Abstract
Background
This study aims to compare surgical outcomes of severe carpal tunnel syndrome (CTS) treated with mini-incision versus extensile release.
Methods
The method employed in this study was a retrospective review of patients with severe CTS, defined by electrophysiologic studies showing non-recordable distal sensory latency of the median nerve. Patients underwent either a mini-incision (2 cm) release of the transverse carpal ligament (group 1) or extensile release proximal to the wrist flexion crease (group 2). Exclusion criteria included prior carpal tunnel release, use of muscle flap, multiple concurrent procedures, or a prior diagnosis of peripheral neuropathy. Group 1 included 70 wrists (40 females, 30 males). Group 2 included 64 wrists (35 females, 29 males). Reported outcomes included pre- and post-operative grip strength as well as Boston Carpal Tunnel Questionnaires (BCTQ).
Results
Patients in group 1 had a 22.6 % increase in grip strength postoperatively (4.5 months ± 5.0), while patients in group 2 had a 59.3 % increase (10.0 months ± 6.9). BCTQ surveys from group 1 (n = 46) demonstrated a symptom severity score of 12.93 and functional status score of 9.39 at an average follow-up of 41.9 ± 10.6 months. Group 2 (n = 42) surveys demonstrated averages of 12.88 and 9.10 at 43.1 ± 11.6 months. One patient in the mini-incision cohort required revision surgery after 2 years, while no patient in the extended release cohort underwent revision.
Conclusion
No significant differences between the two procedures with regard to patient-rated symptom severity or functional status outcomes were found. Both techniques were demonstrated to be effective treatment options for severe CTS.
Keywords: Extensile release, Mini-incision, Outcomes, Severe carpal tunnel syndrome
Introduction
The diagnosis of severe carpal tunnel syndrome (CTS) can be made with a combination of clinical and electrophysiological examinations. When considering nerve conduction studies (NCS), severe CTS has been classically defined as a non-recordable distal sensory latency along with an increased distal motor latency [5]. Patients with advanced CTS have been demonstrated to respond poorly to conservative therapies, and surgical release of the transverse carpal ligament (TCL) is considered as the most reliable treatment method. A wide variety of surgical techniques have been described for CTS [1, 2, 6, 14, 15, 26, 35]. However, as of yet, no strong data have suggested that any one approach is superior to the others [4, 10, 13, 15, 19, 23, 32, 34]. This ambiguity extends to the treatment of severe CTS patients as well.
In Phalen’s landmark study defining CTS, all patients were treated with an extensile surgical approach. Although electrodiagnostic testing was not included in his paper, the majority of patients would be defined in today’s terms as having severe CTS based on his clinical observations [29]. Since then, the size of the skin incision has progressively diminished, and most surgeons now favor a more limited approach [20, 33]. When considering severe CTS though, it is possible that median nerve compression might not be restricted to the carpal tunnel alone and that there may be more proximal nerve compression present. In these cases, an extensile technique could allow improved visualization proximally and further decompression of the median nerve, along with the release of any potential pseudoneuroma. In accordance with this, a cadaver study by Means et al. suggested that some amount of forearm fascia release proximal to the wrist flexion crease is necessary to avoid pathologic post-operative pressures on the median nerve [25]. Clinical outcome studies pertaining specifically to severe CTS are notably lacking, however, and to our knowledge no clinical study exists that assesses the potential influence of incision size in patients with electrophysiologically severe carpal tunnel syndrome.
Given the limited data on severe CTS outcomes in the current literature as outlined in the preceding discussion, the present study aims to evaluate the efficacy of mini-open (2 cm) carpal tunnel release compared to extended open release in treating patients with electrodiagnostically confirmed severe CTS. We hypothesize that a mini-open technique may be as equally effective as an extended open technique in relieving symptoms and restoring functionality in patients with severe CTS.
Materials and Methods
Patients
This study was Institutional Review Board-approved. A retrospective review of all patients treated surgically for severe CTS at our institution from January 2008 to June 2012 was performed. Patients were considered for inclusion if they were 18 years or older, had a diagnosis of severe CTS, and underwent either a mini- (2 cm) incision or extended incision. Patients were excluded from the study if they had a diagnosis of peripheral neuropathy, prior carpal tunnel release, use of muscle flap, or multiple concurrent procedures on the same hand. Severe CTS was defined by electrodiagnostic studies as showing a non-recordable distal sensory latency and prolonged motor nerve latency of the median nerve (>4.2 ms). Only electrophysiologic criteria were utilized in order to provide a standardized value by which to classify the patients’ carpal tunnel severity.
All patients underwent a thorough history and physical examination as part of the standard pre-operative diagnostic workup, including electrodiagnostic testing and grip strength analysis. Findings from special physical examination maneuvers such as Phalen’s test or Tinel’s sign were recorded prospectively at the time of initial visit.
Based on the information collected from chart review, patients were organized into two groups: those who underwent the mini-incision surgery (group 1) and those patients who underwent an extended open release in which the incision continued proximal to the wrist flexion crease (group 2). All mini-incision surgeries were performed by one surgeon, while all extensile open surgeries were performed by a second surgeon.
All charts were reviewed for patient demographics, pre-operative electromyographic (EMG) findings, surgical technique, intra-operative findings, concurrent operations, pre- and post-operative grip strengths, and post-operative complications. Grip strengths of the operative and contralateral hands were measured pre- and post-operatively by a physician or physical therapist by means of a JAMAR hydraulic hand dynamometer (Sammons Preston, Bolingbrook, IL, USA). Grip strength was reported as a percentage change from pre- to post-operative measurements. At a minimum of 1 year post-operatively, each patient was contacted by telephone in order to complete the Boston Carpal Tunnel Questionnaire (BCTQ) [21]. Patients in either group were considered to have a failed surgical result if persisting symptoms post-operatively necessitated the performance of a secondary surgery.
Surgical Technique
All surgeries were performed as outpatient procedures under local or regional anesthesia using a non-sterile pneumatic tourniquet on the upper arm with loupe magnification. Patients in group 1 underwent mini-open carpal tunnel release by one of the authors. This is the standard of care for all CTS patients treated by this surgeon, regardless of patient comorbidities or CTS severity. A longitudinal incision no greater than 2 cm in length was performed in line with the fourth ray, extending to but not crossing the distal wrist crease, and the TCL was divided (Fig. 1). After releasing the TCL, the distal end of the forearm fascia was also released, utilizing a push–cut technique. No ancillary procedures such as internal neurolysis or tenosynovectomy were performed. Once certain that the carpal tunnel was fully released, the tourniquet was deflated, hemostasis was achieved, and the skin incision was closed with monofilament non-absorbable sutures. Patients in group 2 underwent extended open carpal tunnel release by a separate author. Any patient with a non-recordable distal sensory latency cared for by this author received an extended incision, regardless of any other demographic factors. A skin incision was made beginning at Kaplan’s cardinal line distally and carried across the distal wrist crease in zigzag fashion, extending the incision approximately 2–4 cm proximal from the distal wrist crease (Fig. 2). The TCL and distal volar forearm fascia were released under direct observation, tenosynovectomy was performed, and any evidence of nerve damage or pseudoneuroma was addressed. Internal neurolysis was not carried out. Upon complete decompression of the median nerve, the tourniquet was deflated, hemostasis was achieved, and the incision was closed with non-absorbable sutures. The operative hand was then placed in a splint for approximately 1 week or until the first post-operative visit.
Fig. 1.
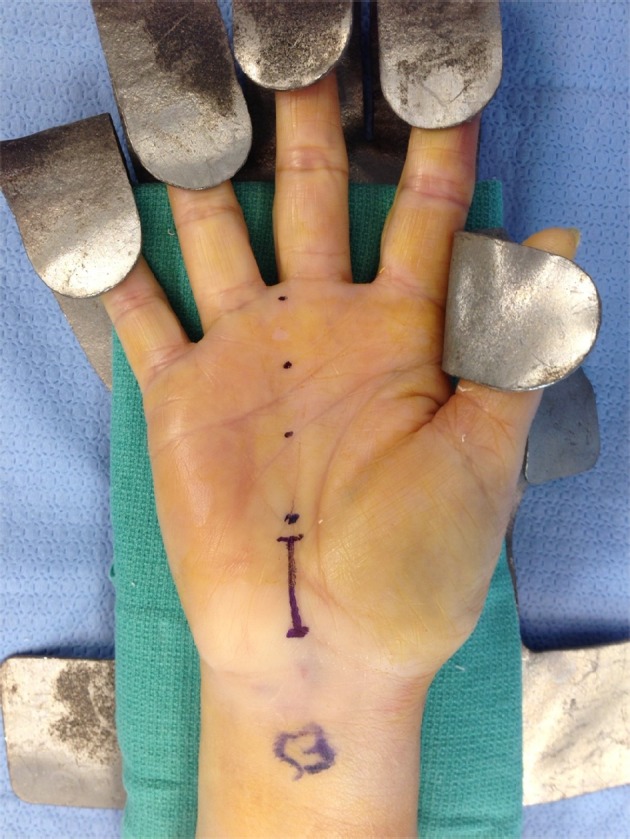
Surgical incision length of the mini-incision group
Fig. 2.

Surgical incision length of the extensile incision group
Statistical Analysis
To determine if data were normally distributed, data were analyzed using the Kolmogorov–Smirnoff test. For percentage grip strength change and BCTQ evaluation, nonparametric univariate analysis was performed with the Mann–Whitney U-test for comparison of two groups. Spearman’s rho correlation coefficient (r) was used for assessing associations between continuous variables. All statistical analyses were performed using IBM SPSS Statistics, Version 20 (Armonk, NY, USA). All reported p-values were two-tailed with an alpha of 0.05, indicating statistical significance.
Results
One hundred thirty-four cases met the study criteria and were included for analysis. There were 70 hands in 58 patients in group 1 (30 male and 40 female hands) and 64 hands in 56 patients in group 2 (29 male and 35 female hands). Complete patient demographics can be found in Table 1. All patients demonstrated a positive Phalen’s test, Tinel’s sign, and sensory changes in the distribution area of the median nerve. There was no significant difference between the two groups in regard to demographic data, comorbidities, or pre-operative electrodiagnostic testing results. All patients demonstrated non-recordable distal sensory latencies at pre-operative electrodiagnostic testing. Age was found to be significantly correlated with duration of follow-up (Spearman rho = 0.235; p = 0.014).
Table 1.
Patient demographics
| Mini-incision release | Extended release | |
|---|---|---|
| Severe CTS cases, (gender) | 70 (male, 30; female, 40) | 64 (male, 29; female, 35) |
| Number of patients, (gender) | 58 (male, 24; female, 34) | 56 (male, 26; female, 30) |
| Mean age at time of surgery, years (range) | 62 (34–89) | 65 (22–89) |
| Mean motor EMG onset (ms) | 7.54 | 7.91 |
| Cases with no response on motor EMG (percentage) | 8 (11.4) | 9 (14.1) |
| Patients with diabetes mellitus | 13 | 13 |
Forty-seven of the 70 (67 %) cases in group 1 had post-operative grip strengths available for comparison, compared to 62 of the 64 (97 %) cases in group 2. On average, patients in group 1 had a 22.6 % increase in grip strength at a postoperative follow-up of 4.5 ± 5.0 months, while patients in group 2 had a 59.3 % increase at an average of 10.0 ± 6.9 months, yielding no significant difference between the groups (p = 0.118) (Table 2). Duration of follow-up was found to be significantly correlated to percentage increase in grip strength (Spearman rho = 0.230; p = 0.016).
Table 2.
Patient outcomes
| Mini-incision release | Extended release | P-value | |
|---|---|---|---|
| Grip strength | |||
| Mean % increase | 22.6 | 59.3 | 0.118 |
| Mean follow-up (months) | 4.5 ± 5.04 | 10.0 ± 6.94 | |
| Boston Carpal Tunnel Questionnaire | |||
| Mean SSS (number of responses) | 12.93 (46) | 12.88 (42) | 0.926 |
| Mean FSS (number of responses) | 9.39 (46) | 9.10 (42) | 0.517 |
| Failures | 1 | 0 | |
SSS symptom severity scale, FSS functional status scale
Of the 114 patients (134 cases) who met the study criteria, five patients (five cases) refused to participate in follow-up and two patients (two cases) were deceased, leaving 107 patients (127 cases) available for follow-up. Fifteen patients (16 cases) were unable to be contacted by telephone or mail, and no follow-up information could be recorded as a result. Of the 127 cases, BCTQ forms were completed for 88 (69.3 %) at an average of 41.9 ± 10.6 months in group 1 patients and 43.1 ± 11.6 months in group 2 patients post-operatively (range, 12 to 61 months). There was no significant difference between the average follow-up. Patients in the mini-open cohort reported an average BCTQ symptom severity score of 12.93 (out of 55) and functional status score of 9.39 (out of 40) (n = 46). In the extended release cohort, average scores were 12.88 and 9.10, respectively (n = 42). There was no significant difference in BCTQ symptom severity or functional status scores between the two groups (p = 0.926 and p = 0.517, respectively) (Table 2).
Two patients in the mini-open cohort reported an atypical amount of pain following the procedure. In one patient, the pain was immediately following the procedure but resolved spontaneously with conservative treatment. The other patient reported increased scar sensitivity at 6 months post-operatively, which also resolved spontaneously. One patient in the mini-open cohort required revision surgery after 2 years and, for study purposes, was deemed a failure. An extensile release was performed at the revision surgery. The patient’s outcome data were still included in the analysis. No patient from the extended release cohort required secondary surgery.
Four patients in the extended release cohort developed erythema of the incision site within 6 weeks post-operatively, three of which were prescribed antibiotics as a precaution. One patient in the extended release cohort demonstrated mild wound dehiscence without erythema within the first 2 weeks post-operatively. This resolved on its own. Among the mini-open cohort, four patients demonstrated mild wound dehiscence within the first 2 post-operative weeks. Two of these patients were given antibiotics as a prophylaxis, and the other two were observed. All four patients’ dehiscence resolved without further incident by the next clinical visit.
Discussion
From a historical perspective, a standard procedure for carpal tunnel release had involved open release of the TCL through a longitudinal incision beginning at Kaplan’s cardinal line distally and extending proximally beyond the distal wrist crease. This lengthier incision may lead to longer healing time and, in some cases, increased scar tenderness [17, 22, 24]. Recently, limited incision and mini-open techniques for carpal tunnel release have been described [6, 14, 18, 30], and the question as to which offers an improved clinical result has prompted several comparative outcome studies [6, 14, 16]. Each of these aforementioned studies treated all CTS patients as a single population, however, and outcomes were not stratified according to pre-operative CTS severity.
The desire to achieve optimal clinical results while minimizing incision and exposure size continues to drive the advancement of new surgical techniques. Treatment for CTS has followed a similar pattern, with surgeons moving toward more conservative surgical approaches and shorter incision length [20, 33]. Surveys of ASSH members from 1987 and 2012 demonstrate this shift in surgical preferences, with the majority of surgeons now favoring a mini-open approach compared to a longer incision (>4 cm) [7, 20]. Similarly, a 2012 survey of AAHS members also found the mini-open technique to be the most common, utilized by 45.5 % of survey respondents compared to 33.3 % for an extensile approach. Interestingly, when that same population reported on surgical preference in electrodiagnostically severe CTS, the percentage of surgeons using the mini-open technique was equivalent to a more extensile approach (42.3 vs 43.9 %, respectively) [33]. This suggests that surgeons may actually choose a different and more extensile approach over a smaller incision when it comes to the treatment of severe CTS.
Treatment outcomes for severe CTS are not well documented in literature [8, 9, 27, 28, 31], and there are few, if any, comparative surgical technique studies pertaining specifically to this subset of patients. The results from the present study demonstrate that one technique does not result in any significant difference in post-operative patient-rated symptom severity or functional status in the long-term compared to the other. At an average follow-up of 40 months, no statistically significant difference was observed between the two cohorts regarding BCTQ scores on the symptom severity (p = 0.926) and functional status (p = 0.517) scales, and both techniques resulted in good functionality and minimal pain. These values are also equivalent to those reported in prior studies [11, 12], including most recently that of Beck et al. [3], in which patients demonstrated similarly acceptable outcomes, regardless of the pre-operative severity of the disease.
It is interesting to note the difference between the two groups regarding the post-operative grip strength percentage increase. Although large, this difference was not found to be statistically significant (p = 0.118). This may be a result of the difference between groups in follow-up duration, as well as the number of patients with recorded post-operative measurements. One must also bear in mind that follow-up duration was found to be positively correlated to percentage increase in grip strength (Spearman rho = 0.230; p = 0.016). This is not surprising as it is reasonable to expect that patients would demonstrate an increased improvement in grip strength as they progress further post-operatively. Therefore, the smaller percentage increase in grip strength of the mini-incision patients could result from shorter follow-up duration. It is also possible that this difference in follow-up duration may in fact mask a significant difference in outcomes between the two groups, however. Without similar follow-up durations for grip strength, it is not possible to determine with any certainty whether or not both groups would demonstrate an equivalent percentage increase. This exposes a weakness of the retrospective nature of the study as patients were not asked to return to the clinic and comparable follow-up measurements for grip strength could not be obtained.
Only one patient in both cohorts required revision surgery and was thus considered a failure. Originally in the mini-incision group, this patient underwent a secondary extensile release for recurrence of complaints. During the course of treatment, this patient was engaged in a lawsuit against his employer for his carpal tunnel symptoms. Post-operative NCS testing demonstrated marked improvement in both motor and sensory latencies following his index procedure despite his subjective complaints. A revision surgery with an extensile approach was utilized as a last effort to improve his carpal tunnel findings. However, even after his second surgery, he remained unsatisfied with his outcomes.
A strength of this study is that it presents a large cohort of severe CTS patients with unrecordable distal sensory latencies. However, there are a few notable weaknesses. The retrospective nature of the study limited the duration of clinical follow-up and data to only that recorded at each visit. Patients were unable to be randomized to each group as a result. Although no significant difference in demographic data or pre-operative electrodiagnostic testing existed, it is uncertain whether patients were adequately matched between the two groups with regard to symptom severity and functional status. Future prospective studies with pre-operative BCTQ data would be helpful both in randomizing patients and quantifying the post-operative change in symptom severity and functional status. This leads to another limitation to the reported BCTQ results. Despite not identifying any statistically significant difference between the two groups for symptom severeity or functional status, this is not the same as saying that both groups’ outcomes are truly equivalent. Having pre-operative BCTQ data would therefore help to alleviate this issue, providing an initial data point to compare outcomes for each group. It was also decided to not focus on short-term differences between the two operative techniques, and thus no comment can be made as to whether the mini-open technique had advantages regarding recovery time, scar sensitivity, or cosmetic satisfaction.
The present study suggests that mini-open and extended open carpal tunnel release offer similar outcomes and that both are safe and effective treatment options for severe CTS. Patients with diagnosis of severe CTS represent a unique subset within the disease population, and further studies addressing treatment choice and surgical outcomes of this group specifically are required.
Acknowledgements
The authors wish to acknowledge Abdo Bachoura, M.D., for assistance in data collection and interpretation, as well as Grant Dornan, M.Sc., for his contribution of statistical expertise to the analysis in this study.
No external funding was required for this study.
Conflict of Interest
Praveen G. Murthy declares that he has no conflict of interest.
Peter Goljan declares that he has no conflict of interest.
Gregory Mendez declares that he has no conflict of interest.
Sidney M. Jacoby declares that he has no conflict of interest.
Eon K. Shin declares that he has no conflict of interest.
A. Lee Osterman declares that he has no conflict of interest.
Statement of Human and Animal Rights
All study procedures were followed in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 and 2008.
Statement of Informed Consent
Informed consent was obtained from all patients included within the study.
References
- 1.Al-Benna S, Nano PG, El-Enin H. Extended open-carpal tunnel release in renal dialysis patients. Saudi J Kidney Dis Transpl. 2012;23(6):1181–1187. doi: 10.4103/1319-2442.103557. [DOI] [PubMed] [Google Scholar]
- 2.Atroshi I, Larsson GU, Ornstein E, Hofer M, Johnsson R, Ranstam J. Outcomes of endoscopic surgery compared with open surgery for carpal tunnel syndrome among employed patients: randomised controlled trial. BMJ. 2006;332(7556):1473. doi: 10.1136/bmj.38863.632789.1F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beck JD, Wingert NC, Rutter MR, Irgit KS, Tang X, Klena JC. Clinical outcomes of endoscopic carpal tunnel release in patients 65 and over. J Hand Surg [Am] 2013;38(8):1524–1529. doi: 10.1016/j.jhsa.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 4.Blair WF, Goetz DD, Ross MA, Steyers CM, Chang P. Carpal tunnel release with and without epineurotomy: a comparative prospective trial. J Hand Surg [Am] 1996;21(4):655–661. doi: 10.1016/S0363-5023(96)80021-9. [DOI] [PubMed] [Google Scholar]
- 5.Bland JD. A neurophysiological grading scale for carpal tunnel syndrome. Muscle Nerve. 2000;23(8):1280–1283. doi: 10.1002/1097-4598(200008)23:8<1280::AID-MUS20>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 6.Cellocco P, Rossi C, Bizzarri F, Patrizio L, Costanzo G. Mini-open blind procedure versus limited open technique for carpal tunnel release: a 30-month follow-up study. J Hand Surg [Am] 2005;30(3):493–499. doi: 10.1016/j.jhsa.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 7.Duncan KH, Lewis RC, Jr, Foreman KA, Nordyke MD. Treatment of carpal tunnel syndrome by members of the American Society for Surgery of the Hand: results of a questionnaire. J Hand Surg [Am] 1987;12(3):384–391. doi: 10.1016/S0363-5023(87)80011-4. [DOI] [PubMed] [Google Scholar]
- 8.Finestone HM, Woodbury GM, Collavini T, Marchuk Y, Maryniak O. Severe carpal tunnel syndrome: clinical and electrodiagnostic outcome of surgical and conservative management. Muscle Nerve. 1996;19(2):237–239. doi: 10.1002/(SICI)1097-4598(199602)19:2<237::AID-MUS20>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 9.Gelberman RH, Pfeffer GB, Galbraith RT, Szabo RM, Rydevik B, Dimick M. Results of treatment of severe carpal-tunnel syndrome without internal neurolysis of the median nerve. J Bone Joint Surg Am. 1987;69(6):896–903. [PubMed] [Google Scholar]
- 10.Gerritsen AA, Uitdehaag BM, van Geldere D, Scholten RJ, de Vet HC, Bouter LM. Systematic review of randomized clinical trials of surgical treatment for carpal tunnel syndrome. Br J Surg. 2001;88(10):1285–1295. doi: 10.1046/j.0007-1323.2001.01858.x. [DOI] [PubMed] [Google Scholar]
- 11.Greenslade JR, Mehta RL, Belward P, Warwick DJ. Dash and Boston questionnaire assessment of carpal tunnel syndrome outcome: what is the responsiveness of an outcome questionnaire? J Hand Surg (Br) 2004;29(2):159–164. doi: 10.1016/j.jhsb.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 12.Heybeli N, Kutluhan S, Demirci S, Kerman M, Mumu EF. Assessment of outcome of carpal tunnel syndrome: a comparison of electrophysiological findings and a self-administered Boston questionnaire. J Hand Surg (Br) 2002;27(3):259–264. doi: 10.1054/jhsb.2002.0762. [DOI] [PubMed] [Google Scholar]
- 13.Holmgren H, Rabow L. Internal neurolysis or ligament division only in carpal tunnel syndrome. II. A 3 year follow-up with an evaluation of various neurophysiological parameters for diagnosis. Acta Neurochir (Wien) 1987;87(1–2):44–47. doi: 10.1007/BF02076014. [DOI] [PubMed] [Google Scholar]
- 14.Huang JH, Zager EL. Mini-open carpal tunnel decompression. Neurosurgery. 2004;54(2):397–399. doi: 10.1227/01.NEU.0000103669.45726.51. [DOI] [PubMed] [Google Scholar]
- 15.Huisstede BM, Randsdorp MS, Coert JH, Glerum S, van Middelkoop M, Koes BW. Carpal tunnel syndrome. Part II: effectiveness of surgical treatments—a systematic review. Arch Phys Med Rehabil. 2010;91(7):1005–1024. doi: 10.1016/j.apmr.2010.03.023. [DOI] [PubMed] [Google Scholar]
- 16.Jugovac I, Burgić N, Mićović V, Radolović-Prenc L, Uravić M, Golubović V, et al. Carpal tunnel release by limited palmar incision vs traditional open technique: randomized controlled trial. Croat Med J. 2002;43(1):33–36. [PubMed] [Google Scholar]
- 17.Kessler FB. Complications of the management of carpal tunnel syndrome. Hand Clin. 1986;2(2):401–406. [PubMed] [Google Scholar]
- 18.Lee WP, Strickland JW. Safe carpal tunnel release via a limited palmar incision. Plast Reconstr Surg. 1998;101(2):418–424. doi: 10.1097/00006534-199802000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Leinberry CF, Hammond NL, Siegfried JW. The role of epineurotomy in the operative treatment of carpal tunnel syndrome. J Bone Joint Surg Am. 1997;79(4):555–557. doi: 10.2106/00004623-199704000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Leinberry CF, Rivlin M, Maltenfort M, Beredjiklian P, Matzon JL, Ilyas AM, et al. Treatment of carpal tunnel syndrome by members of the American Society for Surgery of the Hand: a 25-year perspective. J Hand Surg [Am] 2012;37(10):1997–2003. doi: 10.1016/j.jhsa.2012.07.016. [DOI] [PubMed] [Google Scholar]
- 21.Levine DW, Simmons BP, Koris MJ, Daltroy LH, Hohl GG, Fossel AH, et al. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993;75(11):1585–1892. doi: 10.2106/00004623-199311000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Louis DS, Greene TL, Noellert RC. Complications of carpal tunnel surgery. J Neurosurg. 1985;62(3):352–356. doi: 10.3171/jns.1985.62.3.0352. [DOI] [PubMed] [Google Scholar]
- 23.Lowry WE, Jr, Follender AB. Interfascicular neurolysis in the severe carpal tunnel syndrome. A prospective, randomized, double-blind, controlled study. Clin Orthop Relat Res. 1988;227:251–254. [PubMed] [Google Scholar]
- 24.MacDonald RI, Lichtman DM, Hanlon JJ, Wilson JN. Complications of surgical release for carpal tunnel syndrome. J Hand Surg. 1978;3(1):70–76. doi: 10.1016/S0363-5023(78)80118-X. [DOI] [PubMed] [Google Scholar]
- 25.Means KR, Jr, Parks BG, Lee SK, Segalman KA. Release of the transverse carpal ligament alone is associated with elevated pressure beneath the distal volar forearm fascia in a cadaver model of carpal tunnel syndrome. J Hand Surg [Am] 2007;32(10):1533–1537. doi: 10.1016/j.jhsa.2007.08.020. [DOI] [PubMed] [Google Scholar]
- 26.Mintalucci DJ, Leinberry CF., Jr Open versus endoscopic carpal tunnel release. Orthop Clin N Am. 2012;43(4):431–437. doi: 10.1016/j.ocl.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 27.Mondelli M, Reale F, Padua R, Aprile I, Padua L. Clinical and neurophysiological outcome of surgery in extreme carpal tunnel syndrome. Clin Neurophysiol. 2001;112(7):1237–1242. doi: 10.1016/S1388-2457(01)00555-7. [DOI] [PubMed] [Google Scholar]
- 28.Nolan WB, 3rd, Alkaitis D, Glickel SZ, Snow S. Results of treatment of severe carpal tunnel syndrome. J Hand Surg [Am] 1992;17(6):1020–1023. doi: 10.1016/S0363-5023(09)91050-4. [DOI] [PubMed] [Google Scholar]
- 29.Phalen GS. The carpal-tunnel syndrome. Seventeen years’ experience in diagnosis and treatment of six hundred fifty-four hands. J Bone Joint Surg Am. 1966;48(2):211–228. [PubMed] [Google Scholar]
- 30.Plancher KD, Perekh SR. Limited open incision carpal tunnel release. Tech Hand Upper Extrem Surg. 1998;2(1):64–71. doi: 10.1097/00130911-199803000-00009. [DOI] [PubMed] [Google Scholar]
- 31.Rhoades CE, Mowery CA, Gelberman RH. Results of internal neurolysis of the median nerve for severe carpal-tunnel syndrome. J Bone Joint Surg Am. 1985;67(2):253–256. [PubMed] [Google Scholar]
- 32.Scholten RJ. Mink van der Molen AM. Bouter LM, de Vet HC. Surgical treatment options for carpal tunnel syndrome. Cochrane Database Syst Rev: Uitdehaag BM; 2009. [DOI] [PubMed] [Google Scholar]
- 33.Shin EK, Bachoura A, Jacoby SM, Chen NC, Osterman AL. Treatment of carpal tunnel syndrome by members of the American Association for Hand Surgery. Hand. 2012;7(4):351–356. doi: 10.1007/s11552-012-9455-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shum C, Parisien M, Strauch RJ, Rosenwasser MP. The role of flexor tenosynovectomy in the operative treatment of carpal tunnel syndrome. J Bone Joint Surg Am. 2002;84(2):221–225. doi: 10.2106/00004623-200202000-00009. [DOI] [PubMed] [Google Scholar]
- 35.Wilson SW, Pollard RE, Lees VC. Management of carpal tunnel syndrome in renal dialysis patients using an extended carpal tunnel release procedure. J Plast Reconstr Aesthet Surg. 2008;61(9):1090–1094. doi: 10.1016/j.bjps.2007.07.004. [DOI] [PubMed] [Google Scholar]


