Abstract
The current paradigm of bystander cardiopulmonary resuscitation (CPR) blankets a community with training. Recently, the authors have found that high-risk neighborhoods can be identified, and CPR training can be targeted in the neighborhoods in which it is most needed. This article presents a novel method and pilot implementation trial for the HANDDS (identifying High Arrest Neighborhoods to Decrease Disparities in Survival) program. The authors also seek to describe example methods in which the HANDDS program is being implemented in Denver, Colorado. The HANDDS program uses a simple three-step approach: identify, implement, and evaluate. This systematic conceptual framework uses qualitative and quantitative methods to 1) identify high-risk neighborhoods, 2) understand common barriers to learning and performing CPR in these neighborhoods, and 3) implement and evaluate a train-the-trainer CPR Anytime intervention designed to improve CPR training in these neighborhoods. The HANDDS program is a systematic approach to implementing a community-based CPR training program. Further research is currently being conducted in four large metropolitan U.S. cities to examine whether the results from the HANDDS program can be successfully replicated in other locations.
Out-of-hospital cardiac arrest (OHCA) affects more than 420,000 people annually in the United States. For almost 30 years, survival from OHCA in the United States has remained poor, at less than 8%.1 The American Heart Association's (AHA) “chain of survival” has been used to describe the key aspects of OHCA care that have been shown to affect survival: recognition of the arrest and activation of the emergency response system, early cardiopulmonary resuscitation (CPR), rapid defibrillation, effective advanced life support, and integrated postarrest care. The early provision of bystander CPR is vital to surviving OHCA.2 For every 30 patients who receive bystander CPR, one additional life will be saved.3 Communities in Arizona4 and Washington5 that increased bystander CPR have observed a corresponding increase in OHCA survival. In most communities, however, bystander CPR is provided in less than half of all OHCA events, despite public education campaigns and promotion of CPR as a best practice by organizations like the AHA and American Red Cross (ARC).2,6,7
Rationale
The neighborhood where a person arrests may also affect his or her likelihood of receiving CPR and ultimately surviving.3,8–10 Previous research has shown that residents who live in neighborhoods that are primarily Hispanic, African American, or poor are two to three times more likely to have OHCA. When they experience an OHCA, they are 30% less likely to receive CPR and as a result are more likely to be found in asystole or pulseless electrical activity—cardiac rhythms that are associated with a very low likelihood of survival.11–15 Neighborhoods may be high risk secondary to an increased burden of chronic disease,16,17 lack of social cohesion (e.g., wanting to help a neighbor who may have an event),18,19 or underlying associations with poorer health due to lower socioeconomic status.20,21 Therefore, these high-risk neighborhoods (where the incidence of OHCA is high and the prevalence of bystander CPR provision is low) are an important target for public health interventions to help reduce disparities in bystander CPR and to ultimately improve OHCA survival.
Once high-risk neighborhoods are identified, it is important to understand the community barriers for 1) learning and performing bystander CPR, 2) recognizing cardiac arrest symptoms, and 3) potential ways to plan community-based CPR programming that is concordant with community desires for training. In other chronic diseases, this type of community-based participatory research has been integral in designing successful community programs that have addressed health disparity needs. Interventions that have adhered to the principles of community-based participatory research by using culturally sensitive approaches, conducting interventions in settings such as churches22 and barbershops,23 and using local neighborhood residents as health promoters24–26 have been successful in promoting healthy behavior change.
However, to our knowledge no prior research has been conducted in OHCA to see if this type of systematic approach may be successful in reducing health disparities. The objective of this study was to present a novel method and pilot implementation trial for the HANDDS (identifying High Arrest Neighborhoods to Decrease Disparities in Survival) program. The HANDDS program, which is based on behavioral health theory to increase likelihood of action, challenges the traditional paradigm of blanketing a city with CPR training, and moves toward the ultimate goal of focusing scarce public health resources for CPR training in the geographic locations in which it is most needed.
Conceptual Framework
The Health Belief Model (HBM) was originally created in the 1950s and is used to describe and explain why people choose to do certain health activities (e.g., perform CPR). The model has been changed over the years, but it is used to help promote people's readiness to act. It is one of the most widely used health promotion models.27
There are six core concepts in this model that affect a person's likelihood of doing a specific behavior such as performing bystander CPR.28 These core concepts have been applied to the likelihood of performing CPR on a person in cardiac arrest (Figure 1). Perceived susceptibility is a person's belief that a cardiac arrest might happen to him- or herself or a loved one. Perceived severity is a person's belief in the consequences of not performing CPR on a person in cardiac arrest. Perceived benefit is a person's belief that performing CPR will be efficacious and potentially increase the chance of surviving a cardiac arrest event. Perceived barriers is a person's perception of the tangible and psychological consequences of performing CPR. Cues to action are the strategies to activate a person to readiness, such as dispatcher-assisted CPR or community-based CPR educational programs. Self-efficacy is a person's confidence that he or she can perform CPR if the situation arises. Ultimately, for a person to act, the perceived benefits must outweigh the perceived barriers.
Figure 1.
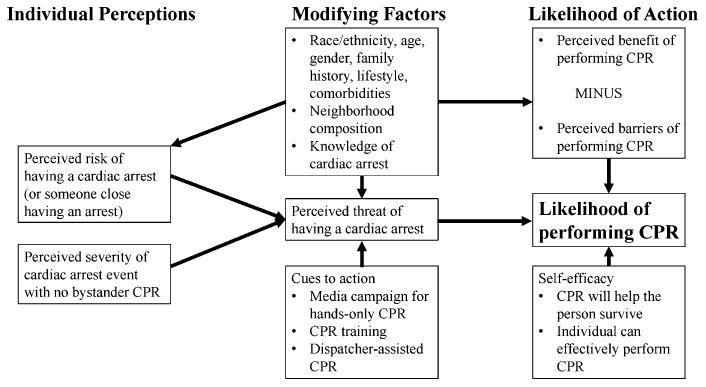
Health Belief Model and likelihood of performing bystander CPR.
HANDDS Program Method
The HANDDS program, which is derived from the HBM, uses a three-phased approach to systematically implementing community-based CPR training programs in the neighborhoods in which it is most needed (Figure 2). The three phases are to identify, implement, and evaluate. We present each phase of the HANDDS program, how it relates to the HBM, and the sample research methods that can be used to implement the HANDDS program based on our Denver-based pilot program. It is important to note that other research methods can be used to complete each phase of the program.
Figure 2.
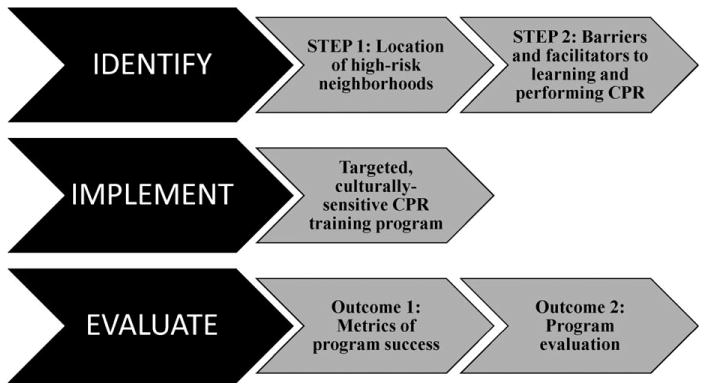
Three-phase HANDDS program approach. HANDDS = identifying High Arrest Neighborhoods to Decrease Disparities in Survival.
Human Subjects Considerations
All research conducted in the HANDDS study was approved by the Colorado Multiple Institutional Review Board. One author (CS) is the principal investigator for all three phases of the HANDDS program. Phase 1 includes a secondary data analysis of the Cardiac Arrest Registry to Enhance Survival (CARES), which is a continuous quality improvement tool and surveillance registry designed to help local officials monitor and improve their provision of prehospital emergency cardiac care. To ensure each patient's confidentiality, case reports are stripped of all individual identifiers before the data are permanently entered in the registry. Each patient receives the standard care available in his or her community, and no patient is subjected to any experimental intervention. In light of these safeguards, the institutional review boards of all participating sites have determined that CARES is exempt from the requirement to secure verbal or written consent.29 Phase 1 step 2, phase 2, and phase 3 are considered expedited studies by the Colorado Multiple Institutional Review Board. All participants sign written consent forms to participate in the studies.
Phase 1: Identify
Step 1: Location of High-risk Neighborhoods
Spatial epidemiologic clustering techniques have been used in infectious disease mapping for more than 20 years to identify outbreaks, trends in disease incidence, and clustering of patients. The HANDDS program uses this method, based on prior research, to identify high-risk neighborhoods for OHCA incidence and low provision of bystander CPR. This “personalizes” the data by giving a community member insight into his or her own perceived susceptibility to having a cardiac arrest and not receiving bystander CPR.
In the Denver-based HANDDS program pilot, we use a five-step spatial analytical process to identify high-risk neighborhoods using existing secondary data of OHCA. We use the standardized data elements from the CARES database. CARES is a surveillance registry that is funded by the AHA, ARC, Medtronic Foundation, and Zoll and is sponsored by the Centers for Disease Control and Prevention and Emory University. CARES links a standard set of data elements from three sources: 9-1-1 call centers, EMS providers, and receiving hospitals. The registry was established in 2005 and includes 40 major U.S. cities and six U.S. states,30 with a catchment area of more than 64 million people.
First, OHCA address data are geocoded into census tracts using ArcGIS software, and census tract socioeconomic and demographic data, obtained from the 2010 Census,31 are added to each OHCA event. Second, adjusted OHCA incidence and proportion of arrests receiving bystander CPR are calculated for each census tract using Spatial Empirical Bayes methods.32 This method adjusts rates toward the average rate of the surrounding census tracts with the amount of shrinkage inversely proportional to the size of the population at risk.32 Third, after calculating adjusted OHCA incidence and bystander CPR, a Local Moran's I statistic is calculated for each census tract with R software.33 Local Moran's I is a measure of local spatial autocorrelation and can be used to identify spatial clusters or hot spots (census tracts where adjacent tracts have similar values) or spatial outliers (tracts with very distinct or different values than their neighbors). Clusters of increased OHCA incidence are then determined if the p-value resulting from nonparametric Monte Carlo simulations is <0.05. Fourth, the process is repeated to identify spatial clusters of low bystander CPR provision by census tract. Finally, an overlay of the high OHCA incidence clusters with the low bystander CPR clusters is conducted to find those high-risk tracts that have both statistically significant high rates of OHCA and low bystander CPR.
Because there is no “standard” method for conducting spatial cluster analysis, a sensitivity analysis is conducted using four other spatial analysis methods: Empirical Bayes adjusted rates,8,34 SatScan,35 Getis-Ord Gi* Statistic,36 and Kernel Density.37 Results are then stratified by a public (outside of the home/residence) versus private (home/residence) location of arrest, with 80% of all arrests occurring in a private location. The p-value is set at <0.05 for all sensitivity analyses. The community-level structural, organizational, economic, and demographic characteristics are then described to understand the composition of each high-risk neighborhood and to inform the census tracts to target in the second step of the identification process.
Step 2: Barriers to Recognition of OHCA and Learning and Performing Bystander CPR
Despite a strong evidence base for CPR, the widespread translation of this practice into the community has not been accomplished.38 Historically, CPR training is based on convenience and is typically offered at workplaces,39,40 schools,41–43 and community events.44,45 This CPR training is not targeted based on needs or tailored to specific social or cultural groups that are less likely to perform CPR. This historical approach to CPR training fails to consider who is getting training, the setting in which the training occurs, and how the training is being delivered. No previous studies have been conducted to understand how these three contributing factors, particularly in certain racial/ethnic and socioeconomic groups, and at the individual and neighborhood levels, may affect a person's likelihood of learning and performing CPR. As a result, we use community-based participatory research with qualitative methods to understand the underlying cause of health disparities in OHCA and provision of bystander CPR in the target neighborhoods and how a tailored, culturally sensitive, neighborhood-based intervention could be designed and implemented in the high-risk neighborhoods identified in step 1.
This step in the HANDDS program allows for a better understanding of community members' perceptions of severity of sustaining OHCA, benefit of performing bystander CPR, and the barriers that may prevent people from performing CPR in an emergency situation. This information is critical to understanding what fears must be overcome and addressed to increase a person's likelihood of action.
In the Denver-based HANDDS program, participants who reside in the identified high-risk neighborhoods are purposefully sampled to participate in focus groups or semistructured key informant interviews carried out by a moderator trained in qualitative methods and in the primary language of the participant. Participants are queried on the barriers to calling 9-1-1, recognition of OHCA symptoms, and learning and performing bystander CPR. Other topics addressed are the neighborhood residents' thoughts on how to design, develop, and implement a community-based CPR training program that is congruent with the needs of the neighborhood residents and provides appropriate incentives to draw in populations that are traditionally difficult to engage in training programs. This formative work provides the basis for the next phase of implementation.46
Phase 2: Implement
The uptake of CPR training and other health interventions has been limited in Hispanics and African Americans.11–15 Health disparities have been reduced in these populations by 1) understanding the social and cultural context of the target population, 2) identifying appropriate settings for the intervention, and 3) working with local community members to design and implement the intervention.47,48 According to the HBM, cues to action (implementing a community-based educational program), as well as increasing a person's self-efficacy (by psychomotor practice of hands-only CPR), are integral in increasing the desired behavior (performing CPR).
Informed by steps 1 and 2 of the identification phase, the next step of the community-based CPR educational program is implementation. In the Denver-based HANDDS program, the implementation strategy is tailored to racial, ethnic, and socioeconomic groups (e.g., Spanish-language for non-English-speaking participants) and is being conducted in local settings based on community preferences (at churches and schools) and using local resources (local bilingual residents as health educators) to implement and disseminate CPR training in high-risk neighborhoods. Careful attention is given to the data collected during these trainings to ensure that the fidelity, scalability, and reproducibility of this targeted, culturally sensitive program is being adequately captured.
In the Denver-based HANDDS program, we conduct a feasibility study of a community-based, culturally sensitive CPR intervention to teach 300 participants how to perform CPR and indirectly teach 600 to 900 friends and family of the 300 participants how to perform CPR using a train-the-trainer approach. The AHA CPR Anytime take-home kit contains an inflatable manikin and a short educational video (in both English and Spanish) that describes when to call 9-1-1 and how to perform hands-only and traditional CPR. The participant watches the video, practices CPR on the manikin, and receives feedback when the correct chest compression depth is achieved. These kits are specifically designed to be used in a train-the-trainer program, and the average kit has been shown in prior studies to train two to three additional people.49,50 Participants are then encouraged to train family and friends on CPR and to keep a record (contact information) of the people they train. We conduct CPR interventions in the community (approximately once a month, alternating locations within the high-risk neighborhoods) with both a didactic session and a hands-on training session. We follow-up with participants, in person, after 2 to 4 weeks to assess the numbers of family and friends they trained through the take-home CPR kit and comfort and knowledge acquisition of the family and friends.
The participants who directly receive the CPR intervention complete a survey pre- and postintervention that assesses their knowledge of and comfort with performing CPR and calling 9-1-1. At 2 to 4 weeks postintervention, the participants are then provided a $10 grocery store gift card as an incentive to bring back both the data collection sheets and the pre- and post-knowledge surveys that were given to five family and friends.
Phase 3: Evaluate
Outcome 1: Metrics for Program Success
Primary outcome measures are 1) the number of people directly trained in CPR, 2) participants' satisfaction with the CPR intervention, 3) participants' knowledge acquisition (via pre- and postintervention knowledge test), and 4) dissemination into the target high-risk neighborhoods (by collecting addresses of the participants who attend the training). Secondary outcome measures are bystander CPR prevalence and OHCA incidence in the high-risk neighborhoods pre- and postintervention and the comfort and knowledge acquisition of family and friends who were educated by the participants.
Outcome 2: Program Evaluation Framework
The intervention can also be evaluated using the Reach Effectiveness Adoption Implementation Maintenance (RE-AIM) measures (Table 1). The RE-AIM framework has been used extensively for evaluating the effectiveness of community-based interventions and is well vetted in the program implementation literature.51–53 This program evaluation framework has been designed to increase the speed in which promising, evidence-based community interventions are translated into the real world. This systematic evaluation framework concentrates on five major areas: reach to the intended target population, efficacy/effectiveness, adoption, implementation consistency, and maintenance of the intervention over time.
Table 1.
RE-AIM Evaluation for Denver HANDDS Program
| Evaluation Measure | Proposed Strategies to Enhance Overall Impact | Outcome Measures to Evaluate Impact | Denver HANDDS Program |
|---|---|---|---|
| REACH: Extent of representativeness of participants | A. Clearly defined target population and numbers of people eligible for he intervention. | Proportion of residents from high-risk neighborhoods who participated in CPR intervention. | 344 participants |
| B. Major barriers and facilitators to CPR intervention identified in step 2 to develop targeted intervention. | Number of settings willing and unwilling to host intervention. Number of residents from high-risk neighborhoods who participated. | No settings were unwilling to host the intervention. 344 participants |
|
| EFFECTIVENESS: Short-term impact/outcomes for participants | A. Tailored messaging approach based on community recommendations. | Postintervention survey assessing the participants' satisfaction with the training, knowledge acquisition, and recommendations for improvement. | Increase in knowledge acquisition from 1.71 (±1.31) to 3.96 (±1.07) out of possible five questions. |
| B. Reinforced CPR intervention with direct training and take-home kit. | In-person follow-up at 2 to 4 weeks to understand how participants felt training family and friends. | 80% of family and friends feel comfortable performing hands-only CPR. | |
| ADOPTION: Interface between researchers and potential program settings | A. Settings for intervention based on community input. | Record which settings were willing or unwilling to participate and why. | Not applicable |
| B. Intervention can be easily conducted in multiple settings with few resources. | Record which settings initially participated and then dropped out and why. | Not applicable | |
| C. Commitment to piloting intervention from key community organizations. | Number of formal local collaborations established by the end of the intervention period. | Continuation of two community-based programs in stroke and hypertension in same populations. | |
| IMPLEMENTATION: Fidelity or intervention integrity | A. Meet with participants who completed the CPR intervention to understand how to make intervention better. | Record number of participants who complete the follow-ups. | 154 participants (44.8% response rate) |
| MAINTENANCE: Both individual participant and program/setting level | A. Reduce level of resources needed for starting and maintaining this type of project. | Creation of a “how-to guide” for the entire intervention that can then be “taken off the shelf” and used in other communities. | In process |
| B. Work with existing network of community organizations locally to develop sustainability plan. | Number of formal local collaborations established by the end of the intervention period. | Continuation of two community-based programs in stroke and hypertension in same populations. |
HANDDS = identifying High Arrest Neighborhoods to Decrease Disparities in Survival; RE-AIM = Reach Effectiveness Adoption Implementation Maintenance.
Discussion
There are major health disparities in the provision of bystander CPR by race, ethnicity, and socioeconomic status. Prior research has shown that residents of primarily black, lower-income neighborhoods are 51% less likely to have bystander CPR performed compared to residents of white, higher-income neighborhoods.55 In addition, these same neighborhoods composed of racial/ethnic minorities and lower-income residents are also more likely to have a higher incidence of cardiac arrest and lower provision of bystander CPR. These neighborhoods are potential high-risk areas that may be targets for community-based interventions to increase the provision of bystander CPR.56
We propose the novel, systematic HANDDS program and method to identify, implement, and evaluate a community-based CPR training program that is focused in the areas where it is most needed and potentially most likely to have the greatest effect. The systematic approach outlined by the HANDDS program has been successfully used in other areas such as community policing and infectious disease to quickly and efficiently address community problems, such as increase in violence near establishments serving alcohol57 or a Chagas disease outbreak.58 However, the HANDDS program's systematic approach, based on the HBM, has never been applied to increasing the likelihood of bystanders performing CPR. Traditional CPR paradigms of offering training to those who seek out the training, can afford it, and speak English have created a culture in which disparities are promulgated and propagated.59 The paradigm must shift, but in a manner in which data and evidence can drive the implementation of this type of community-based CPR programming.
There are three key points that must be in place before the HANDDS program can be used in the community. First, a mechanism for the collection of surveillance data is required to be able to identify the highest-risk neighborhoods and to track the successful adoption or implementation of this program. Second, the buy-in and trust of the community is paramount to the successful implementation and evaluation of this program. Community leaders must be engaged in all aspects of the study. Data collection and analysis must be done in conjunction with community leaders, be transparent, and be shared back with the community. Studies have shown that the most successful community-based programs are ones in which the interventions are conducted in the community, developed by the community residents, and value the residents' time by providing incentives.59 The HANDDS program and method follows these principles and we believe these are important to replicating similar success in other communities. Finally, the sustainability and reproducibility of the program are paramount. In the Denver-based pilot, the biggest barrier faced by the team has been sustainability. Because of the success of the initial pilot, as well as overwhelming community support and engagement, additional funding and community partners have been established to sustain a larger initiative in the area. The goal of this initiative is to integrate hands-only CPR training into the culture of the school system and the community organizations that service the high-risk neighborhoods.
Limitations
There are some potential limitations to this type of systematic approach to community-based CPR training. Future research will need to be conducted to assess how the transition from conceptual framework to actual implementation is carried out. Most importantly, can this systematic approach be replicated in other locations? Current studies are under way in four major metropolitan areas to test the reproducibility of the HANDDS program for the identification of health disparities in OHCA and bystander CPR, followed by targeted, culturally relevant train-the-trainer approaches. The lessons learned from the multiple other sites will provide a perspective on the applicability, sustainability, and reproducibility of this type of program. It is also possible that the steps that we have outlined in this conceptual framework may not be feasible for every community to complete. Finally, further refinement and tailoring of this framework will be needed by each community that chooses to implement this stepwise approach. We believe that this local customization process is inherent to doing community-based educational programming.
Future research is also possible testing how the HANDDS program may function in other disease states. Specifically, the lessons we have learned from developing this program may also be used for other diseases states in which health disparities are present and health care resources are scarce. For example, a similar program could be used for the targeted identification, implementation, and evaluation of a culturally sensitive intervention to reduce sexually transmitted infections, teenage pregnancy, and uncontrolled hypertension. The HANDDS program provides a systematic approach to both targeting resources where they are most needed, and conducting the formative work that ensures that the public health intervention is successful and done in conjunction with the community that it is serving.
Conclusions
There are large health disparities in the provision of bystander cardiopulmonary resuscitation in underserved populations. We have provided a HANDDS program, based on the Health Belief Model, that outlines a rigorous, stepwise approach to changing the paradigm of community bystander CPR training from a one-size-fits-all approach to one that is targeted where the need is the greatest. We hope that the novel HANDDS program will begin to address and correct the disparities we see daily for out-of-hospital cardiac arrest victims in the United States.
Acknowledgments
We acknowledge our community partners and emergency medical services providers who have been integral to the success of the Denver HANDDS Program: Merida Carmonas, Dr. Chris Colwell, Grant Jones, Dr. Kevin McVaney, Mandy Medrano, Charlene Barrientos-Ortiz, Lorenzo Ramirez, and May Tran.
This study was supported by NIH/NCATS Colorado CTSI grant number UL1 TR001082. The contents are the authors' sole responsibility and do not necessarily represent official NIH views. Dr. Haukoos is supported by R01AI106057 from the National Institute of Allergy and Infectious Diseases and R01HS021749 and K02HS017526 from the Agency for Healthcare Research and Quality (AHRQ). Dr. Magid currently receives grant funding from the AHRQ, National Health Lung and Blood Institute, National Institute on Aging, National Center for Advancing Translational Science, American College of Cardiology Foundation, Amgen, and the Patient Centered Outcome Research Institute.
Footnotes
The authors have no potential conflicts of interest to disclose.
References
- 1.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics-2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics-2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117:e25–146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 3.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 4.Bobrow BJ, Spaite DW, Berg RA, et al. Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA. 2010;304:1447–54. doi: 10.1001/jama.2010.1392. [DOI] [PubMed] [Google Scholar]
- 5.Eisenberg MS. Improving survival from out-of-hospital cardiac arrest: back to the basics. Ann Emerg Med. 2007;49:314–6. doi: 10.1016/j.annemergmed.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 6.Cummins RO. Emergency medical services and sudden cardiac arrest: the “chain of survival” concept. Annu Rev Public Health. 1993;14:313–33. doi: 10.1146/annurev.pu.14.050193.001525. [DOI] [PubMed] [Google Scholar]
- 7.American Heart Association. 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and EmergencyCardiovascular Care. Circulation. 2005;112:IV1–203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 8.Sasson C, Keirns CC, Smith D, et al. Small area variations in out-of-hospital cardiac arrest: does the neighborhood matter? Ann Intern Med. 2010;153:19–22. doi: 10.1059/0003-4819-153-1-201007060-00255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sasson C, Keirns CC, Smith DM, et al. Examining the contextual effects of neighborhood on out-of-hospital cardiac arrest and the provision of bystander cardiopulmonary resuscitation. Resuscitation. 2011;82:674–9. doi: 10.1016/j.resuscitation.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iwashyna TJ, Christakis NA, Becker LB. Neighborhoods matter: a population-based study of provision of cardiopulmonary resuscitation. Ann Emerg Med. 1999;34:459–68. doi: 10.1016/s0196-0644(99)80047-x. [DOI] [PubMed] [Google Scholar]
- 11.Brookoff D, Kellermann AL, Hackman BB, Somes G, Dobyns P. Do blacks get bystander cardiopulmonary resuscitation as often as whites? Ann Emerg Med. 1994;24:1147–50. doi: 10.1016/s0196-0644(94)70246-2. [DOI] [PubMed] [Google Scholar]
- 12.Becker LB, Han BH, Meyer PM, et al. Racial differences in the incidence of cardiac arrest and subsequent survival. The CPR Chicago Project N Engl J Med. 1993;329:600–6. doi: 10.1056/NEJM199308263290902. [DOI] [PubMed] [Google Scholar]
- 13.Feero S, Hedges JR, Stevens P. Demographics of cardiac arrest: association with residence in a low-income area. Acad Emerg Med. 1995;2:11–6. doi: 10.1111/j.1553-2712.1995.tb03071.x. [DOI] [PubMed] [Google Scholar]
- 14.Galea S, Blaney S, Nandi A, et al. Explaining racial disparities in incidence of and survival from out-of-hospital cardiac arrest. Am J Epidemiol. 2007;166:534–43. doi: 10.1093/aje/kwm102. [DOI] [PubMed] [Google Scholar]
- 15.Vaillancourt C, Lui A, De Maio VJ, Wells GA, Shell IG. Socioeconomic status influences bystander CPR and survival rates for out-of-hospital cardiac arrest victims. Resuscitation. 2008;79:417–23. doi: 10.1016/j.resuscitation.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 16.Gonzalez MA, Rodriguez Artalejo F, Calero JR. Relationship between socioeconomic status and ischaemic heart disease in cohort and case-control studies: 1960-1993. Int J Epidemiol. 1998;27:350–8. doi: 10.1093/ije/27.3.350. [DOI] [PubMed] [Google Scholar]
- 17.Gregor RD, Bata IR, Eastwood BJ, Wolf HK. Ten-year trends of heart disease risk factors in the Halifax County MONICA population. MONItoring of trends and determinants in Cardiovascular disease. Can J Cardiol. 1998;14:1017–24. [PubMed] [Google Scholar]
- 18.McCarthy M. Social determinants and inequalities in urban health. Rev Environ Health. 2000;15:97–108. doi: 10.1515/reveh.2000.15.1-2.97. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization. Social Determinants of Health. [Accessed Jun 27, 2014]; Available at: http://www.who.int/social_determinants/thecommission/finalreport/key_concepts/en/
- 20.Lynch J, Smith GD, Harper S, Hillemeier M. Is income inequality a determinant of population health? Part 2. U.S. National and regional trends in income inequality and age- and cause-specific mortality. Milbank Q. 2004;82:355–400. doi: 10.1111/j.0887-378X.2004.00312.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lynch J, Smith GD, Hillemeier M, Shaw M, Raghunathan T, Kaplan G. Income inequality, the psychosocial environment, and health: comparisons of wealthy nations. Lancet. 2001;358:194–200. doi: 10.1016/S0140-6736(01)05407-1. [DOI] [PubMed] [Google Scholar]
- 22.Todd KH, Heron SL, Thompson M, Dennis R, O'Connor J, Kellermann AL. Simple CPR: a randomized, controlled trial of video self-instructional cardiopulmonary resuscitation training in an African American church congregation. Ann Emerg Med. 1999;34:730–7. doi: 10.1016/s0196-0644(99)70098-3. [DOI] [PubMed] [Google Scholar]
- 23.Victor RG, Ravenell JE, Freeman A, et al. Effectiveness of a barber-based intervention for improving hypertension control in black men: the BARBER-1 study: a cluster randomized trial. Arch Intern Med. 2011;171:342–50. doi: 10.1001/archinternmed.2010.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ingram M, Torres E, Redondo F, Bradford G, Wang C, O'Toole ML. The impact of promotoras on social support and glycemic control among members of a farmworker community on the US-Mexico border. Diabetes Educ. 2007;33(Suppl 6):172S–8S. doi: 10.1177/0145721707304170. [DOI] [PubMed] [Google Scholar]
- 25.Reinschmidt KM, Hunter JB, Fernandez ML, Lacy-Martinez CR, Guernsey de Zapien J, Meister J. Understanding the success of promotoras in increasing chronic diseases screening. J Health Care Poor Underserved. 2006;17:256–64. doi: 10.1353/hpu.2006.0066. [DOI] [PubMed] [Google Scholar]
- 26.Two Feathers J, Kieffer EC, Palmisano G, et al. Racial and ethnic approaches to community health (REACH) Detroit partnership: improving diabetes-related outcomes among African American and Latino adults. Am J Public Health. 2005;95:1552–60. doi: 10.2105/AJPH.2005.066134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health. 2010;31:399–418. doi: 10.1146/annurev.publhealth.012809.103604. [DOI] [PubMed] [Google Scholar]
- 28.Glanz K, Rimer BK, Lewis FM. Health Behavior and Health Education Theory, Research and Practice. San Francisco, CA: Wiley & Sons; 2002. [Google Scholar]
- 29.Centers for Disease Control and Prevention. CARES IRB Approval and Modification. Sansio; 2007. [Accessed Jul 2, 2014]. Cardiac Arrest Registry to Enhance Survival. (restricted access). Available at: https://www.mycares.net/cares_info.jsp. [Google Scholar]
- 30.McNally B, Robb R, Mehta M, et al. Out-of-hospital cardiac arrest surveillance — Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005-December 31, 2010. MMWR Surveill Summ. 2011;60:1–19. [PubMed] [Google Scholar]
- 31.U.S. Census Bureau. State and County QuickFacts. [Accessed Jun 27, 2014]; Available at: http://quickfacts.census.gov/qfd/index.html#.
- 32.Anselin L. Exploring Spatial Data With GeoDa: A Workbook. Urbana-Champaign, IL: University of Illinois; 2004. [Google Scholar]
- 33.Anselin L, Syabri I, Kho Y. GeoDa: an introduction to spatial data analysis. Geographical Anal. 2006;38:5–22. [Google Scholar]
- 34.Hayward RA, Heisler M, Adams J, Dudley RA, Hofer TP. Overestimating outcome rates: statistical estimation when reliability is suboptimal. Health Serv Res. 2007;42:1718–38. doi: 10.1111/j.1475-6773.2006.00661.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kuldorff M. A spatial scan statistic. Comm Stat Theory Meth. 1997;26:1487–96. [Google Scholar]
- 36.Anselin L. Local Indicators of Spatial Association-LISA. Geographic Anal. 1995;27:93–115. [Google Scholar]
- 37.Waller L, Gotway C. Applied Spatial Statistics for Public Health Data. New York, NY: John Wiley & Sons; 2004. [Google Scholar]
- 38.Abella BS, Aufderheide TP, Eigel B, et al. Reducing barriers for implementation of bystander-initiated cardiopulmonary resuscitation: a scientific statement from the American Heart Association for Healthcare Providers, Policymakers, and Community Leaders regarding the effectiveness of cardiopulmonary resuscitation. Circulation. 2008;117:704–9. doi: 10.1161/CIRCULATIONAHA.107.188486. [DOI] [PubMed] [Google Scholar]
- 39.Axelsson AB, Herlitz J, Holmberg S, Thoren AB. A nationwide survey of CPR training in Sweden: foreign born and unemployed are not reached by training programmes. Resuscitation. 2006;70:90–7. doi: 10.1016/j.resuscitation.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 40.Jennings S, Hara TO, Cavanagh B, Bennett K. A national survey of prevalence of cardiopulmonary resuscitation training and knowledge of the emergency number in Ireland. Resuscitation. 2009;80:1039–42. doi: 10.1016/j.resuscitation.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 41.Cave DM, Aufderheide TP, Beeson J, et al. Importance and implementation of training in cardiopulmonary resuscitation and automated external defibrillation in schools: a science advisory from the American Heart Association. Circulation. 2011;123:691–706. doi: 10.1161/CIR.0b013e31820b5328. [DOI] [PubMed] [Google Scholar]
- 42.Roppolo LP, Pepe PE. Retention, retention, retention: targeting the young in CPR skills training! Crit Care. 2009;13:185. doi: 10.1186/cc7997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Winkelman JL, Fischbach R, Spinello EF. Assessing CPR training: the willingness of teaching credential candidates to provide CPR in a school setting. Educ Health (Abingdon) 2009;22:81. [PubMed] [Google Scholar]
- 44.Azhar AA. Mass cardio-pulmonary resuscitation: a new method of public cardio-pulmonary resuscitation teaching. Med J Malaysia. 1999;54:257–60. [PubMed] [Google Scholar]
- 45.Fong YT, Anantharaman V, Lim SH, Leong KF, Pokkan G. Mass cardiopulmonary resuscitation 99-survey results of a multi-organisational effort in public education in cardiopulmonary resuscitation. Resuscitation. 2001;49:201–5. doi: 10.1016/s0300-9572(01)00312-4. [DOI] [PubMed] [Google Scholar]
- 46.Sasson C, Ramirez L, Medrano M, et al. Barriers to calling 9-1-1 and performing cardiopulmonary resuscitation (CPR) in high-risk neighborhoods in Denver. American Heart Association Resuscitation Science Symposium; November 2012; Los Angeles, CA. [Google Scholar]
- 47.Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav. 2003;30:133–46. doi: 10.1177/1090198102251021. [DOI] [PubMed] [Google Scholar]
- 48.Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethnicity Dis. 1999;9:10–21. [PubMed] [Google Scholar]
- 49.Lorem T, Steen PA, Wik L. High school students as ambassadors of CPR-a model for reaching the most appropriate target population? Resuscitation. 2010;81:78–81. doi: 10.1016/j.resuscitation.2009.09.030. [DOI] [PubMed] [Google Scholar]
- 50.Potts J, Lynch B. The American Heart Association CPR Anytime Program: the potential impact of highly accessible training in cardiopulmonary resuscitation. J Cardiopulm Rehabil. 2006;26:346–54. doi: 10.1097/00008483-200611000-00002. [DOI] [PubMed] [Google Scholar]
- 51.Glasgow RE, McKay HG, Piette JD, Reynolds KD. The RE-AIM framework for evaluating interventions: what can it tell us about approaches to chronic illness management? Patient Educ Couns. 2001;44:119–27. doi: 10.1016/s0738-3991(00)00186-5. [DOI] [PubMed] [Google Scholar]
- 52.Glasgow RE, Fisher EB, Haire-Joshu D, Goldstein MG. National Institutes of Health science agenda: a public health perspective. Am J Public Health. 2007;97:1936–8. doi: 10.2105/AJPH.2007.118356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dzewaltowski DA, Glasgow RE, Klesges LM, Estabrooks PA, Brock E. RE-AIM: evidence-based standards and a Web resource to improve translation of research into practice. Ann Behav Med. 2004;28:75–80. doi: 10.1207/s15324796abm2802_1. [DOI] [PubMed] [Google Scholar]
- 54.Virginia Polytechnic Institute and State University. Reach Effectiveness Adoption Implementation Maintenance (RE-AIM) [Accessed Jun 8, 2014]; Available at: http://www.re-aim.hnfe.vt.edu/
- 55.Sasson C, Magid DJ, Chan P, et al. Association of neighborhood characteristics with bystander-initiated CPR. N Engl J Med. 2012;367:1607–15. doi: 10.1056/NEJMoa1110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sasson C, Meischke H, Abella BS, et al. Increasing cardiopulmonary resuscitation provision in communities with low bystander cardiopulmonary resuscitation rates: a science advisory from the American Heart Association for healthcare providers, policymakers, public health departments, and community leaders. Circulation. 2013;127:1342–50. doi: 10.1161/CIR.0b013e318288b4dd. [DOI] [PubMed] [Google Scholar]
- 57.Zhu L, Gorman DM, Horel S. Alcohol outlet density and violence: a geospatial analysis. Alcohol Alcoholism. 2004;39:369–75. doi: 10.1093/alcalc/agh062. [DOI] [PubMed] [Google Scholar]
- 58.Levy MZ, Bowman NM, Kawai V, et al. Spatial patterns in discordant diagnostic test results for Chagas disease: links to transmission hotspots. Clin Infect Dis. 2009;48:1104–6. doi: 10.1086/597464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sasson C, Haukoos JS, Bond C, et al. Barriers and facilitators to learning and performing cardiopulmonary resuscitation in neighborhoods with low bystander cardiopulmonary resuscitation prevalence and high rates of cardiac arrest in Columbus, OH. Circ Cardiovasc Qual Outcomes. 2013;6:550–8. doi: 10.1161/CIRCOUTCOMES.111.000097. [DOI] [PMC free article] [PubMed] [Google Scholar]


