Abstract
Purpose
The aim of this work is to investigate the role of power Doppler sonography as an additional predictor of surgical recurrence in Crohn’s disease.
Methods
A sample of 33 patients, with ileal or ileocolonic Crohn’s disease, that had underwent intestinal resection, were retrospectively enrolled. All patients had bowel ultrasonography 7–16 months after resection. Power Doppler sonography of the preanastomotic ileum was evaluated as a possible prognostication tool to assess the risk of long-term need for reoperation.
Results
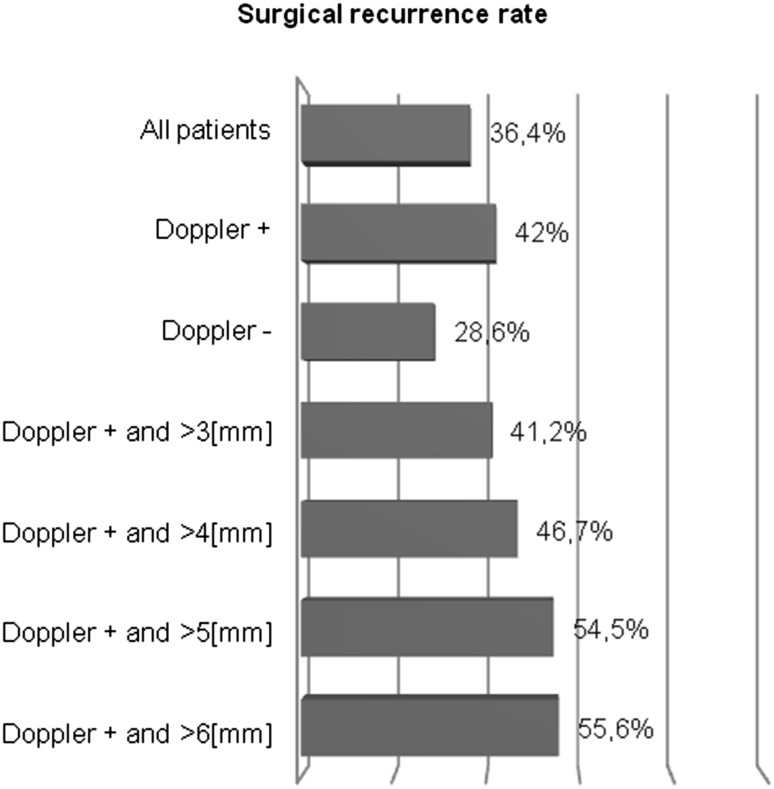
The absolute incidence of surgical recurrence in those who had a positive power Doppler was 42 %, while that of those who had a negative power Doppler was 28.6 %. Combining the power Doppler with bowel wall thickness, the surgical recurrence risk grew from 41.2 % of those with a positive power Doppler and thickness >3 mm to 55.6 % of those with a positive power Doppler and thickness >6 mm.
Conclusions
Power Doppler look to be another useful prediction tool for the personalization of patient’s care. It could be useful to perform power Doppler in all patients with a wall thickness >5 mm: for those who have a positive power Doppler it may be indicated as a more aggressive prophylactic therapy.
Keywords: Color Doppler, Inflammation, Small bowel, Ultrasound
Riassunto
Scopo
L’obiettivo di questo lavoro è investigare il ruolo del power Doppler ecografico come fattore predittivo aggiuntivo della recidiva chirurgica nella malattia di Crohn.
Metodo
Un campione di 33 pazienti, con malattia di Crohn ileale o ileo-colica, che sono stati sottoposti a resezione intestinale, sono stati arruolati retrospettivamente. A tutti i pazienti è stata effettuata un’ecografia intestinale nei 7–16 mesi successivi alla resezione. E’ stato valutato il power Doppler ecografico dell’ileo pre-anastomotico come un possibile predittore del rischio di necessità di una nuova operazione nel lungo termine.
Risultati
L’incidenza assoluta di recidiva chirurgica nei pazienti con power Doppler positivo è risultata essere del 42 %, mentre quella nei pazienti con power Doppler negativo è risultata essere del 28.6 %. Unendo i risultati del power Doppler con quelli dello spessore di parete, il rischio di recidiva chirurgica aumenta dal 41.2 % di quelli con power Doppler positivo e spessore di parete intestinale >3 mm al 55.6 % di quelli con power Doppler positivo e spessore di parete >6 mm.
Conclusioni
Il power Doppler sembra essere un ulteriore utile fattore predittivo per personalizzare la terapia del paziente. Potrebbe essere utile valutare il power Doppler in tutti i pazienti con uno spessore di parete intestinale maggiore di 5 mm: per i pazienti con un risultato positivo al power Doppler potrebbe essere indicata una terapia profilattica più aggressiva.
Introduction
In a previous study [1], we found that bowel wall thickness at the anastomosis >3 mm, detected through bowel ultrasound performed 1 year after surgery, could be added to the list of non-invasive predictors of early recurrence after ileocolonic resection besides those implying a double risk of recurrence, such as smoking, previous bowel surgery, penetrating behavior of the disease, perianal location, extensive small bowel resection, and absence of prophylactic treatment [2].
In recent years, power Doppler has been proposed as an additional prognostication tool to increase the accuracy of bowel ultrasound in the assessment of disease activity [3–5].
A wide deployment of these additional techniques is impaired by the intrinsic variability. It has been also proposed that the morphological characteristics of the intestinal wall correlate with the histological pattern [6, 7] and with the clinical activity [8–11], although the correlation between the intestinal wall thickness and Crohn’s disease activity index (CDAI) is not close [12].
Methodology
We performed a retrospective study on 196 patients, who underwent ileal or ileocolonic resection with ileocolonic anastomosis between December 1993 and March 2009 (all diagnosis of Crohn’s disease was confirmed through histologic examination). All patients underwent bowel ultrasound after at least 6 months from surgery; in this study, we analyzed a total of 33 patients who were evaluated by power Doppler.
The study was reviewed and authorized by the local ethical committee.
Bowel ultrasound was performed using the following ultrasonographic equipments: ESAOTE AU4, ESAOTE Technos, ESAOTE MyLab 70, and TOSHIBA Aplio. A first evaluation of the bowel was made with a convex transducer (frequency 3.5 MHz) and then with a high frequency linear-array transducer (7.5–10 MHz); power Doppler was performed at the preanastomotic ileum.
The four ultrasonographers who performed the examinations were all radiologists with at least 3 years of experience in ultrasound scanning of patients with intestinal bowel diseases and all working in the same department. Each investigation was performed by one radiologist, C. T., S. A., R. D., D. P., who, respectively, performed 11, 10, 7 and 5 investigations. During the procedure, the involved tract wall was examined in a transverse section, from the central hyperechoic line of the lumen to the outer hyperechoic margin of the wall with a linear-array transducer. Wall thickness of the ileocolonic anastomosis was calculated as the average of at least three measurements; at the end of the US investigation, measurements of intestinal wall and power Doppler results at the ileocolonic anastomosis level were reported on a standardized form. Flow was considered to be present when colored pixels could be constantly reproduced in the area of interest or when flowmetric signals could be documented by spectral analysis of the pulsed color Doppler signal. Color Doppler flow was subjectively characterized either as positive (clearly visible, i.e., numerous color signals distributed within and/or around the inflammatory mass or clear identification of vessel paths or minimally visible; i.e., few and/or scattered color signals) or negative (no color signal obtained either inside the lesion or in the periphery).
Ileocolonoscopy was performed in a little percentage of patients and at a different time than bowel ultrasound (due to the invasiveness of this type of exam in patients with resection of the ileum for Crohn’s disease), therefore it is impossible to prove any correlation.
The CDAI was calculated in the follow-up visits.
Statistical analysis
Statistical analysis was performed by using MedCalc software (version 9.2.1.0). The relative risk was calculated with a confidence interval of 95 %.
Results
Clinical characteristics of the study population are reported in Table 1.
Table 1.
Characteristics of the study population (n = 33, Crohn’s disease patients)
| Males/females | 18/15 |
| Median age, years (range) | 44 (24–72) |
| Duration of Crohn’s disease, years (range) | 12 (0–54) |
| Smoking habit at surgery, n (%) | |
| Ever smoker | 15 (45.5) |
| Never smoker | 18 (54.5) |
| Previous surgery, n (%) | |
| Never | 17 (51.5) |
| 1 | 13 (39.4) |
| 2 | 1 (3.0) |
| >2 | 2 (6.1) |
| Total length of bowel resection (cm) | |
| <50 | 20 (60.6 %) |
| ≥50 | 13 (39.4 %) |
| Indication for surgery, n (%) | |
| Strictures | 20 (60.6) |
| Fistula | 5 (15.2) |
| Refractoriness to medical therapy | 6 (18.2) |
| Perforation | 2 (6.1) |
Other data: 28 patients were clinically inactive (CDAI <150 at the time of the bowel ultrasound); bowel ultrasound was performed after a mean time of 13 months (range 7–16 months) after surgery.
The average follow-up was 95 months (range 25–156 months) after surgery.
Major surgical complications occurred in 5 out of the 33 patients (15 %). Clearly, our final analysis refers to the reoperation for the disease recurrence and not to the reoperation for these immediate complications (Table 2).
Table 2.
Major surgical complications
| Patients with major surgical complications | 5 (15 %) |
| Complications | |
| Anastomotic dehiscence | 2 |
| Enterocutaneous fistula | 1 |
| Hemorrhage | 1 |
| Venous thrombosis | 1 |
| Reoperation | 2 |
| Number of patients with anastomosis wall thickness >3 mm 1 year after operation | 5 (100 %) |
| Number of patients with surgical recurrence | 3 (60 %) |
The rate of surgical recurrence for the whole population was 36.4 % (12 of 33 patients), at a mean distance of 50 months from previous surgery (range 20–144 months).
Discussion
Although a sample of 33 patients is not very a large one, considering that power doppler in real world is usually assessed only in a subgroup of patients who underwent bowel ultrasound and the follow-up of 95 months is long enough, this looks to be the first case in the literature in which the predictive power of color Doppler for the surgical recurrence of Crohn’s disease is assessed.
Out of 33 patients, 19 of them had a positive power Doppler after surgery and this seems to be linked to the fact that color Doppler in clinical practice is performed mostly in patients with a thickened bowel wall and, thus, with a greater probability of active disease.
The surgical recurrence was found to be 36.4 %; this percentage is higher than the 20.4 % found in our previous study [1]; this seems linked to the fact that the population in which the power Doppler is normally assessed usually has an increased risk of recurrence (increased thickness of intestinal wall).
Patients with positive power Doppler at the anastomosis run a relative risk = 1.5 (95 % CI = 0.6–3.9) of undergoing surgery compared to patients with negative power Doppler.
The RR of surgical recurrence of those with positive color Doppler compared to those with negative color Doppler does not reach the statistical significance, since there is a selection bias of the population, as there are very few patients with negative power Doppler and physiological thickness of the wall (those who have physiological thickness of the wall generally will not be evaluated by power Doppler in real world, which is the setting of our study).
The RR of surgical recurrence for patients with positive power Doppler and a bowel wall thickness at the anastomosis >3 mm (18 patients), 4 mm (16 patients), 5 mm (12 patients), 6 mm (10 patients), respectively, compared to patients with negative power Doppler and lower bowel thickness is shown in Table 3.
Table 3.
RR of surgical recurrence
| Power Doppler positive and wall thickness at the anastomosis (mm) | RR |
|---|---|
| >3 | 1.3 (95 % CI = 0.5/3.3) |
| >4 | 1.7 (95 % CI = 0.7/4.2) |
| >5 | 2.0 (95 % CI = 0.8/4.8) |
| >6 | 1.9 (95 % CI = 0.8/4.5) |
The RR of patients with positive power Doppler and increased wall thickness does not reach the statistical significance compared to those with negative power Doppler and lower wall thickness because of the smaller sample size compared to our previous study [1] (in fact, only a limited number of patients who underwent bowel ultrasound were assessed using power Doppler).
The absolute incidence of new surgical intervention was 28.6 % in patients with negative power Doppler, 42 % with positive power Doppler, 41.2 % with positive power Doppler and thickness >3 mm, 46.7 % with positive power Doppler and thickness >4 mm, 54.5 % with positive power Doppler and thickness >5 mm, and, finally, 55.6 % with positive power Doppler and thickness >6 mm (Fig. 1).
Fig. 1.
Surgical recurrence rate
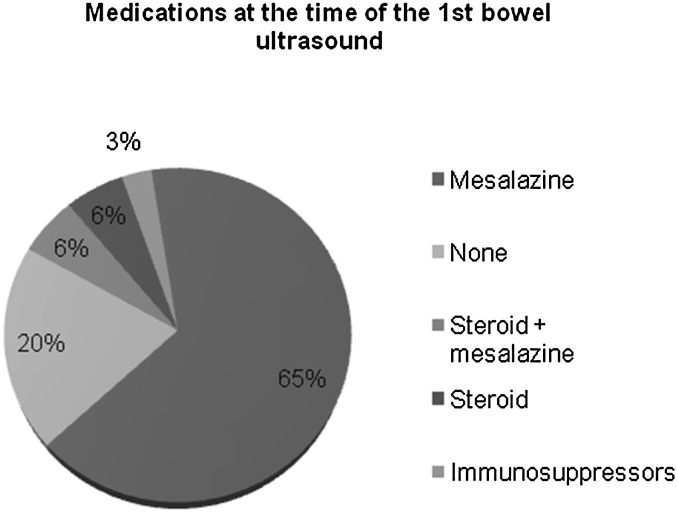
As far as the therapy, the percentage of patients not taking prophylactic therapy of post-surgical recurrence fell from 31.1 % of the previous study [1] to 20 %; only 12 % of patients were receiving steroids and 3 % immunosuppressive agents (Fig. 2).
Fig. 2.
Medications at the time of the bowel ultrasound
The percentage of patients with positive power Doppler that had taken steroids or immunosuppressants or biologics at the time of bowel ultrasound (2 out of 19, 10.5 %) is similar to that of the whole population (5 out of 33, 15 %).
Some critical issues should be considered. The retrospective design of the study represents a limitation, and this is the reason why the color Doppler has been assessed mainly in patients with thickened bowel wall, but this is exactly what happens in daily clinical practice; in addition, the examinations have been assessed by the same group of radiologists and all patients were treated along the years by the same doctor (A. M.).
In conclusion, it seems we have found another useful factor for the personalization of patient’s care: knowing that 54.5 % of patients who performed bowel ultrasound within 1 year after operation and showed both a bowel wall thickness >5 mm and a positive power Doppler will be reoperated, this could help in selecting the patients who should undergo colonoscopy for assessing the endoscopic recurrence and suggest the use of a more aggressive medical therapy to try to change the natural history of their disease.
A prospective study would also be useful, where the population with bowel wall thickness >5 mm within 1 year after surgery would be assessed by color Doppler; those with positive color Doppler should undergo colonoscopy for assessing endoscopic recurrence and should be treated with more aggressive drugs (topical or systemic steroids, immunosuppressants, biological agents) to modify the disease behavior and to extend their surgical recurrence-free interval.
Conflict of interest
We have no conflict of interest.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. All patients provided written informed consent to enrolment in the study and to the inclusion in this article of information that could potentially lead to their identification.
Human and animal studies
The study was conducted in accordance with all institutional and national guidelines for the care and use of laboratory animals.
References
- 1.Cammarota T, Ribaldone DG, Resegotti A, Repici A, Danese S, Fiorino G, et al. Role of bowel ultrasound as a predictor of surgical recurrence of Crohn’s disease. Scand J Gastroenterol. 2013;48:552–555. doi: 10.3109/00365521.2013.777774. [DOI] [PubMed] [Google Scholar]
- 2.Bernstein C, Rawsthorne P, Cheang M, Blanchard JF. A population-based case control study of potential risk factors for IBD. Am J Gastroenterol. 2006;101:993–1002. doi: 10.1111/j.1572-0241.2006.00381.x. [DOI] [PubMed] [Google Scholar]
- 3.Esteban JM, Aleixandre A, Hurtado MJ, Maldonado L, Mora FJ, Nogues E. Contrast-enhanced power Doppler ultrasound in the diagnosis and follow-up of inflammatory abdominal masses in Crohn’s disease. Eur J Gastroenterol Hepatol. 2003;15:253–259. doi: 10.1097/00042737-200303000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Robotti D, Cammarota T, Debani P, Sarno A, Astegiano M. Activity of Crohn disease: value of color-power-Doppler and contrast-enhanced ultrasonography. Abdom Imaging. 2004;29:648–652. doi: 10.1007/s00261-003-0157-0. [DOI] [PubMed] [Google Scholar]
- 5.Bolondi L, Gaiani S, Brignola C, Campieri M, Rigamonti A, Zironi G, et al. Changes in splanchnic hemodynamics in inflammatory bowel disease. Non-invasive assessment by Doppler ultrasound flowmetry. Scand J Gastroenterol. 1992;27:501–507. doi: 10.3109/00365529209000112. [DOI] [PubMed] [Google Scholar]
- 6.Parente F, Maconi G, Bollani S, Anderloni A, Sampietro G, Cristaldi M, et al. Bowel ultrasound in assessment of Crohn’s disease and detection of related small bowel strictures: a prospective comparative study versus X ray and intraoperative findings. Gut. 2002;50:490–495. doi: 10.1136/gut.50.4.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maconi G, Carsana L, Fociani P, Sampietro GM, Ardizzone S, Cristaldi M, et al. Small bowel stenosis in Crohn’s disease: clinical, biochemical and ultrasonographic evaluation of histological features. Aliment Pharmacol Ther. 2003;18:749–756. doi: 10.1046/j.1365-2036.2003.01673.x. [DOI] [PubMed] [Google Scholar]
- 8.Mayer D, Reinshagen M, Mason RA, Muche R, von Tirpitz C, Eckelt D, et al. Sonographic measurement of thickened bowel wall segments as a quantitative parameter for activity in inflammatory bowel disease. Z Gastroenterol. 2000;38:295–300. doi: 10.1055/s-2000-14875. [DOI] [PubMed] [Google Scholar]
- 9.Haber HP, Busch A, Ziebach R, Stern M. Bowel wall thickness measured by ultrasound as a marker of Crohn’s disease activity in children. Lancet. 2000;355:1239–1240. doi: 10.1016/S0140-6736(00)02092-4. [DOI] [PubMed] [Google Scholar]
- 10.Castiglione F, deSio I, Cozzolino A, Rispo A, Manguso F, Del Vecchio Blanco G. Bowel wall thickness at abdominal ultrasound and the one-year-risk of surgery in patients with Crohn’s disease. Am J Gastroenterol. 2004;99:1977–1983. doi: 10.1111/j.1572-0241.2004.40267.x. [DOI] [PubMed] [Google Scholar]
- 11.Maconi G, Parente F, Bollani S, Cesana B, Bianchi Porro G. Abdominal ultrasound in the assessment of extent and activity of Crohn’s disease: clinical significance and implication of bowel wall thickening. Am J Gastroenterol. 1996;91:1604–1609. [PubMed] [Google Scholar]
- 12.Best WR, Becktel JM, Singleton JW. Rederived values of the eight coefficients of the Crohn’s disease activity index (CDAI) Gastroenterology. 1979;77:843–846. [PubMed] [Google Scholar]