Abstract
We herein describe a case of a solitary metastasis of renal cell carcinoma (RCC) in the third ventricle, which was totally removed via an interhemispheric trans-callosal trans-choroidal approach. The histological examination revealed a solitary metastasis of RCC. The postoperative course was uneventful. A stereotactic cyber knife was additionally used for the tumor cavity. As of 2 years after surgery, the patient has been doing well without recurrence. This case highlights the urgent need for an early diagnosis and surgical treatment for solitary metastasis of RCC to the third ventricle due to its critical course.
Keywords: Interhemispheric transcallosal approach, metastatic tumor, third ventricle
Introduction
A choroid plexus metastasis from renal cell carcinoma (RCC) is very rare and has a propensity for intratumoral hemorrhage and massive surrounding edema compared with other metastatic tumors.[1,2,3,4,5] We herein describe the case of a solitary metastasis of RCC to the third ventricle, which resulted in acute neurological deterioration due to acute hydrocephalus. In practice, this case highlights the need for urgent gross total removal via an interhemispheric trans-callosal trans-choroidal approach. We herein discuss this case, with an emphasis on the surgical therapeutic aspects.
Case Report
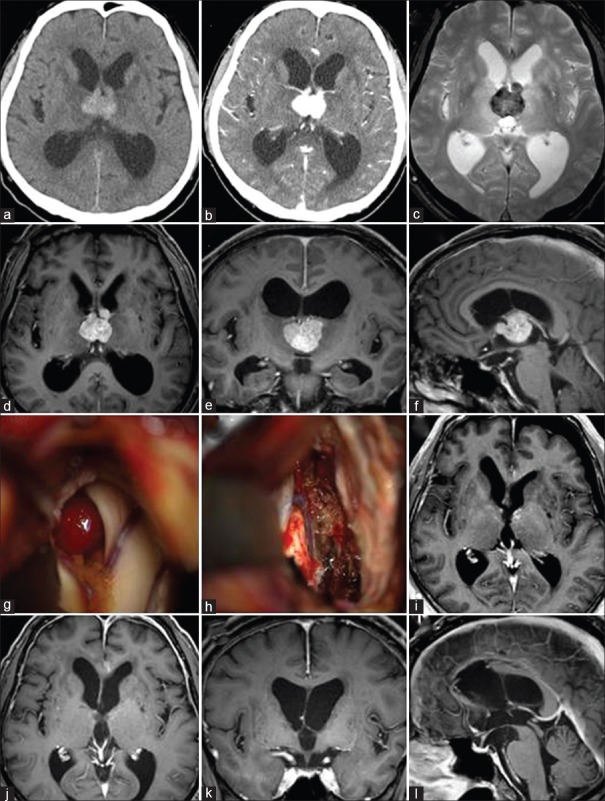
A 68-year-old male was admitted to our hospital because of progressive worsening of cognitive function and gait disturbance. Five years prior to this presentation, the patient had undergone nephrectomy for RCC and had a medical history of irradiation (50 Gy) and oral 5-fluorouracil treatment. The patient appeared drowsy upon a neurological examination on admission. A computed tomography scan showed a high-density mass in the third ventricle and ventricular dilatation [Figure 1a]. The mass lesion exhibited homogenous enhancement with perifocal edema [Figure 1b]. The enhanced T1-weighted image showed that a solitary mass lesion was located in the third ventricle with attachment to the roof of the third ventricle [Figure 1d–f]. The T2-weighted star image showed the lesion as a hypo-intense mass that indicated the intratumoral hemorrhage [Figure 1c]. Preoperative positron emission tomography scan showed that there was no accumulation of the tracer in the whole body, which suggested that solitary lesion. Preoperative Karnofsky Performance Status (KPS) showed as a score of 40, which suggested in a dependent manner. Surgical resection of the tumor was performed via an interhemispheric trans-callosal trans-choroidal approach. The intraoperative findings showed that the tumor was elastic hard, hemorrhagic-, and attached to the velum interpositum [Figure 1g and h]. The tumor was dissected while the internal cerebral veins were spared. Gross total removal was successfully accomplished. A postoperative enhanced magnetic resonance imaging showed improvement of the hydrocephalus and total removal of the tumor [Figure 1i]. The histological examination revealed a metastasis of RCC. The patient's postoperative course was uneventful. A stereotactic cyber knife was applied for the tumor cavity. As of 2 years after surgery, follow-up enhanced magnetic resonance imaging showed no recurrence [Figure 1j–l] and the postoperative KPS showed as a score of 100 in a independent manner, the patient has been doing well.
Figure 1.
A computed tomography scan and the enhanced T1-weighted image showed an abnormal mass in the third ventricle and ventricular dilatation (a, b, d-f). The T2-weighted star image showed the lesion as a hypo-intense mass that indicated the intratumoral hemorrhage (c) surgical tumor removal was performed via an interhemispheric trans-callosal trans-choroidal approach (g) gross total removal was successfully accomplished (h) a postoperative enhanced magnetic resonance imaging showed improvement of the hydrocephalus and total removal of the tumor (i) as of 2 years after surgery, follow-up enhanced magnetic resonance imaging showed no recurrence (j-l)
Discussion
Renal cell carcinoma is one of the primary cancers that most frequently metastasizes to the brain, although RCC accounts for only 1% of all cancers. The metastasis of RCC to the brain occurs in about 10% of RCC patients.[6] However, choroid plexus metastasis of RCC is very rare.[1,2,3,4] In particular, there have been only two reports of a solitary metastasis to the third ventricle, including our present case.[4] Recently, Shapira et al.[7] summarized the overall clinical outcome regarding in 614 patients with brain metastasis, of whom 24 (3.9%) were diagnosed with RCC. Thus, nine of the 24 patients (37.5%) presented with an intraventricular location. On the other hand, of the remaining 590 patients with non-RCC pathologies, only five patients (0.8%) were diagnosed with intraventricular lesions (P < 0.0001). Brain metastasis caused by RCC significantly presented as an intraventricular mass.
Renal cell carcinomas are divided into two types; a slowly progressive type and a rapidly progressive type. This unusual biological behavior of the tumor leads to a late onset of neurological symptoms although a tumor located in the choroid plexus usually leads to early obstructive hydrocephalus.[1,5] In addition, metastatic tumors from RCC have a propensity to exhibit intratumoral hemorrhage and relatively massive surrounding edema compared with other metastatic tumors.[7] These characteristics emphasize the need for surgical resection in the management of metastatic RCC.
The therapy of choice for metastatic RCC is surgical resection plus irradiation or irradiation alone, including gamma knife surgery (GKS). Iwatsuk et al.[8] reviewed the records from 158 consecutive patients who underwent stereotactic radiosurgery (SRS) for 531 brain metastases from RCC and showed that the overall survival after SRS was 60%, 38%-, and 19% at 6, 12-, and 24 months, respectively, with a median survival of 8.2 months. Kano et al.[9] showed that the overall median survival time after GKS was 9.5 months. These reports showed that the KPS score appeared to be a more important factor in predicting survival than any other factor. In the present case, the patient suffered from progressive neurological deterioration, leading to a low KPS score. In addition, the radiological findings showed that the mass lesion was located within the third ventricle with acute hydrocephalus. Therefore, we performed emergency surgical removal of the tumor, and GKS was subsequently performed to remove any remnant malignant cells.
When considering the treatment of a metastasis from RCC to the third ventricular choroid plexus, as in the present case, both surgery and radiation therapy must be considered carefully because of the risks of damage to peripheral structures and bleeding from the tumor. In the present case, the tumor was totally removed using an interhemispheric trans-callosal trans-choroidal approach without leading to any neurological deficit. Opening through the body portion of the choroidal fissure from the lateral ventricle exposes the velum interpositum, through which the internal cerebral veins course, and makes it possible to access the third ventricle.[10,11] The intraoperative findings in the present case showed that the attachment of the tumor was to the choroid plexus of the velum interpositum. This approach may be suitable for such tumors because it spares the internal cerebral veins while allowing for the immediate dissection of the attached tumor.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Lauretti L, Fernandez E, Pallini R, Massimi L, Albanese A, Denaro L, et al. Long survival in an untreated solitary choroid plexus metastasis from renal cell carcinoma: Case report and review of the literature. J Neurooncol. 2005;71:157–60. doi: 10.1007/s11060-004-9653-5. [DOI] [PubMed] [Google Scholar]
- 2.Quinones-Hinojosa A, Chang EF, Khan SA, Lawton MT, McDermott MW. Renal cell carcinoma metastatic to the choroid mimicking intraventricular meningioma. Can J Neurol Sci. 2004;31:115–20. doi: 10.1017/s0317167100002948. [DOI] [PubMed] [Google Scholar]
- 3.Sadatomo T, Yuki K, Migita K, Taniguchi E, Kodama Y, Kurisu K. Solitary brain metastasis from renal cell carcinoma 15 years after nephrectomy: Case report. Neurol Med Chir (Tokyo) 2005;45:423–7. doi: 10.2176/nmc.45.423. [DOI] [PubMed] [Google Scholar]
- 4.Tomiyama A, Nakayama H, Aoki K, Ueda M. Solitary metastasis of renal cell carcinoma to the third ventricular choroid plexus with rapid clinical manifestation by intratumoral hemorrhage. Neurol India. 2008;56:179–81. doi: 10.4103/0028-3886.41997. [DOI] [PubMed] [Google Scholar]
- 5.Matsumura H, Yoshimine T, Yamamoto S, Maruno M, Hayakawa T, Ono Y, et al. Single solitary metastasis of the slowly progressive type of renal cell carcinoma to the choroid plexus - Case report. Neurol Med Chir (Tokyo) 1997;37:916–9. doi: 10.2176/nmc.37.916. [DOI] [PubMed] [Google Scholar]
- 6.Sivaramakrishna B, Gupta NP, Wadhwa P, Hemal AK, Dogra PN, Seth A, et al. Pattern of metastases in renal cell carcinoma: A single institution study. Indian J Cancer. 2005;42:173–7. [PubMed] [Google Scholar]
- 7.Shapira Y, Hadelsberg UP, Kanner AA, Ram Z, Roth J. The ventricular system and choroid plexus as a primary site for renal cell carcinoma metastasis. Acta Neurochir (Wien) 2014;156:1469–74. doi: 10.1007/s00701-014-2108-7. [DOI] [PubMed] [Google Scholar]
- 8.Iwatsuki K, Sato M, Taguchi J, Fukui T, Kiyohara H, Yoshimine T, et al. Choroid plexus metastasis of renal cell carcinoma causing intraventricular hemorrhage: A case report. No Shinkei Geka. 1999;27:359–63. [PubMed] [Google Scholar]
- 9.Kano H, Iyer A, Kondziolka D, Niranjan A, Flickinger JC, Lunsford LD. Outcome predictors of gamma knife radiosurgery for renal cell carcinoma metastases. Neurosurgery. 2011;69:1232–9. doi: 10.1227/NEU.0b013e31822b2fdc. [DOI] [PubMed] [Google Scholar]
- 10.Shuto T, Inomori S, Fujino H, Nagano H. Gamma knife surgery for metastatic brain tumors from renal cell carcinoma. J Neurosurg. 2006;105:555–60. doi: 10.3171/jns.2006.105.4.555. [DOI] [PubMed] [Google Scholar]
- 11.Nagata S, Rhoton AL, Jr, Barry M. Microsurgical anatomy of the choroidal fissure. Surg Neurol. 1988;30:3–59. doi: 10.1016/0090-3019(88)90180-2. [DOI] [PubMed] [Google Scholar]