Introduction
Adenoid cystic carcinoma (ACC) is a rare cancer of the salivary gland arising from myoepithelial cells, accounting for 10 % of salivary carcinoma and <1 % of head and neck tumors [1]. The natural history of ACC can be varied. A subset of patients with ACC can have an aggressive clinical course often characterized by a high incidence of local recurrence. Up to 40 % of submandibular gland ACC tumors can metastasize distally, with the lung, bone, brain, and liver being the most common sites [2, 3]. Very few cases have been reported with liver metastasis as the initial presentation of ACC [4, 5].
Case Report
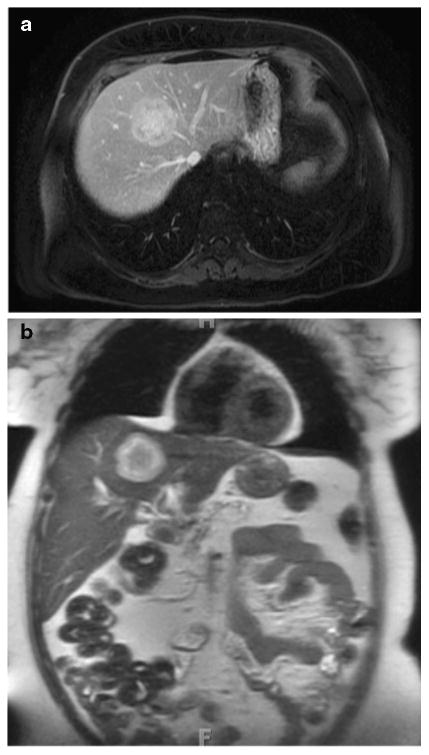
A 59-year-old Caucasian female presented with complaints of mild, vague abdominal pain. The outside institution obtained an abdominal magnetic resonance image (MRI) that revealed a 4.5 cm mass in the liver abutting the common trunk of the middle and left hepatic veins (Fig. 1). Upon referral to Johns Hopkins Hospital, the films were reviewed and the mass was deemed to be suspicious for a malignancy such as an intrahepatic cholangiocarcinoma. Further work-up including endoscopy and recent mammogram was unremarkable. The patient underwent an uneventful extended left hepatectomy with concomitant lymphadenectomy.
Fig. 1. Axial (a) and coronal view (b) of the liver mass.
Gross pathology revealed a tan-white, lobulated mass measuring 5 cm. On histological evaluation, the lesion was well-circumscribed and had a solid architecture, with some areas characterized by a cribriform pattern comprised of pseudolumens (Fig. 2a). While the overall pattern was consistent with a possible ACC, there was no history of a primary tumor. The specimen stained positive for cytokeratin 7, c-KIT, and EMA and negative for PAX8, TTF-1, CDX2, cytokeratin 20, chromagranin, synaptophysin, CD5, Hepar1, ER, and p63. Ki67 staining was 20–30 % positive. Based on histology and immunostaining, a diagnosis of high-grade carcinoma, best classified as a solid variant of ACC, was suspected. Further studies with cytogenetic fluorescent immunohistochemistry staining (FISH) for the translocation t(6;9)(q22–23; p23–24) confirmed the diagnosis of ACC [6].
Fig. 2.
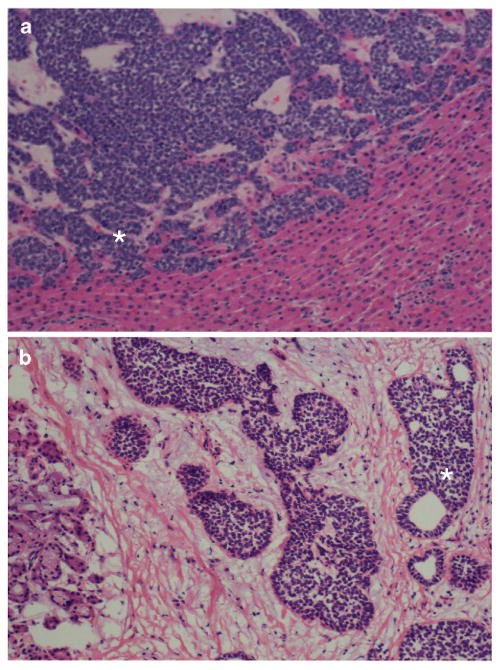
Adenoid Cystic Carcinoma metastasis (asterisk) abutting uninvolved hepatic tissue. Hyaline material was noted within the pseudolumens of the cribriform architecture (a); Adenoid Cystic Carcinoma primary tumor (asterisk) next to salivary gland ducts (b)
On directed questioning, the patient revealed that indeed she had experienced a vague feeling of fullness in her right submandibular region and had been diagnosed with a “salivary stone” 2 years ago. The patient was referred for ENT consultation; head and neck MRI revealed a mass in the right submandibular gland as well as suspicious level II and III nodes (Fig. 2b). A right submandibular gland excision with neck dissection was performed. Final pathology revealed a 3-cm primary ACC with a solid high-grade component (pathologic stage: pT3N2bM1). PET scan revealed no evidence of other systemic disease. The patient received adjuvant systemic therapy with cisplatin combined with radiation therapy and is currently disease-free at 5 months of follow-up.
Discussion
ACC of the salivary glands is an uncommon tumor, characterized by local invasion and nodal metastasis, as well as hematogenous distant spread [3–7]. While distant metastasis may only become clinically manifest after a long period of time, evidence of micro-metastasis at the cellular level can often be detected earlier [7]. However, distant metastases typically occur after the diagnosis and treatment of the primary tumor, even many years afterward [2, 8–10]. The current case is only the third reported in the literature in which ACC of the submandibular gland presented in the unusual manner of a liver metastasis in the absence of spread elsewhere [4, 5]. This case highlights important concepts. First, isolated liver metastasis can be the primary pattern of presentation for ACC. Second, expert pathological assessment of the liver specimen is critical in suggesting an atypical primary tumor site. Finally, an interdisciplinary approach to patients with metastatic ACC is critical in managing this rare entity.
Contributor Information
Gaya Spolverato, Department of Surgery, The Johns Hopkins University School of Medicine, 600 N. Wolfe Street, Blalock 688, Baltimore, MD 21287, USA.
Judd Fite, Department of Pathology, The Johns Hopkins University School of Medicine, Baltimore, MD, USA.
Justin Bishop, Department of Pathology, The Johns Hopkins University School of Medicine, Baltimore, MD, USA.
Pedram Argani, Department of Pathology, The Johns Hopkins University School of Medicine, Baltimore, MD, USA.
Timothy M. Pawlik, Email: tpawlik1@jhmi.edu, Department of Surgery, The Johns Hopkins University School of Medicine, 600 N. Wolfe Street, Blalock 688, Baltimore, MD 21287, USA
References
- 1.Matsuba HM, Spector GJ, Thawley SE, Simpson JR, Mauney M, Pikul FJ. Adenoid cystic salivary gland carcinoma. A histopathologic review of treatment failure patterns. Cancer. 1986;57:519–524. doi: 10.1002/1097-0142(19860201)57:3<519::aid-cncr2820570319>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 2.Balducci G, Sagnotta A, Muroni M, Cacchi C, D'Amato A. An unusual case of exclusive liver metastases from adenoid cystic carcinoma of the submandibular gland: a role for surgery? Report of a case. Surgery Today. 2011;41:596–599. doi: 10.1007/s00595-010-4318-9. [DOI] [PubMed] [Google Scholar]
- 3.Spiro RH, Huvos AG, Strong EW. Adenoid cystic carcinoma of salivary origin. A clinicopathologic study of 242 cases. Am J Surg. 1974;128:512–520. doi: 10.1016/0002-9610(74)90265-7. [DOI] [PubMed] [Google Scholar]
- 4.Deshpande AH, Kelkar AA. Hepatic metastasis as an initial manifestation of salivary adenoid cystic carcinoma: cytologic diagnosis. Diagn Cytopathol. 2009;37:45–7. doi: 10.1002/dc.20961. [DOI] [PubMed] [Google Scholar]
- 5.Garg N, Tomar R, Goyal S, Singh UR. Isolated liver metastases in an adenoid cystic carcinoma of the submandibular gland on fine needle aspiration cytology: an unusual presentation. Cyto-pathology. 2014;25:133–140. doi: 10.1111/cyt.12061. [DOI] [PubMed] [Google Scholar]
- 6.Brill LB, II, Kanner WA, Fehr A, et al. Analysis of MYB expression and MYB-NFIB gene fusions in adenoid cystic carcinoma and other salivary neoplasms. Mod Pathol. 2011;24:1169–1176. doi: 10.1038/modpathol.2011.86. [DOI] [PubMed] [Google Scholar]
- 7.Sung MW, Kim KH, Kim JW, et al. Clinicopathologic predictors and impact of distant metastasis from adenoid cystic carcinoma of the head and neck. Arch Otolaryngol Head Neck Surg. 2003;129:1193–1197. doi: 10.1001/archotol.129.11.1193. [DOI] [PubMed] [Google Scholar]
- 8.Aninos D, Koumarianou A, Georgoulakis J, et al. Liver metastasis of adenoid cystic carcinoma of salivary origin: report of a case prepared by ThinPrep method. Cytopathology. 2007;18:268–269. doi: 10.1111/j.1365-2303.2006.00405.x. [DOI] [PubMed] [Google Scholar]
- 9.Mehrotra R, Singh M. Diagnosis of hepatic metastasis of adenoid cystic carcinoma of the salivary gland by fine needle aspiration. Cytopathology. 1999;10:216–217. doi: 10.1046/j.1365-2303.1999.0157a.x. [DOI] [PubMed] [Google Scholar]
- 10.Plafker J, Nosher JL. Fine needle aspiration of liver with metastatic adenoid cystic carcinoma. Acta Cytol. 1983;27:323–325. [PubMed] [Google Scholar]


