Figure 1.
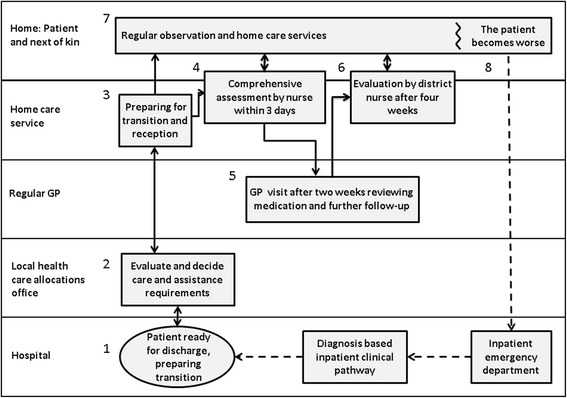
Generic care pathway (PaTH), for transition from hospital and follow-up of home care recipients [ 2 ] . The boxes represent procedures and checklists and the arrows the flow of information between involved parties. It starts with the patient being reported ready for discharge and information is exchanged (1, 2 and 3). Within three days a home care nurse performs a thorough and structured assessment (4). The patient has a consultation with the GP 14 days after discharge (5), and a nurse or nursing assistant performs an extended assessment during the first four weeks (6). A daily care plan is continuously updated (7), and if the patient’s condition gets worse, the home care service has a routine for what to observe, whom to contact and which information to pass on (8). The checklists included practical issues (e.g. whether assistive devices had been ordered and when they would be installed), health issues (e.g. review of medication), social conditions (e.g. if the present accommodation was appropriate for the patients’ level of functioning) and physical and cognitive functioning (e.g. ability to climb stairs, reduced memory). Some checklists were to be used by nurses only (3 and 4), while others were also to be used by nursing assistants (6 and 8). All of the issues on the lists were not necessarily relevant for all patients and the nurses and nursing assistants had to use their professional insight to decide what to assess and how to follow-up.
