Abstract
The diastolic intraventricular ring vortex formation and pinch-off process may provide clinically useful insights into diastolic function in health and disease. The vortex ring formation time (FT) concept, based on hydrodynamic experiments dealing with unconfined (large tank) flow, has attracted considerable attention and popularity. Dynamic conditions evolving within the very confined space of a filling, expansible ventricular chamber with relaxing and rebounding viscoelastic muscular boundaries, diverge from unconfined (large tank) flow and encompass rebounding walls’ suction and myocardial relaxation. Indeed, clinical/physiological findings seeking validation in vivo failed to support the notion that FT is an index of normal/abnormal diastolic ventricular function. Therefore, FT as originally proposed cannot and should not be utilized as such an index. Evidently, physiologically accurate models accounting for coupled hydrodynamic and (patho)physiological myocardial wall interactions with the intraventricular flow are still needed to enhance our understanding and yield diastolic function indices useful and reliable in the clinical setting.
Keywords: Vortex formation time (FT), Ventricular function, Diastole, Atrioventricular and intraventricular pressure difference, Intraventricular diastolic flow, Diastolic vortex interaction with myocardial boundaries
But experience is by far the best demonstration, provided it adhere to the experiment actually made, for if that experiment be transferred to other subjects apparently similar, unless with proper and methodical caution it becomes fallacious.
—Sir Francis Bacon, Aphorism LXX. Novum Organum, Book I (1620)
Clinical Perspective
Diastolic dysfunction spans an array of clinical conditions in a setting where the cardiac ventricle(s) are unable to fully relax while they fill in diastole or they fill incompletely in the time available for filling at a suitably low pressure to prevent upstream congestion. Traditional global ratios such as early to late diastolic transmitral blood flow velocity (E/A), early transmitral inflow velocity to early mitral annular velocity (E/e′), early transmitral blood flow velocity to color Doppler M-mode flow propagation velocity (E/Vp), etc. or metrics like regional myocardial strains and strain rates are often used for the clinical evaluation of diastolic cardiac function. Yet, such measures do not adequately enlighten clinical decisions, and therefore, numerous recent pluridisciplinary studies have been devoted toward developing novel and better indices of right ventricular/left ventricular (RV/LV) diastolic performance.
However, such studies oftentimes do not capture the intricacies of the interplay between physiologic conditions, functional characteristics, and the fluid dynamics that govern the diastolic filling process in hearts working under various normal and abnormal operating circumstances. They then can lead to systematic prediction errors, misleading results, and incorrect deductions, as cautioned by Sir Francis Bacon, in the epigraph. The “universal parameter or diastolic intraventricular vortex ring formation time” is such a noninvasive index of diastolic function that has been recently proposed. It is based upon extrapolating vortex formation findings from simplified in vitro experiments, and it has been currently receiving considerable attention in the literature. This timely survey and commentary aims to enable the practicing cardiologist to acquire a better intuitive and conceptual grasp of diastolic intraventricular vortex ring formation, its potential clinical utility, and also the limitations and pitfalls of accepting and using a universal vortex formation time as an index of diastolic function without previous proper validation in the heart working in situ.
Introduction
Ventricular filling is complex and remains far less understood than ejection [1, 2]. Early in diastole, there is rapid blood flow into each ventricle through its atrioventricular valve, in response to an atrioventricular and intraventricular pressure difference (IVPD). This rapid inflow results in the formation of a ring-shaped vortex that interacts with the surrounding myocardial walls. This toroidal vortex is developed as the blood recirculates back upon itself, forming a spinning coil. Leonardo da Vinci first described vortex motions in the sinuses of Valsalva in his Quaderni d′ Anatomia in 1513 [3]. Later, vortex rings intrigued the physician-physiologist Hermann Helmholtz, who was one of the founders of vortex dynamics [1]. The duration of the early filling and the magnitude of the IVPD govern the formation of the diastolic vortex; hence, impaired diastolic function and dynamics would alter its formation time and strength. In recent years, fluid mechanics concepts primarily based on observations of vortex ring formation in large, unbounded flow domains (large liquid-filled tanks) have been extrapolated to intraventricular filling vortex formation and diastolic ventricular function. Here, we examine this approach, namely of inductively generalizing the concept/“universal parameter” of a vortex ring formation time from physical observations of unconstrained, unbounded vortical flows to intracardiac blood flows, where the forming vortices are enclosed within confining tapering myocardial RV/LV boundaries.
The Proposed “Universal Parameter” of a Vortex Ring Formation Time (FT)
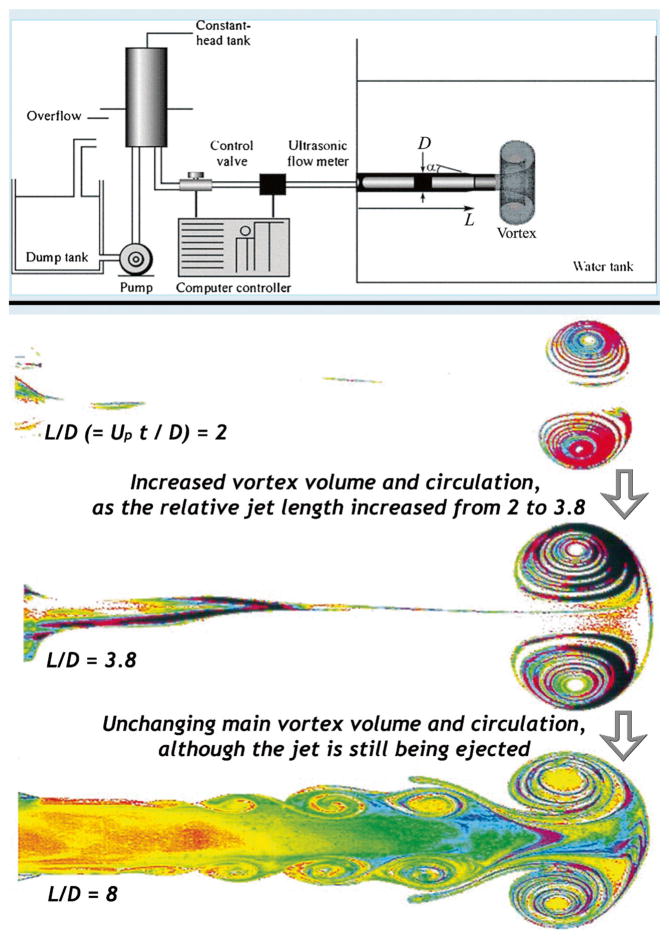
Gharib and his collaborators, in a series of influential contributions, investigated the fundamentals of canonical (archetypal) unconfined vortex rings [4, 5]. Using a piston-driven vortex ring generator, liquid was pushed into a large-volume tank through a long cylindrical conduit of inner diameter D (Fig. 1, top). A wide range of piston stroke-length to diameter (L/D) ratios was used to form vortex rings of varied strengths into the large tank. The jet velocity (V0) and discharge interval duration (T) were specified, and a slug flow model with radially uniform (flat) velocity profile was assumed. The overall length of the cylinder limited the maximum stroke of the piston to (L/D)max=15, and the maximum acceleration and deceleration to |a|max≈250 cm s−2. This procedure is inherently governed by the temporal evolution of the velocity and acceleration of the piston and the fluid, and therefore, the conditions of the vortex ring formation can appear to depend upon the characteristics of the motion of the piston; e.g., at the time of a sudden piston stop, the liquid jet moving at any sizeable velocity may continue its inertial motion, rendering the actual discharge duration longer than the piston stroke.
Fig. 1.
Top: schematic representation of the vortex ring generator tank utilized by Gharib et al. Bottom: visualization images of vortex ring formation in the tank of the top panel, obtained by Gharib et al. for assorted durations of jet discharge, Upt/D. See discussion in text. (From Gharib et al. [5], reproduced by permission of Cambridge University Press)
Applying fluid dynamic dimensional analysis [1], impulsive formation of a vortex ring by such a jet exhausting from a circular nozzle into a large unconstrained volume (Fig. 1, top) is shown to be determined by the dimensionless length of the ejected jet, L*=V0T/D, and its Reynolds number Re=V0D/ν, where ν is the kinematic viscosity of the liquid. The “strength of the vortex ring” is measured by the hydrodynamic circulation of the vortex, which can be defined simply as the product of the Reynolds number with the kinematic viscosity [6].
As is shown in Fig. 1, bottom, Gharib et al. [5] reported that the volume and the circulation of a vortex ring increase with the jet length L* only until L*≤8–10, which corresponds to the dimensionless discharge time Upt/D≈4–5, where Up is the running mean (time integrated) of the piston velocity, assumed to equal that of the jet issuing out of the conduit, D is the conduit’s inner diameter, and t is discharge time. Then, a critical point is reached, i.e., the volume and the circulation of the vortex ring that forms in the head portion of the jet do not increase further, they stay approximately constant, despite continuing jet discharge [5]. Effectively, it is no longer possible for the discharged jet’s mass and energy to further strengthen the vortex ring, and the vortex ring is then pinched-off, i.e., it detaches from the momentum supplying inflowing jet, and the excess mass and energy are disposed of into a system of a few secondary vortices in its wake (Fig. 1, bottom) [5]. These investigators proposed that the nominal pinch-off instant corresponds to a nondimensional “universal vortex ring formation time,” FT=Upt/D≈4–5, denoting the dimensionless time at which both the volume and the circulation of the vortex ring reach a limiting magnitude. According to this model, pinch-off occurs when the inflow jet is terminated or when the expanding vortex ring reaches its energetic limit—the above described critical point [5].
Physiological Concerns on the Universality of the Proposed Parameter
The introduction of the formation time (FT) and its ramifications [4, 5] had a transformative impact on the fluid mechanics understanding of vortex formation processes in aerodynamics and other conventional branches of fluid dynamics [7]. However, before generalizing this concept to intraventricular flows, one needs to consider how the formation process is affected by the presence of confining boundaries. Although vortex ring pinch-off always occurs when the critical conditions are reached, the formation process and the potential FT values are dependent on the orifice geometry, the surrounding boundaries’ geometry, and the applying flow conditions. All these parameters are not “universal”; as a matter of fact, they are very application specific. In particular, considering the diastolic intraventricular vortex formation process in the heart, the physiologic and pathologic conditions are highly diverse and very different [7] from the conditions (cf. Fig. 1) under which the universal FT was introduced [4, 5]. In the case of the RV/LV bounded flow domains with confining endocardial sidewalls, the vortices interact with the solid boundaries, providing a net torque on the no-slip walls and impacting the angular momentum of the flow [7, 8]. Additionally, vortex formation is governed by the vorticity production and flux into the vortex. In the case of the RV/LV flow, the vorticity production will be controlled by the temporal evolution of the intraventricular pressure difference, which cannot be reproduced with a simple model of vortex ring formation in an unbounded domain.
Despite these shortcomings, the above experimental vortex formation concept, characterized using a virtually unbounded domain (large-volume tank, Fig. 1), encouraged numerous additional investigations to apply the “FT” as an index of filling dynamics in the heart, beating in situ [9–13]. It was conjectured, but not tested, that the FT is an index of diastolic ventricular function both normally and in presence of diverse filling abnormalities, not properly accounting for the dependence of vortex ring formation characteristics on the applying conditions. The published results [9–13] alluded that normal subjects exhibit FTs close to 4–5; mitral valve stenosis begets a substantial increase in the FT, whereas patients with impaired relaxation, a pseudonormal transmitral flow pattern, restrictive ventricular filling, and dilated cardiomyopathy would exhibit FT values considerably lower than normal.
Vortex Formation Time Measurements on Normal Subjects and Patients
In addition, the proposed calculation of a universal parameter or FT heart index [5] was based on the assumption that the FT coincided with the completion of the early filling E-wave. But this latter key assumption was not tested or verified [9]. Subsequent work by Stewart et al. [14] evaluated this hypothesis directly on normal subjects and patients, using LV color M-mode echocardiography and phase-contrast MRI velocimetry. It was found that the diastolic LV vortex ring formation process and pinch-off are governed by the temporal evolution of the favorable atrioventricular pressure difference (whose cumulative magnitude increases with distance along the inflow axis), which is driving early diastolic inflow. In fact, the vortex ring pinch-off within the ventricle occurs when this inflow-driving pressure difference declines to zero—an event correlated with the onset of the early filling wave deceleration—and not with the completion of the E-wave. Accordingly, the vortex ring formation time should be measured from the initiation of the E-wave only up to the “velocity deceleration point,” located at the intersection of the initial and terminal propagation velocities of the early diastolic inflow. This was recently demonstrated and validated—using color M-mode echocardiography—by Stewart et al. [15]; they also cited earlier works showing that the vortex pinch-off indeed coincides with the deceleration of the filling propagation velocity, which clearly occurs considerably before the completion of the E-wave.
Stewart et al. [14] found that the pressure difference from the left atrium to the LV apex that drives early filling falls to zero simultaneously with the deceleration of the early filling wave and the pinch-off of the diastolic vortex ring. What is more, in concert with the earlier findings of Gharib and coworkers [9], when FT—the proposed index of optimal filling vortex formation—was calculated using the total duration of early filling (i.e., up to the end of the E-wave), FT was not constant but varied both with age and with ventricular diastolic dysfunction (Fig. 2). However, such evaluations are not consistent with the actual physical process where the vortex ring pinches-off before the completion of the E-wave, at the time that the abrupt filling wave deceleration is observed.
Fig. 2.
The vortex formation time calculated as Gharib et al.’s FT index [4, 5], using the total E-wave duration (green circles), and as determined [14] using the time interval from the initiation of the E-wave until the time of the actual vortex ring pinch-off (blue diamonds). The vortex formation times are displayed versus A age in years for 46 healthy subjects, as classified by E/E′<8 and B early diastolic peak intraventricular pressure difference (IVPD, mmHg) for 128 patients with varying degrees of diastolic dysfunction. The center lines display the linear fits and the shaded regions, the 95 % confidence intervals. See discussion in text. (From Stewart et al. [14] reproduced by permission of The American Physiological Society)
Most importantly, Stewart et al. [14] then proceeded to show that when FT is computed up to the time of the actual pinch-off, then it remains, in fact, unaffected by either age or impairments of diastolic ventricular function (Fig. 2). These pivotal results [14], shown in the plots of Fig. 2, imply that the diastolic vortex formation is regulated by the temporal evolution of the intraventricular pressure difference during early filling [16] and that FT is not, in fact, an index of diastolic dysfunction as previously thought [9]. This does not imply that the vortex ring strength is also independent of diastolic ventricular function. Since the early vortex ring strength is governed by the more or less energetic ventricular suction, increased early intraventricular pressure gradients and inflow velocities yield higher vortex ring strength and vice versa, as it was shown for the right ventricle by Pasipoularides et al. [17, 18] and for the left ventricle by Charonko et al. [19].
Conclusions
In conclusion, the diastolic ring vortex formation may provide useful insights into ventricular filling. Understanding the physical principles that govern vortex formation and pinch-off can enhance our understanding of normal and pathologic processes. The vortex ring FT concept, based on a simplistic model of unconfined (large-tank) flow, has attracted considerable attention and popularity. However, clinical/physiological findings [14] do not support the notion that the FT is an index of normal/abnormal ventricular filling function. Dynamic conditions of ventricular filling diverge from those of unconfined (large-tank) flow and are driven not only by passive processes but also by rebounding walls’ suction and myocardial relaxation [20–22]. These processes evolve within the very confined space of a filling, expansible ventricular chamber with relaxing and rebounding, viscoelastic muscular boundaries [1, 7]. Thus, FTas originally proposed cannot be used as an index of ventricular diastolic function. Nonetheless, physiologically accurate models accounting for hydrodynamic and (patho)physiological myocardial wall interactions with the intraventricular flow are still needed in order to enhance our understanding and yield diastolic function indices useful and reliable in the clinical setting.
Acknowledgments
Funding Work from A.P.’s Laboratory surveyed here was supported, in part, by the National Heart, Lung, and Blood Institute [grant number R01-HL-050446]; the National Science Foundation [grant number CDR 8622201]; and the North Carolina Supercomputing Center/Cray Research. Work from P.P.V.’s Laboratory surveyed here was supported, in part, by the National Heart, Lung, and Blood Institute [grant number R21-HL-106276-01A1].
Contributor Information
Ares Pasipoularides, Email: apasipou@duke.edu, Duke University School of Medicine, Durham, NC, USA. Duke/NSF Research Center for Emerging Cardiovascular Technologies, Duke University, Durham, NC 27710, USA.
Pavlos P. Vlachos, Biomedical Engineering, Purdue University, West Lafayette, IN 47907, USA. Mechanical Engineering Department, Virginia Tech University, Blacksburg, VA, USA. School of Biomedical Engineering and Sciences, Virginia Tech, Blacksburg, VA, USA. Engineering Science and Mechanics Department, Virginia Tech, Blacksburg, VA, USA. Wake Forest University School of Medicine, Winston-Salem, NC, USA
William C. Little, Lehan Professor and Chair, Department of Medicine, University of Mississippi Medical Center, Jackson, MS 39216, USA
References
- 1.Pasipoularides A. Heart’s vortex: intracardiac blood flow phenomena. Shelton: People’s Medical Publishing House; 2010. p. 960. [Google Scholar]
- 2.Pasipoularides A. Clinical assessment of ventricular ejection dynamics with and without outflow obstruction. [Review] Journal of the American College of Cardiology. 1990;15:859–882. doi: 10.1016/0735-1097(90)90287-y. [DOI] [PubMed] [Google Scholar]
- 3.Pasipoularides A. Historical continuity in the methodology of modern medical science: Leonardo leads the way. International Journal of Cardiology. 2014;171:103–115. doi: 10.1016/j.ijcard.2013.11.133. [DOI] [PubMed] [Google Scholar]
- 4.Weigand A, Gharib M. On the evolution of laminar vortex rings. Experiments in Fluids. 1997;22:447–457. [Google Scholar]
- 5.Gharib M, Rambod E, Shariff K. A universal time scale for vortex ring formation. Journal of Fluid Mechanics. 1998;360:121–140. [Google Scholar]
- 6.Pasipoularides A. Evaluation of right and left ventricular diastolic filling. Journal of Cardiovascular Translational Research. 2013;6:623–639. doi: 10.1007/s12265-013-9461-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pasipoularides A. Analysis of vortex flow imaging in normal and dysfunctional RV’s. American Society of Echocardiography 22nd Annual Scientific Sessions, Montreal, 2011 EE02d – Flow Vortex Imaging. 2011 PROLibraries.com http://www.aseuniversity.org/session/3053/Flow-Vortex-Imaging-br-Analysis-of-Vortex-Flow-Imaging-in-Normal-and-Dysfunctional-RV-s.
- 8.Pasipoularides A. Diastolic filling vortex forces and cardiac adaptations: probing the epigenetic nexus. Hellenic Journal of Cardiology. 2012;53:458–469. [PMC free article] [PubMed] [Google Scholar]
- 9.Gharib M, Rambod E, Kheradvar A, Sahn DJ, Dabiri JO. Optimal vortex formation as an index of cardiac health. Proceedings of the National Academy of Sciences of the United States of America. 2006;103:6305–6308. doi: 10.1073/pnas.0600520103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ishizu T, Seo Y, Ishimitsu T, Obara K, Moriyama N, Kawano S, et al. The wake of a large vortex is associated with intraventricular filling delay in impaired left ventricles with a pseudonormalized transmitral flow pattern. Echocardiography. 2006;23:369–375. doi: 10.1111/j.1540-8175.2006.00220.x. [DOI] [PubMed] [Google Scholar]
- 11.Jiamsripong P, Calleja AM, Alharthi MS, Dzsinich M, McMahon EM, Heys JJ, et al. Impact of acute moderate elevation in left ventricular afterload on diastolic transmitral flow efficiency: analysis by vortex formation time. Journal of the American Society of Echocardiography. 2009;22:427–431. doi: 10.1016/j.echo.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kheradvar A, Assadi R, Falahatpisheh A, Sengupta PP. Assessment of transmitral vortex formation in patients with diastolic dysfunction. Journal of the American Society of Echocardiography. 2011;25:220–227. doi: 10.1016/j.echo.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 13.Poh KK, Lee LC, Shen L, Chong E, Tan YL, Chai P, et al. Left ventricular fluid dynamics in heart failure: echocardiographic measurement and utilities of vortex formation time. European Journal of Echocardiography. 2012;13:385–393. doi: 10.1093/ejechocard/jer288. [DOI] [PubMed] [Google Scholar]
- 14.Stewart KC, Charonko JC, Niebel CL, Little WC, Vlachos PP. Left ventricle filling vortex formation is unaffected by diastolic impairment. American Journal of Physiology Heart and Circulatory Physiology. 2012;303:H1255–H1262. doi: 10.1152/ajpheart.00093.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stewart KC, Kumar R, Charonko JJ, Ohara T, Vlachos PP, Little WC. Evaluation of LV diastolic function from color M-mode echocardiography. JACC Cardiovascular Imaging. 2011;4:37–46. doi: 10.1016/j.jcmg.2010.09.020. [DOI] [PubMed] [Google Scholar]
- 16.Pasipoularides A. Right and left ventricular diastolic flow field: why are measured intraventricular pressure gradients small? Revista Española de Cardiología. 2013;66:337–341. doi: 10.1016/j.rec.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pasipoularides A, Shu M, Shah A, Womack MS, Glower DD. Diastolic right ventricular filling vortex in normal and volume overload states. American Journal of Physiology Heart and Circulatory Physiology. 2003;284:H1064–H1072. doi: 10.1152/ajpheart.00804.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pasipoularides A, Shu M, Shah A, Tucconi A, Glower DD. RV instantaneous intraventricular diastolic pressure and velocity distributions in normal and volume overload awake dog disease models. American Journal of Physiology Heart and Circulatory Physiology. 2003;285:H1956–H1965. doi: 10.1152/ajpheart.00372.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Charonko JJ, Kumar R, Stewart K, Little WC, Vlachos PP. Vortices formed on the mitral valve tips aid normal left ventricular filling. Annals of Biomedical Engineering. 2013;41:1049–1061. doi: 10.1007/s10439-013-0755-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pasipoularides A. Right and left ventricular diastolic pressure–volume relations: a comprehensive review. Journal of Cardiovascular Translational Research. 2013;6:239–252. doi: 10.1007/s12265-012-9424-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pasipoularides A. LV twisting-and-untwisting in HCM: ejection begets filling. Diastolic functional aspects of HCM. American Heart Journal. 2011;162:798–810. doi: 10.1016/j.ahj.2011.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pasipoularides A, Mirsky I, Hess OM, Grimm J, Krayenbuehl HP. Myocardial relaxation and passive diastolic properties in man. Circulation. 1986;74:991–1001. doi: 10.1161/01.cir.74.5.991. [DOI] [PubMed] [Google Scholar]