 20-fold greater rates of “serious harm”.1 However, a critical issue in assessing patient safety and complications following surgical procedures is benchmarking: comparison to agreed upon acceptable and expected background rates for complications. Notable variation in complication rates and practice between hospitals and surgeons has been described for urologic cancer surgeries.2,3 Furthermore, even with increased scrutiny on improving the quality of surgical care in the past several years, a recent report suggests the United States may have made no progress in reducing the rate of adverse events after surgery compared to significant reductions in the care of patients with acute myocardial infarctions and congestive heart failure.4
Benchmarking is a prerequisite to identify process deviations in quality of care, especially important because adverse events, preventable or not, may represent 16% of direct hospital costs and Medicare is taking a firmer stance in not paying for preventable complications.5,6 Complication rates and perioperative outcomes for urological procedures are known to evolve along learning curves and hence resident training is also under scrutiny.7–9 Therefore, establishing reliable and comparable background rates of minor and major complications is important followed by appropriate risk-adjustment before improvements in quality of care can be accurately tracked.
Most reports on the complications of urological procedures focus on the retrospective experience of few surgeons performing select operations with various definitions for tracked complications limiting application as comparative quality improvement benchmarks. The goal of the present analysis is to quantify complication rates and perioperative outcomes for a broad range of urological procedures using the National Surgical Quality Improvement Program (NSQIP). We hypothesize predictors will be similar across procedures, including for serious complications (Clavien-Dindo grade IV or V), and that resident trainees will not impact complication rates.
Materials and Methods
Institutional IRB review approved the study. The NSQIP provides voluntary assessment of surgical outcomes for >300 academic and community hospitals across the United States. Preoperative, operative, and 30-day postoperative complication data is collected by trained Surgical Clinical Reviewers using clinical records rather than administrative data. Clinical abstraction is audited and collected for internal quality improvement but de-identified data is made available to researchers. Detailed methods and rationale behind NSQIP have been previously described.10,11
Study Cohort
NSQIP datasets from the years 2006 to 2011 were used to identify patients undergoing common urological procedures by restriction to cases performed by urologic surgeons followed by review of Current Procedural Terminology (CPT) codes (major urological CPT codes between 50010 to 55899; additional urogynecologic procedures 57265 to 57425; adrenal procedures 60540 to 60650; retroperitoneal lymph node dissection (RPLND) 38780). Among all urologic operations, 18 specific procedures were categorized and included in the analysis: radical retropubic prostatectomy (RRP), laparoscopic radical prostatectomy (LRP; includes both robotic (majority) and traditional laparoscopic), transurethral resection of the prostate (TURP), photoselective vaporization of the prostate, total nephrectomy (TN), partial nephrectomy (PN), cystectomy, transurethral resection of bladder tumor (TURBT), radical orchiectomy, spermatocelectomy, hydrocelectomy, varicocelectomy, artificial urinary sphincter, male sling procedure, female sling procedure, colporrhaphy, adrenalectomy, and RPLND.
Variables and Outcomes
Baseline demographics, American Society of Anesthesiologists (ASA) physical status classification system, preoperative risk factors, and outcomes including length of stay (LOS), operative time, death, reoperation, and 21 specific complications were obtained. Preoperative risk factors included comorbidities (COPD, hypertension, diabetes), functional status assessment (independent, partially or totally dependent), recent steroid use, acute kidney injury (AKI), bleeding risk assessment, and preoperative transfusion requirement. The outcomes were 1. any complication (including death) and 2. Clavien-Dindo grade IV or V complication. NSQIP does not employ Clavien grading but grade IV or V was determined using a previously reported algorithm (Clavien IV: postoperative septic shock, postoperative dialysis, PE, prolonged ventilator requirements, need for reintubation, myocardial infarction, and cardiac arrest; Clavien V: mortality).12 Clavien I – III grades could not be determined. Specific complications included superficial surgical site infection (SSI), deep SSI, organ/space SSI, wound dehiscence, pneumonia, reintubation, pulmonary embolism (PE), >48 hour ventilator requirement, renal insufficiency, dialysis requirement, urinary tract infection (UTI), stroke, coma, peripheral nerve injury, cardiac arrest, myocardial infarction, transfusion (≥5 units within 72 hours after operation), graft/prosthesis failure, deep vein thrombosis (DVT), sepsis, and septic shock.
Statistical Analysis
Mean operative time, LOS, and proportion of patients experiencing any complication, reoperation, or death within 30 days of the procedure were assessed. Rates of individual complications were tabulated as proportions by each of the 18 procedures. Multivariable logistic regression models were developed to assess risk factors for the outcomes of interest (described above). Results were adjusted for case-mix except for sex, which could not be adjusted across all procedures as some procedures involved only males or females. Subanalyses also assessed resident trainee involvement and predictors of the most common complications.
Results
Baseline Characteristics
From 2006 to 2011, a total of 48,421 procedures captured by NSQIP were identified with demographics, ASA class, and functional status given by primary organ involved in Supplemental Table 1. The 18 selected procedures comprised 39,700 (82.0%) of the operations as shown in Supplemental Figure 1A with preoperative characteristics listed in Table 1. Overall, a notable proportion of patients had hypertension (56.3%) and diabetes (16.2%) while a smaller fraction were assessed to be a bleeding risk (2.4%) or on recent steroid therapy (2.1%).
Table 1.
Preoperative comorbidities and risk factors by type of procedure, NSQIP 2006–2011.
| Procedurea | Preoperative Characteristicsb | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | (%) | HTN | (%) | DM | (%) | COPD | (%) | Bleeding Risk | (%) | Steroid Use | (%) | Preop Transfusion | (%) | AKI | (%) | |
| RRP | 2,279 | (5.7) | 1,117 | (49.0) | 263 | (11.5) | 53 | (2.3) | 11 | (0.5) | 30 | (1.3) | 6 | (0.3) | 4 | (0.2) |
| LRP | 8,381 | (21.1) | 4,250 | (50.7) | 862 | (10.3) | 161 | (1.9) | 74 | (0.9) | 70 | (0.8) | 6 | (0.1) | 5 | (0.1) |
| TURP | 4,968 | (12.5) | 3,120 | (62.8) | 1,025 | (20.6) | 374 | (7.5) | 162 | (3.3) | 125 | (2.5) | 50 | (1.0) | 26 | (0.5) |
| PVP | 2,853 | (7.2) | 1,764 | (61.8) | 532 | (18.6) | 212 | (7.4) | 120 | (4.2) | 51 | (1.8) | 10 | (0.4) | 13 | (0.5) |
| Total Nephrectomy | 3,988 | (10.0) | 2,580 | (64.7) | 791 | (19.8) | 233 | (5.8) | 125 | (3.1) | 171 | (4.3) | 69 | (1.7) | 30 | (0.8) |
| Partial Nephrectomy | 2,737 | (6.9) | 1,617 | (59.1) | 476 | (17.4) | 131 | (4.8) | 46 | (1.7) | 63 | (2.3) | 6 | (0.2) | 4 | (0.1) |
| Cystectomy | 1,302 | (3.3) | 770 | (59.1) | 251 | (19.3) | 115 | (8.8) | 39 | (3.0) | 38 | (2.9) | 36 | (2.8) | 8 | (0.6) |
| TURBT | 6,881 | (17.3) | 4,395 | (63.9) | 1,440 | (20.9) | 694 | (10.1) | 299 | (4.3) | 192 | (2.8) | 86 | (1.2) | 65 | (0.9) |
| Radical Orchiectomy | 373 | (0.9) | 73 | (19.6) | 32 | (8.6) | 3 | (0.8) | 3 | (0.8) | 6 | (1.6) | 1 | (0.3) | 0 | 0.0 |
| Spermatocelectomy | 395 | (1.0) | 134 | (33.9) | 30 | (7.6) | 16 | (4.1) | 4 | (1.0) | 8 | (2.0) | 0 | 0.0 | 1 | (0.3) |
| Hydrocelectomy | 1,208 | (3.0) | 573 | (47.4) | 168 | (13.9) | 34 | (2.8) | 20 | (1.7) | 20 | (1.7) | 0 | 0.0 | 1 | (0.1) |
| Varicocelectomy | 316 | (0.8) | 28 | (8.9) | 8 | (2.5) | 0 | 0.0 | 1 | (0.3) | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| AUS | 279 | (0.7) | 184 | (65.9) | 56 | (20.1) | 11 | (3.9) | 9 | (3.2) | 6 | (2.2) | 2 | (0.7) | 0 | 0.0 |
| Male sling procedure | 366 | (0.9) | 240 | (65.6) | 56 | (15.3) | 16 | (4.4) | 4 | (1.1) | 7 | (1.9) | 0 | 0.0 | 0 | 0.0 |
| Female sling procedure | 2,616 | (6.6) | 1,100 | (42.0) | 313 | (12.0) | 102 | (3.9) | 19 | (0.7) | 55 | (2.1) | 1 | (0.0) | 0 | 0.0 |
| Colporrhaphy | 528 | (1.3) | 303 | (57.4) | 91 | (17.2) | 13 | (2.5) | 2 | (0.4) | 4 | (0.8) | 0 | 0.0 | 1 | (0.2) |
| Adrenalectomy | 129 | (0.3) | 85 | (65.9) | 24 | (18.6) | 7 | (5.4) | 2 | (1.6) | 2 | (1.6) | 0 | 0.0 | 0 | 0.0 |
| RPLND | 101 | (0.3) | 18 | (17.8) | 4 | (4.0) | 2 | (2.0) | 4 | (4.0) | 3 | (3.0) | 0 | 0.0 | 0 | 0.0 |
| Selected Procedures | 39700 | (100.0) | 22,351 | (56.3) | 6,422 | (16.2) | 2,177 | (5.5) | 944 | (2.4) | 851 | (2.1) | 273 | (0.7) | 158 | (0.4) |
RRP = radical retropubic prostatectomy; LRP = laparoscopic radical prostatectomy; TURP = transurethral resection of the prostate; PVP photoelective vaporization of the prostate; TURBT = transurethral resection of bladder tumor; AUS = artificial urinary sphincter; RPNLD = retroperitoneal lymph node dissection
HTN = hypertension; DM = diabetes mellitus; COPD = chronic obstructive pulmonary disease; AKI = acute kidney injury
Outcomes
Abdominopelvic operations were more morbid than endoscopic, scrotal, incontinence, or prolapse procedures. Outcomes in Table 2 show cystectomy had the highest morbidity (10.75 days LOS, 3.23% 30-day mortality) with a 56.3% rate of any complication followed by total nephrectomy (20.6%), RPLND (19.8%) and RRP (19.4%). Amongst non-abdominopelvic procedures, rates were highest for TURBT (10.6%) and TURP (10.1%). Overall composition of specific complications displayed in Supplemental Figure 1B is tabulated in a supplement as absolute rates by procedure (Supplemental Table 2). Transfusion requirements ≥5 units within 72 hours of the case [1741 (30.7%)] and UTIs [1242 (21.9%)] were the most common complications followed by SSIs [519 (9.1%)], sepsis [413 (7.3%)], thromboembolic events [369 (6.5%)], and pneumonia [239 (4.2%)]. Each procedure was associated with a unique rate and relative array of complications.
Table 2.
Operative time and major perioperative outcomes by type of procedures, NSQIP 2006–2011.
| Procedurea | Perioperative Outcomesb | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | (%) | Operative Time | (SD) | LOS | (SD) | Any Complication | (%) | Reoperation | (%) | Death | (%) | |
| RRP | 2,279 | (5.7) | 176 | (81) | 3.01 | (3.27) | 443 | (19.44) | 34 | (1.49) | 8 | (0.35) |
| LRP | 8,381 | (21.1) | 211 | (74) | 1.81 | (4.05) | 515 | (6.14) | 89 | (1.06) | 9 | (0.11) |
| TURP | 4,968 | (12.5) | 54 | (37) | 2.42 | (6.03) | 504 | (10.14) | 109 | (2.19) | 31 | (0.62) |
| PVP | 2,853 | (7.2) | 56 | (37) | 0.87 | (3.56) | 240 | (8.41) | 41 | (1.44) | 13 | (0.46) |
| Total Nephrectomy | 3,988 | (10.0) | 177 | (92) | 5.04 | (5.49) | 823 | (20.64) | 116 | (2.91) | 45 | (1.13) |
| Partial Nephrectomy | 2,737 | (6.9) | 193 | (77) | 3.96 | (3.24) | 410 | (14.98) | 70 | (2.56) | 14 | (0.51) |
| Cystectomy | 1,302 | (3.3) | 347 | (130) | 10.75 | (8.56) | 733 | (56.30) | 75 | (5.76) | 42 | (3.23) |
| TURBT | 6,881 | (17.3) | 35 | (35) | 1.18 | (6.53) | 731 | (10.62) | 291 | (4.23) | 84 | (1.22) |
| Radical Orchiectomy | 373 | (0.9) | 57 | (60) | 0.83 | (3.07) | 14 | (3.75) | 5 | (1.34) | 1 | (0.27) |
| Spermatocelectomy | 395 | (1.0) | 43 | (24) | 0.28 | (4.67) | 4 | (1.01) | 2 | (0.51) | 0 | 0.00 |
| Hydrocelectomy | 1,208 | (3.0) | 44 | (24) | 0.13 | (0.88) | 42 | (3.48) | 15 | (1.24) | 0 | 0.00 |
| Varicocelectomy | 316 | (0.8) | 61 | (36) | 0.05 | (0.32) | 4 | (1.27) | 2 | (0.63) | 1 | (0.32) |
| AUS | 279 | (0.7) | 96 | (34) | 1.07 | (0.64) | 22 | (7.89) | 12 | (4.30) | 2 | (0.72) |
| Male sling procedure | 366 | (0.9) | 78 | (31) | 0.44 | (0.56) | 13 | (3.55) | 3 | (0.82) | 0 | 0.00 |
| Female sling procedure | 2,616 | (6.6) | 50 | (46) | 0.53 | (1.20) | 117 | (4.47) | 22 | (0.84) | 0 | 0.00 |
| Colporrhaphy | 528 | (1.3) | 81 | (49) | 1.06 | (0.79) | 37 | (7.01) | 8 | (1.52) | 0 | 0.00 |
| Adrenalectomy | 129 | (0.3) | 168 | (73) | 4.43 | (6.58) | 14 | (10.85) | 3 | (2.33) | 0 | 0.00 |
| RPLND | 101 | (0.3) | 292 | (116) | 5.47 | (2.64) | 20 | (19.80) | 5 | (4.95) | 0 | 0.00 |
| Selected Procedures | 39700 | (100.0) | - | - | - | 4686 | (11.80) | 902 | (2.27) | 250 | (0.63) | |
RRP = radical retropubic prostatectomy; LRP = laparoscopic radical prostatectomy; TURP = transurethral resection of the prostate; PVP photoselective vaporization of the prostate; TURBT = transurethral resection of bladder tumor; AUS = artificial urinary sphincter; RPNLD = retroperitoneal lymph node dissection
SD = standard deviation; LOS = length of stay
Predictors of Complications
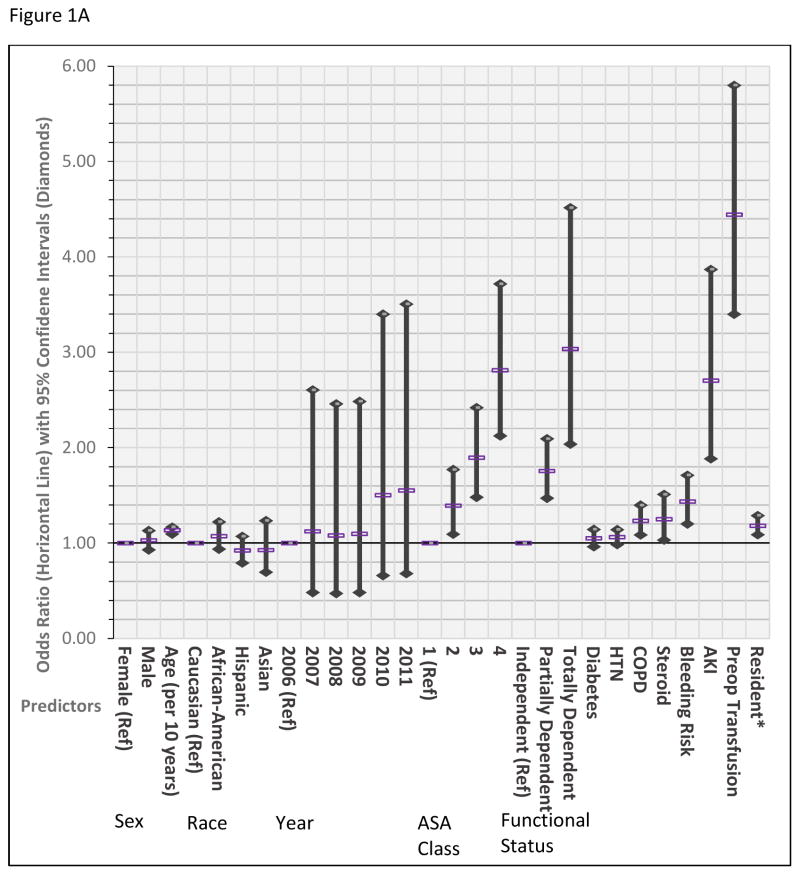
Figure 1 and Table 3 show the results of the case-mix adjusted multivariable logistic regression models. For the outcome of any complication, older age [OR 1.73 (1.47–2.02) for octogenarians compared to <50 years], increasing ASA class, dependent functional status, and preoperative risk factors including history of COPD [OR 1.23 (1.09–1.40)], steroid use [OR 1.25 (1.03–1.51)], AKI [OR 2.70 (1.89–3.87)], bleeding risk [OR 1.44 (1.20–1.71)], and ≥5 units preoperative transfusion [OR 4.44 (3.40–5.80)] were associated with increased risk of experiencing a complication. Associations with experiencing a Clavien IV or V revealed higher ORs for age, ASA class, functional status, COPD, steroid use, and AKI. Associations with bleeding risk and preoperative transfusion were diminished as postoperative transfusion did not qualify as a Clavien IV or V complication.
Figure 1.
Adjusted multivariable analysis assessing for predictors for the outcomes of any complication (A) as well as for Clavien IV or V complication (B) among urological procedures, NSQIP 2006–2011. AKI = acute kidney injury, COPD = chronic obstructive pulmonary disease, HTN = hypertension. *= derived from subset analysis of 77% of procedures including data on resident assistance. Reference set at y=1.00.
Table 3.
Adjusted multivariable analysis assessing for predictors for the outcomes of any complication as well as for Clavien IV or V complication among urological procedures, NSQIP 2006–2011.
| Adjusted Multivariable Analysis | Any Complicationa 95% CI |
Clavien IV or V Complicationa 95% CI |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variableb | OR | Low | High | p-value | OR | Low | High | p-value | |
| Sex | Female | Reference | Reference | ||||||
| Male | 1.03 | 0.93 | 1.13 | 0.59 | 1.37 | 1.11 | 1.69 | <0.01 | |
| Age | <50 | Reference | Reference | ||||||
| 50–59 | 1.11 | 0.96 | 1.29 | 0.14 | 1.57 | 1.04 | 2.39 | 0.03 | |
| 60–69 | 1.16 | 1.01 | 1.33 | <0.01 | 1.72 | 1.15 | 2.56 | 0.01 | |
| 70–79 | 1.35 | 1.17 | 1.55 | <0.01 | 2.70 | 1.81 | 4.03 | <0.01 | |
| ≥80 | 1.73 | 1.47 | 2.02 | <0.01 | 3.98 | 2.62 | 6.04 | <0.01 | |
| Race | Caucasian | Reference | Reference | ||||||
| African-American | 1.07 | 0.94 | 1.22 | 0.30 | 1.22 | 0.92 | 1.61 | 0.17 | |
| Hispanic | 0.92 | 0.79 | 1.07 | 0.29 | 0.71 | 0.48 | 1.04 | 0.08 | |
| Asian | 0.93 | 0.70 | 1.24 | 0.61 | 0.90 | 0.45 | 1.78 | 0.76 | |
| Year | 2006 | Reference | Reference | ||||||
| 2007 | 1.12 | 0.48 | 2.61 | 0.79 | 0.79 | 0.10 | 6.41 | 0.82 | |
| 2008 | 1.08 | 0.47 | 2.46 | 0.86 | 1.58 | 0.21 | 11.95 | 0.66 | |
| 2009 | 1.10 | 0.48 | 2.49 | 0.83 | 1.57 | 0.21 | 11.80 | 0.66 | |
| 2010 | 1.50 | 0.66 | 3.40 | 0.33 | 1.30 | 0.17 | 9.74 | 0.80 | |
| 2011 | 1.55 | 0.68 | 3.51 | 0.29 | 1.35 | 0.18 | 10.10 | 0.77 | |
| ASA Class | 1 | Reference | Reference | ||||||
| 2 | 1.39 | 1.09 | 1.77 | 0.01 | 4.13 | 1.01 | 16.90 | 0.05 | |
| 3 | 1.89 | 1.48 | 2.42 | <0.01 | 8.03 | 1.96 | 32.83 | <0.01 | |
| 4 | 2.81 | 2.13 | 3.72 | <0.01 | 13.72 | 3.30 | 57.11 | <0.01 | |
| Functional Status | Independent | Reference | Reference | ||||||
| Partially Dependent | 1.76 | 1.47 | 2.09 | <0.01 | 2.31 | 1.72 | 3.11 | <0.01 | |
| Totally Dependent | 3.03 | 2.04 | 4.52 | <0.01 | 6.76 | 4.06 | 11.26 | <0.01 | |
| COPD | 1.23 | 1.09 | 1.40 | <0.01 | 1.52 | 1.21 | 1.92 | <0.01 | |
| Steroid | 1.25 | 1.03 | 1.51 | 0.02 | 1.51 | 1.07 | 2.14 | 0.02 | |
| AKI | 2.70 | 1.89 | 3.87 | <0.01 | 3.38 | 2.01 | 5.69 | <0.01 | |
| Bleeding Risk | 1.44 | 1.20 | 1.71 | <0.01 | 1.22 | 0.86 | 1.74 | 0.26 | |
| Preop Transfusion | 4.44 | 3.40 | 5.80 | <0.01 | 1.64 | 1.03 | 2.62 | 0.04 | |
| HTN | 1.06 | 0.99 | 1.14 | 0.11 | 1.06 | 0.89 | 1.26 | 0.49 | |
| Diabetes | 1.05 | 0.96 | 1.15 | 0.26 | 1.13 | 0.10 | 1.35 | 0.94 | |
|
| |||||||||
| Residentc | Not case-mix adjusted | 1.43 | 1.34 | 1.53 | <0.01 | 1.62 | 1.39 | 1.90 | <0.01 |
| Residentc | Case-mix adjusted | 1.18 | 1.09 | 1.29 | <0.01 | 1.06 | 0.88 | 1.28 | 0.55 |
| Scrotal | 0.98 | 0.54 | 1.77 | 0.95 | N/A | ||||
| Transurethral | 1.01 | 0.88 | 1.18 | 0.84 | 0.88 | 0.61 | 1.29 | 0.53 | |
| Urogynecologic | 1.70 | 1.18 | 2.45 | <0.01 | N/A | ||||
| Abdominopelvic | 1.23 | 1.10 | 1.38 | <0.01 | 1.12 | 0.88 | 1.41 | 0.36 | |
Also adjusted for case-mix of procedures; 95% CI = 95% confidence interval; OR = odds ratio
ASA = American Society of Anesthesiologists; COPD = chronic obstructive pulmonary disease; AKI = acute kidney injury; HTN = hypertension
Subset analysis of 77% of procedures including data on resident assistance; abdominopelvic includes prostatectomy, nephrectomy, and cystectomy; scrotal and urogynecologic surgeries had too small of a sample size and low rate of Clavien 4 or 5 complications to analyze.
The strongest predictors of postoperative transfusion, the most common complication, included preoperative transfusion [OR 10.19 (7.38–14.06)], bleeding risk, ASA class, age, and female sex. Procedure type was the most predictive of UTIs, which was not associated with any preoperative characteristics except ASA class and age. Notably, for 77% of procedures with data on resident assistance with the case, resident involvement was associated with increased odds of any complication [OR 1.18 (1.09–1.29), p<0.01] but not with outcome of Clavien IV or V complication [(OR 1.06 (0.88–1.28), p=0.55] after adjusting for case-mix (Table 3). The increased odds appeared limited to urogynecologic [OR 1.70 (1.18–2.45)] and major abdominopelvic procedures (nephrectomy, prostatectomy, cystectomy) [OR 1.23 (1.10–1.38)]. The number of hospitals capturing data on urological procedures increased significantly between 2006 and 2011, accounting for great variance in comparisons between years although none were statistically significant.
Comment
NSQIP was utilized to report on the unique array of complications and perioperative outcomes for 18 specific urological procedures across >300 hospitals in >40 states of the United States. As hypothesized, similar independent preoperative risk factors associated with the occurrence of any complication as well as Clavien IV or V complications were identified across procedures. However, important differences in magnitude existed. Cystectomy was associated with the greatest rate of complications, transfusion requirement (≥5 units postoperatively) and UTIs were the most common complications, and, contrary to our hypothesis, the presence of resident trainees in cases was associated with increased occurrence of any complication but not with serious complications.
Benchmarking is an important starting point toward measuring health quality in the perioperative setting – a setting in which “preventable” is very difficult to define.13 Risk-adjustment tools have thus far proved imperfect in making comparisons between hospitals and individuals. One other route of actionable health policy might be to focus on reducing unwarranted variation in care around risk-adjusted benchmarks.3 Additionally, NSQIP may compare and track rates of adverse events associated with surgical interventions for quality improvement initiatives or evolving surgical technologies in urology shifting practice patterns to minimally-invasive and robotic techniques.14 With potentially equivalent efficacy for disease treatment, increased costs of new technology might be offset by improved quality of care and decreased complication rates. Health policy measures will be key as a recent study indicates hospitals in the United States may actually receive marginally higher per-encounter hospital contribution margins from Medicare and private insurance for having postoperative complications – an incentive against quality improvement and extra reason to push for benchmarking.15
Although previous studies are less generalizable reporting on the experience of one surgeon with series varying from less than 20 procedures to about 100 procedures, it is illustrative to compare complication rates captured by NSQIP to those previously reported. The overall rate of 15% for PN compares reasonably with 15–17% noted for laparoscopic and robotic PN.16 A large single-surgeon series notes rates of 41% and 59% for open and robotic cystectomy, respectively, and multi-institutional experience of 65% compared to 56% reported here.17.18 A report on scrotal surgery for benign conditions showed reports on complication rates varied widely, from 0.7% to 91.7% up to the year 2007, due to inconsistent reporting windows (30-day vs. 90-day vs. years of follow-up) and the types of complications included making comparisons difficult.19 We report 30-day perioperative complication rates of 1.01%, 1.27%, and 3.48% for spermatocelectomy, varicocelectomy, and hydrocelectomy, respectively.
Few NSQIP studies have previously looked at urological procedures. A report by Hollenbeck et al. on TURBT rates up to 2002 including only Veterans Affairs hospitals with a limited array of complications has been updated here. They reported rates of overall complications, UTIs, and mortality of 4.3%, 3.0%, and 1.3%, respectively, compared to our update of 10.6%, 3.7%, and 1.2%.20 Tyson et al. report only on the rates of thromboembolic events, including DVT and PE rates of 4.0% and 2.9% for cystectomy compared to our 4.1% and 3.2%, respectively.21 Finally, two recently published comparative reports attempt to compare minimally-invasive surgery for prostatectomy and nephrectomy to their open counterparts.22,23 While trends in safety over time, demonstrated by Liu et al., are an admirable application of NSQIP, direct comparisons between these procedures may be more limited until specific disease characteristics are obtainable through NSQIP or clinical practice evolves to a point that selection bias is less of a concern.
Both prospective tracking of complications for NSQIP by full-time Surgical Clinical Reviewers, most often nurses, and auditing of reported data has allowed robust reporting of complication rates. Therefore, rates for individual complications may be higher and more accurate than represented in the retrospective literature. Other notable findings in the study also benefit from methodology employed by NSQIP. While racial disparities are often present in obtaining healthcare, there appears to be no inherent racial disparity or predisposition to complications after undergoing a urological procedure. As may be expected, increased age and comorbidity (reflected by ASA class) were associated with somewhat increased risk of experiencing a complication. However, risk of serious complications was dramatically increased with age [OR 1.43 (1.32–1.54) per 10 years] and ASA class (ORs ~4, 8, and 14 for ASA 2, 3, and 4 compared to 0) indicating better selection and frailty measures are needed for these populations to balance the benefits and risks of surgery. Sex, as previously mentioned, cannot be interpreted in the overall fashion as case-mix adjustment is not possible for procedures performed on only males or females.
Notably, resident involvement was associated with increased odds of any complication [OR 1.18 (1.09–1.29)] but not Clavien IV or V complication [(OR 1.06 (0.88–1.28)]. Balancing patient safety and resident training is a critical issue for all teaching hospitals. Case-mix adjustment for procedures was key as the unadjusted association of resident involvement with serious complication was substantial [1.62 (1.39–1.90)]. Resident involvement may increase the overall rate of complications either directly, through technical errors or insufficient supervision, but also possibly indirectly as a consequence of increased operative time.24 If the former is a major contributor, the results may support a more structured approach to help residents reduce the learning curve associated with each procedure. At the same time, it is possible case-mix adjustment for procedures is not sufficient if resident involvement is a surrogate for academic centers where case-mix of disease characteristics is substantially different for any given procedure. A stratified approach revealed the increased odds of complications appeared limited to urogynecologic [OR 1.70 (1.18–2.45)] and major abdominopelvic procedures (nephrectomy, prostatectomy, cystectomy) [OR 1.23 (1.10–1.38)] and did not apply to scrotal or transuretheral surgeries.
The current study has important limitations and advantages which should be summarized. The main limitation applicable to the current analysis is deidentification of sensitive data on morbidity and mortality, required by the data use agreement, so that hospital volume and individual surgeon characteristics cannot be analyzed for impact on perioperative outcomes and complication rates. While this limits some comparisons based on surgeon experience and setting, it protects integrity of data initially intended for internal evaluation and improvement. Notably, because of this the data is collected in an audited fashion using clinical records and is not administrative. Another limitation is the lack of some procedure-specific complications as NSQIP standardizes complication reporting. However, although it is a trade-off, there is value in tracking a comparable array of outcomes and complications across procedures for quality improvement. Hospitals may choose to internally track some procedure-specific complications, and one important potential area of improvement, albeit labor-intensive as NSQIP requires clinical abstraction, is to include an important agreed upon procedure-specific complication for each index procedure into the Participant Use Data File.
Notwithstanding the limitations, we have reported on complications and perioperative outcomes for a broad range of urological procedures using NSQIP and identified important predictors of complications including the effect of trainees in urology. The array of complications and perioperative outcomes for urological procedures is specific to each type of procedure with significant variation in morbidity and mortality.
Conclusions
NSQIP provides a tool for benchmarking adverse events associated with surgical interventions. We identified comparable background rates of complications from a national quality improvement program along with independent preoperative risk factors associated with the occurrence of complications including Clavien IV or V complications. Resident trainees were associated with slightly increased occurrence of any complication for abdominopelvic and urogynecologic procedures but not with serious complications. Removal of financial incentives to have complications, compliance with safety practice, and attention to risk-adjusting quality of care will be vital to overcoming the lack of progress we have made in reducing rates of adverse events after surgery. Through research and technology, urologists will continue to play an important role in improving the quality of surgical care.
Supplementary Material
Supplemental Figure. The relative proportion of procedures (A) and complications (B) among the eighteen selected index urological procedures. AUS = artificial urinary sphincter, DVT = deep vein thrombosis, PVP = photoselective vaporization of the prostate, RPLND = retroperitoneal lymph node dissection, RRP = radical retropubic prostatectomy, SSI = surgical site infection, TURBT = transurethral resection of bladder tumor, TURP = transurethral resection of the prostate.
Supplemental Table 1. Demographics and baseline characteristics of patients undergoing urological procedures, NSQIP 2006–2011.
Supplemental Table 2. Overall rates of complications for the eighteen selected index procedures, NSQIP 2006–2011.
Acknowledgments
This project was supported, in part, by the Predoctoral Clinical Research Training Program and the Johns Hopkins Institute for Clinical and Translational Research (ICTR), which is funded in part by Grant Number UL1 TR 000424-06 from the National Center for Advancing Translational Sciences (NCATS) a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research.
Abbreviations and Acronyms
- AKI
acute kidney injury
- ASA
American Society of Anesthesiologists
- COPD
chronic obstructive pulmonary disorder
- DVT
deep vein thrombosis
- OR
odds ratio
- LOS
length of stay
- LRP
laparoscopic radical prostatectomy
- NSQIP
National Surgical Quality Improvement Program
- PE
pulmonary embolism
- PN
partial nephrectomy
- RPLND
retroperitoneal lymph node dissection
- RRP
radical retropubic prostatectomy
- SSI
surgical site infection
- TN
total nephrectomy
- TURBT
transurethral resection of bladder tumor
- TURP
transurethral resection of the prostate
- UTI
urinary tract infection
Footnotes
Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the Johns Hopkins ICTR, NCATS or NIH.
Disclosures:
The authors declare no disclosures associated with this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.James JT. A new, evidence-based estimate of patient harms associated with hospital care. J Patient Saf. 2013;9:122–8. doi: 10.1097/PTS.0b013e3182948a69. [DOI] [PubMed] [Google Scholar]
- 2.Gore JL, Wright JL, Daratha KB, et al. Hospital-level variation in the quality of urologic cancer surgery. Cancer. 2012;118:987–96. doi: 10.1002/cncr.26373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel HD, Humphreys E, Trock BJ, Han M, Carter HB. Practice patterns and individual variability of surgeons performing radical prostatectomies at a high volume academic center. J Urol. 2014 doi: 10.1016/j.juro.2014.08.101. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 4.Wang Y, Eldridge N, Metersky ML, et al. National trends in patient safety for four common conditions, 2005–2011. N Engl J Med. 2014;370:341–51. doi: 10.1056/NEJMsa1300991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pronovost PJ, Goeschel CA, Wachter RM. The wisdom and justice of not paying for “preventable complications”. JAMA. 2008;299:2197–9. doi: 10.1001/jama.299.18.2197. [DOI] [PubMed] [Google Scholar]
- 6.Ehsani JP, Jackson T, Duckett SJ. The incidence and cost of adverse events in Victorian hospitals 2003–04. Med J Aust. 2006;184:551–5. doi: 10.5694/j.1326-5377.2006.tb00378.x. [DOI] [PubMed] [Google Scholar]
- 7.Pierorazio PM, Patel HD, Feng T, et al. Robotic-assisted versus traditional laparoscopic partial nephrectomy: comparison of outcomes and evaluation of learning curve. Urology. 2011;78:813–9. doi: 10.1016/j.urology.2011.04.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel VR, Tully AS, Holmes R, et al. Robotic radical prostatectomy in the community setting--the learning curve and beyond: initial 200 cases. J Urol. 2005;174:269–72. doi: 10.1097/01.ju.0000162082.12962.40. [DOI] [PubMed] [Google Scholar]
- 9.Bianco FJ, Jr, Riedel ER, Begg CB, et al. Variations among high volume surgeons in the rate of complications after radical prostatectomy: further evidence that technique matters. J Urol. 2005;173:2099–103. doi: 10.1097/01.ju.0000158163.21079.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Henderson WG, Daley J. Design and statistical methodology of the National Surgical Quality Improvement Program: why is it what it is? Am J Surg. 2009;198:S19–27. doi: 10.1016/j.amjsurg.2009.07.025. [DOI] [PubMed] [Google Scholar]
- 11.Cohen ME, Ko CY, Bilimoria KY, et al. Optimizing ACS NSQIP Modeling for evaluation of surgical quality and risk: Patient risk adjustment, procedure mix adjustment, shrinkage adjustment, and surgical focus. J Am Coll Surg. 2013;217:336–46. doi: 10.1016/j.jamcollsurg.2013.02.027. [DOI] [PubMed] [Google Scholar]
- 12.Obeid NM, Azuh O, Reddy S, et al. Predictors of critical care-related complications in colectomy patients using the National Surgical Quality Improvement Program: exploring frailty and aggressive laparoscopic approaches. J Trauma Acute Care Surg. 2012;72:878–83. doi: 10.1097/TA.0b013e31824d0f70. [DOI] [PubMed] [Google Scholar]
- 13.Pronovost PJ, Thompson DA, Holzmueller CG, et al. Defining and measuring patient safety. Crit Care Clin. 2005;21:1–19. doi: 10.1016/j.ccc.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 14.Patel HD, Mullins JK, Pierorazio PM, et al. Trends in renal surgery: robotic technology is associated with increased use of partial nephrectomy. J Urol. 2013;189:1229–35. doi: 10.1016/j.juro.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 15.Eappen S, Lane BH, Rosenberg B, et al. Relationship between occurrence of surgical complications and hospital finances. JAMA. 2013;309:1599–606. doi: 10.1001/jama.2013.2773. [DOI] [PubMed] [Google Scholar]
- 16.Mullins JK, Feng T, Pierorazio PM, et al. Comparative analysis of minimally invasive partial nephrectomy techniques in the treatment of localized renal tumors. Urology. 2012;80:316–21. doi: 10.1016/j.urology.2012.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ng CK, Kauffman EC, Lee MM, et al. A comparison of postoperative complications in open versus robotic cystectomy. Eur Urol. 2010;57:274–81. doi: 10.1016/j.eururo.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 18.De Nunzio C, Cindolo L, Leonardo C, et al. Analysis of radical cystectomy and urinary diversion complications with the Clavien classification system in an Italian real life cohort. Eur J Surg Oncol. 2013;39:792–8. doi: 10.1016/j.ejso.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 19.Swartz MA, Morgan TM, Krieger JN. Complications of scrotal surgery for benign conditions. Urology. 2007;69:616–9. doi: 10.1016/j.urology.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 20.Hollenbeck BK, Miller DC, Taub D, et al. Risk factors for adverse outcomes after transurethral resection of bladder tumors. Cancer. 2006;106:1527–35. doi: 10.1002/cncr.21765. [DOI] [PubMed] [Google Scholar]
- 21.Tyson MD, Castle EP, Humphreys MR, et al. Venous Thromboembolism after Urological Surgery. J Urol. 2014;192:793–7. doi: 10.1016/j.juro.2014.02.092. [DOI] [PubMed] [Google Scholar]
- 22.Liu JJ, Leppert JT, Maxwell BG, et al. Trends and perioperative outcomes for laparoscopic and robotic nephrectomy using the National Surgical Quality Improvement Program (NSQIP) database. Urol Oncol. 2014;32:473–9. doi: 10.1016/j.urolonc.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 23.Pilecki MA, McGuire BB, Jain U, Kim JY, Nadler RB. National multi-institutional comparison of 30-day postoperative complication and readmission rates between open retropubic radical prostatectomy and robot-assisted laparoscopic prostatectomy using NSQIP. J Endourol. 2014;28:430–6. doi: 10.1089/end.2013.0656. [DOI] [PubMed] [Google Scholar]
- 24.Procter LD, Davenport DL, Bernard AC, Zwischenberger JB. General surgical operative duration is associated with increased risk-adjusted infectious complication rates and length of hospital stay. J Am Coll Surg. 2010;210:60–5. doi: 10.1016/j.jamcollsurg.2009.09.034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure. The relative proportion of procedures (A) and complications (B) among the eighteen selected index urological procedures. AUS = artificial urinary sphincter, DVT = deep vein thrombosis, PVP = photoselective vaporization of the prostate, RPLND = retroperitoneal lymph node dissection, RRP = radical retropubic prostatectomy, SSI = surgical site infection, TURBT = transurethral resection of bladder tumor, TURP = transurethral resection of the prostate.
Supplemental Table 1. Demographics and baseline characteristics of patients undergoing urological procedures, NSQIP 2006–2011.
Supplemental Table 2. Overall rates of complications for the eighteen selected index procedures, NSQIP 2006–2011.