Abstract
Objectives:
To evaluate associations of sleep duration with total mortality and disease-specific mortality in a Chinese population.
Design:
Prospective study conducted from 1996 (for women)/2002 (for men) to 2010.
Setting:
A population-based cohort study in Shanghai, China.
Intervention:
None.
Measurements and Results:
A total of 113,138 participants (68,548 women and 44,590 men) of the Shanghai Women's and Men's Health Studies, aged 44–79 y and 40–75 y (women and men, respectively) at sleep duration assessment, were included in the study. In-person interviews were conducted to collect information on sleep duration, socioeconomic status, living conditions, history of chronic disease, participation in regular exercise, and family history of disease. The cohort has been followed using a combination of biannual in-person interviews and record linkages with Shanghai's population-based death registry. Survival status of participants on December 31, 2010 was included as the study outcome. Relative risks were calculated using a Cox proportional model stratified by sex and comorbidity score. There were 4,277 deaths (2,356 among women; 1,921 among men) during a median follow-up time of 7.12 y for women and 6.07 y for men. Among both women and men, sleep duration showed a J-shaped association with total mortality. Hazard ratios (95% confidence intervals) were 1.15 (1.01–1.32), 1.06 (0.94–1.20), 1.17 (1.04–1.32), 1.36 (1.13–1.64), and 2.11 (1.77–2.52) for women and 1.06 (0.90–1.25), 1.07 (0.94–1.23), 1.13 (1.00–1.28), 1.34 (1.10–1.62), and 1.55 (1.29–1.86) for men who slept 4–5, 6, 8, 9, and ≥ 10 h per day, respectively, compared with those who slept 7 h per day. Associations for disease-specific mortality, including cardiovascular disease, stroke, diabetes, and cancer, also generally followed the same J-shaped pattern. The sleep duration-mortality association was more evident among participants with comorbidities, but varied little by sex.
Conclusion:
In our study population of Chinese adults, shorter and longer sleep durations were independently associated with increased risk of mortality. But longer sleep duration had a higher mortality risk of cardiovascular disease and diabetes than short sleep.
Citation:
Cai H, Shu XO, Xiang YB, Yang G, Li H, Ji BT, Gao J, Gao YT, Zheng W. Sleep duration and mortality: a prospective study of 113,138 middle-aged and elderly Chinese men and women. SLEEP 2015;38(4):529–536.
Keywords: association, sleep duration, mortality
INTRODUCTION
Accumulating evidence suggests that quantity of sleep is an important factor associated with health and mortality.1 Deviations from 7–8 h of sleep per day have been associated with increased total mortality with a U-shaped association in several longitudinal studies.1–5 In a cohort study of 98,634 individuals in Japan, sleep duration showed a U-shaped association with increased total mortality with a nadir at 7 h of sleep.6 A recent meta-analysis found that the risk ratio associated with shorter sleep duration (e.g., < 7 h/day) was 1.12 (1.06–1.18, 95% confidence interval [CI]), whereas that associated with longer sleep duration (> 8 h/day) was 1.30 (1.22–1.38, 95% CI) compared with 7–8 h per day.3 However, a large study reported recently that mortality risk does not significantly vary according to sleep duration after prospectively controlling for baseline health and concluded that previous findings suggesting a relationship between sleep duration and mortality could be affected by residual confounding by poor preexisting health.7
Sleep duration is not only a habit people can freely choose but one that can be influenced by physical, mental, and other social conditions.8–10 Thus, the relation of sleep with total mortality and disease-specific mortality is complex. In this study, we used the data from two population-based cohort studies of Chinese adults, the Shanghai Women's Health Study (SWHS) and the Shanghai Men's Health Study (SMHS). We examined the associations of sleep duration on total mortality and disease-specific mortality and evaluated the influence of sex, comorbidities, history of night-shift work, and participation in regular exercise on the associations of sleep duration with mortality.
METHODS
Participants
The SWHS and the SMHS are population-based prospective studies involving 74,941 Chinese women aged 40 to 70 y and 61,480 men aged 40 to 74 y living in Shanghai, China. Details on the study design, methods, and questionnaires used in the baseline surveys have been previously described.11,12 Briefly, study enrollment for the SWHS took place between 1997 and 2000 with an overall response rate of 92.3%. Enrollment for the SMHS took place between 2002 and 2006 with an overall response rate of 75%. In-person follow-up surveys of all living SWHS cohort members were conducted from 2000 to 2002, 2002 to 2004, 2004 to 2006, and 2007 to 2012 with response rates of 99.8%, 98.7%, 95.0%, and 91.9%, respectively. Similar follow-up surveys of all living SMHS cohort members were conducted from 2004 to 2008 and from 2007 to 2011 with response rates of 97.7% and 91.9%, respectively. Both studies were approved by the relevant institutional review boards for human research at the Shanghai Cancer Institute (China) and Vanderbilt University (United States), and written informed consent was obtained from all participants.
Data Collection
The SWHS and SMHS used identical study protocols and nearly identical structured questionnaires at baseline to collect information on socioeconomic status, occupation, living conditions, personal history of chronic disease, physical activity level, family history disease, use of supplements (including vitamins and calcium), and usual dietary habits. Anthropometric measurements, including height, weight, and circumferences of waist and hips, were taken by trained interviewers. Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters, and waist-to-hip ratio (WHR) was calculated as waist circumference divided by hip circumference. The follow-up surveys collected information on occurrence of cancer and other chronic diseases, as well as survival status. Information on dietary intakes, physical activity, and other lifestyle factors were updated during follow-up.
Sleep related questions were asked during the third follow-up (approximately 4 y after enrollment) for the SWHS and during the baseline survey (at enrollment) for the SMHS. Information on sleep duration was collected based on the following question: “In the past 2 y for women (past 1 y for men), how many hours did you sleep each day (including sleeping during the day and night, but not including time if you woke up between two periods of sleep)?”. Participants reported sleep in 1-h increments and sleep duration referred to total hours of sleep per day. Information on history of night-shift work, defined as starting work after 22:00 at least 3 times per month for 1 y or longer, was collected at the second follow-up for the SWHS and at baseline for the SMHS. Among the 131,254 participants who completed the third follow-up survey for the SWHS or baseline survey for the SMHS, we excluded 17,731 participants who were missing sleep information (942 women, 16,775 men) or who were lost to follow-up (14 men). We also excluded 385 people who reported a sleep duration of less than 4 h or more than 15 h per day. The remaining 113,138 participants were included in the current study.
Total Mortality and Disease-Specific Mortality
Deaths were identified through a combination of active follow-up and record linkage with the Shanghai Vital Statistics Registry. The current analysis used mortality data updated through December 31, 2010. Underlying causes of death were coded according to the International Classification of Diseases, Ninth Revision13 and included: cardiovascular disease (CVD) (codes 390–459), stroke (codes 430–438), diabetes (code 250), cancer (codes 140–208; 150 and 151 for upper gastrointestinal cancer (UGI), 153 and 154 for colorectal cancer (CRC), 162 for lung cancer, and 174 for female breast cancer). Remaining codes were lumped together under the category “other causes of death”. Because information on sleep duration was not collected until the third follow-up survey for the SWHS, only deaths occurring after the third follow-up were included in this study.
Statistical Analyses
Sleep duration was divided into six categories: 4–5 h, 6 h, 7 h, 8 h, 9 h, and ≥ 10 h. Analysis of variance was used for comparing continuous variables, and the chi-square test was used for comparing dichotomous variables across the different sleep duration groups. Hazard ratios (HRs) for shorter or longer sleep durations and their 95% CIs were calculated by using Cox regression models adjusted for potential confounders, using the 7-h sleep group as the reference, because this group had the lowest mortality rates in both a previous study14 and the current study. Covariates adjusted for in the model included age at interview and selected demographic factors, including lifestyle factors, health status, and anthropometric measurements. Educational attainment level was divided into four categories: primary school or under, middle school, high school, and college or above. Personal income was divided into three categories: < 5,000, 5,000–10,000, and > 10,000 yuan/y for both the SWHS and the SMHS. Smoking status was divided into two categories (ever/never) for the SWHS and four categories (never, ex-smoker, current smoker [≤ 22.85 and > 22.85 pack/y]) for the SMHS. Alcohol consumption had two categories (ever/never) for the SWHS and five categories (0, 0.01–1.10, 1.11–1.84, 1.85–3.52, and > 3.52 drink/day) for the SMHS. Participation in regular exercise (“regular exercise” was defined as at least once per week for 3 mo or more) was categorized into five groups of 0, 0.01–0.97, 0.98–1.98, 1.99–3.83, and ≥ 3.84 metabolic equivalent (MET)-h/day for men and 0, 0.01–1.98, 1.99–3.77, 3.78–4.47, and ≥ 4.48 MET-h/day for women. Other dichotomous variables were created for self-reported history of night-shift work (yes/no), and tea consumption (ever/never). History of chronic disease was assessed using the Charlson comorbidity index (0, 1, 2, and ≥ 3).15
A restricted cubic spline function was used to calculate P values for curve trend tests. Similar models were applied for analyzing all-cause deaths, six specific causes of death, and deaths from all other causes. All tests were two-tailed with a significance level of P < 0.05. All analyses were performed using SAS statistical software (version 9.3; SAS Institute Inc., Cary, NC).
RESULTS
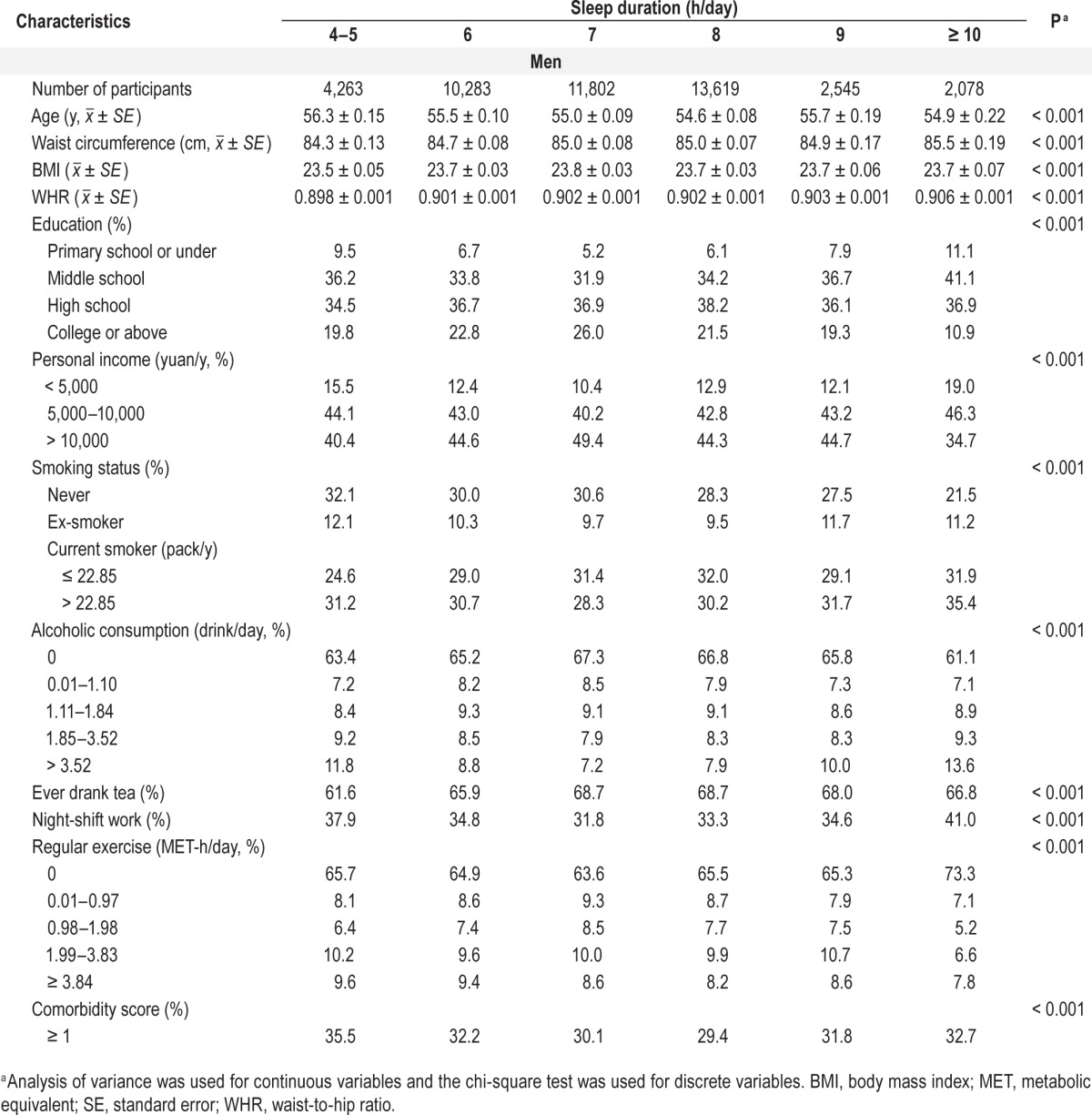
Tables 1A and 1B present associations between sleep duration and selected demographic characteristics, lifestyle factors, and anthropometric measurements for all study participants. The most frequent sleep duration was 8 h among both women and men. Sleep duration decreased with age, but increased with waist circumference, BMI, and WHR. For both sexes, those who had shorter and longer sleep durations were less educated, less likely to drink tea, and more likely to drink alcohol; in addition, they were more likely to have had a night-shift job, to have low income, and to have high comorbidity scores compared with participants in the 7 h/day and 8 h/day groups. Among women, exercise rates were inversely associated with sleep duration. Among men, exercise rates were comparable across all sleep duration groups, except among men in the ≥ 10 h/day group, whose exercise rates were lower.
Table 1A.
Associations between age at interview, lifestyle factors, and anthropometric measurements among women in Shanghai, China.
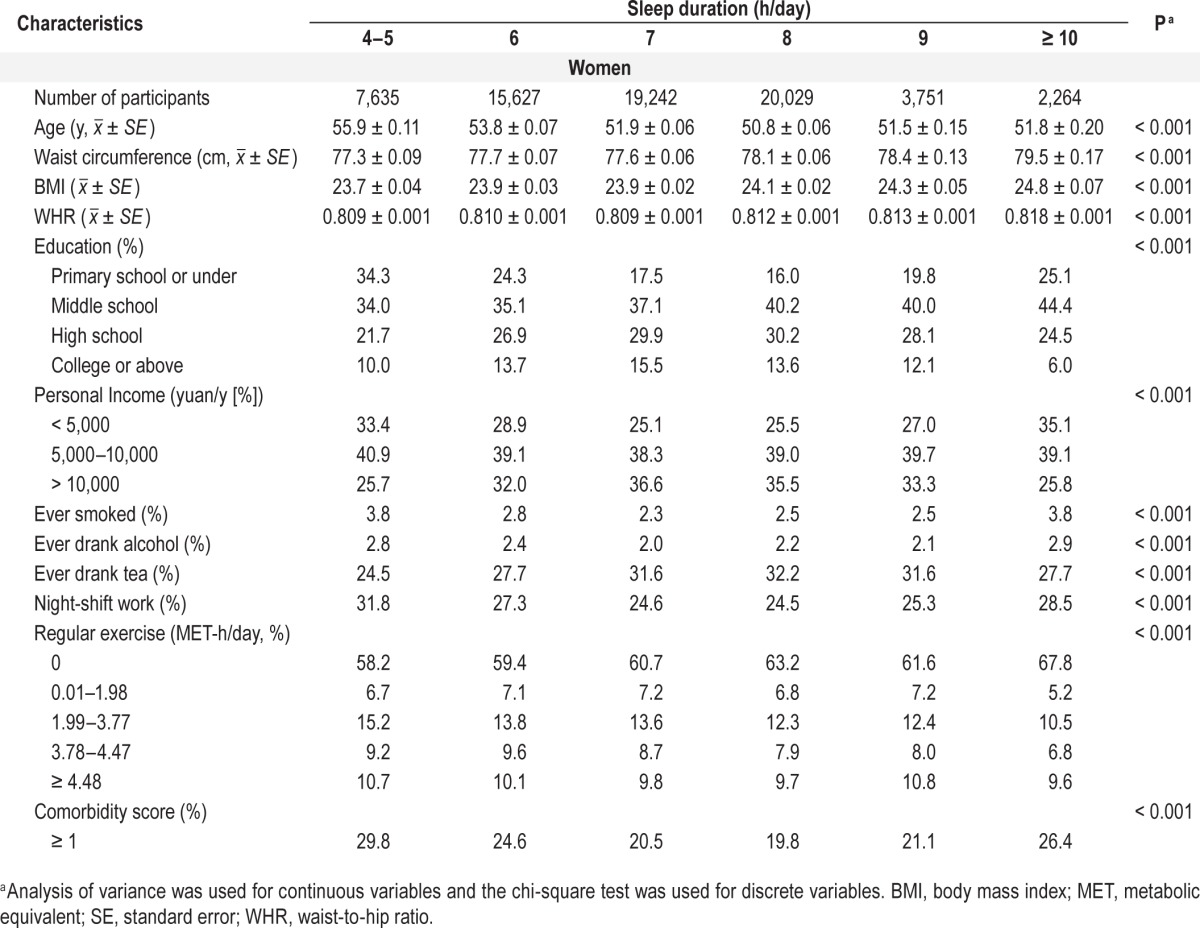
Table 1B.
Associations between age at interview, lifestyle factors, and anthropometric measurements among men in Shanghai, China.
A total of 4,277 deaths (2,356 women, 1,921 men) had occurred as of the end of 2010. As shown in Table 2, a sleep duration of 4–5 h/day was associated with a modestly elevated HR for total mortality (HR = 1.15 and 1.06 for women and men, respectively), compared with the 7 h/day group. Longer sleep durations were associated with significantly increased risk of total mortality. Among women, HRs were 1.17 (1.04–1.32) for the 8 h/day group, 1.36 (1.13–1.64) for the 9 h/day group, and 2.11 (1.77–2.52) for the ≥ 10 h/day group. Among men, HRs were 1.13 (1.00–1.28), 1.34 (1.10–1.62), and 1.55 (1.29–1.86) for the 8, 9, and ≥ 10 h/day groups, respectively. For both women and men, a J-shaped association was observed between sleep duration and total mortality (Figure 1). This J-shaped association was also observed for several major causes of death, including CVD, stroke, diabetes, and cancer. Among women, HRs for the ≥ 10 h/day group were 2.64 (1.99–3.52) for CVD, 3.09 (2.14–4.47) for stroke, 3.73 (1.98–7.05) for diabetes, and 1.47 (1.08–2.00) for all cancers combined compared with women in the 7 h/day group. These non-linear associations were all statistically significant (P < 0.01). Among men, we found no nonlinear associations between sleep duration and disease-specific mortality.
Table 2.
Associations of sleep duration with overall and disease-specific mortality among women and men in Shanghai, China.
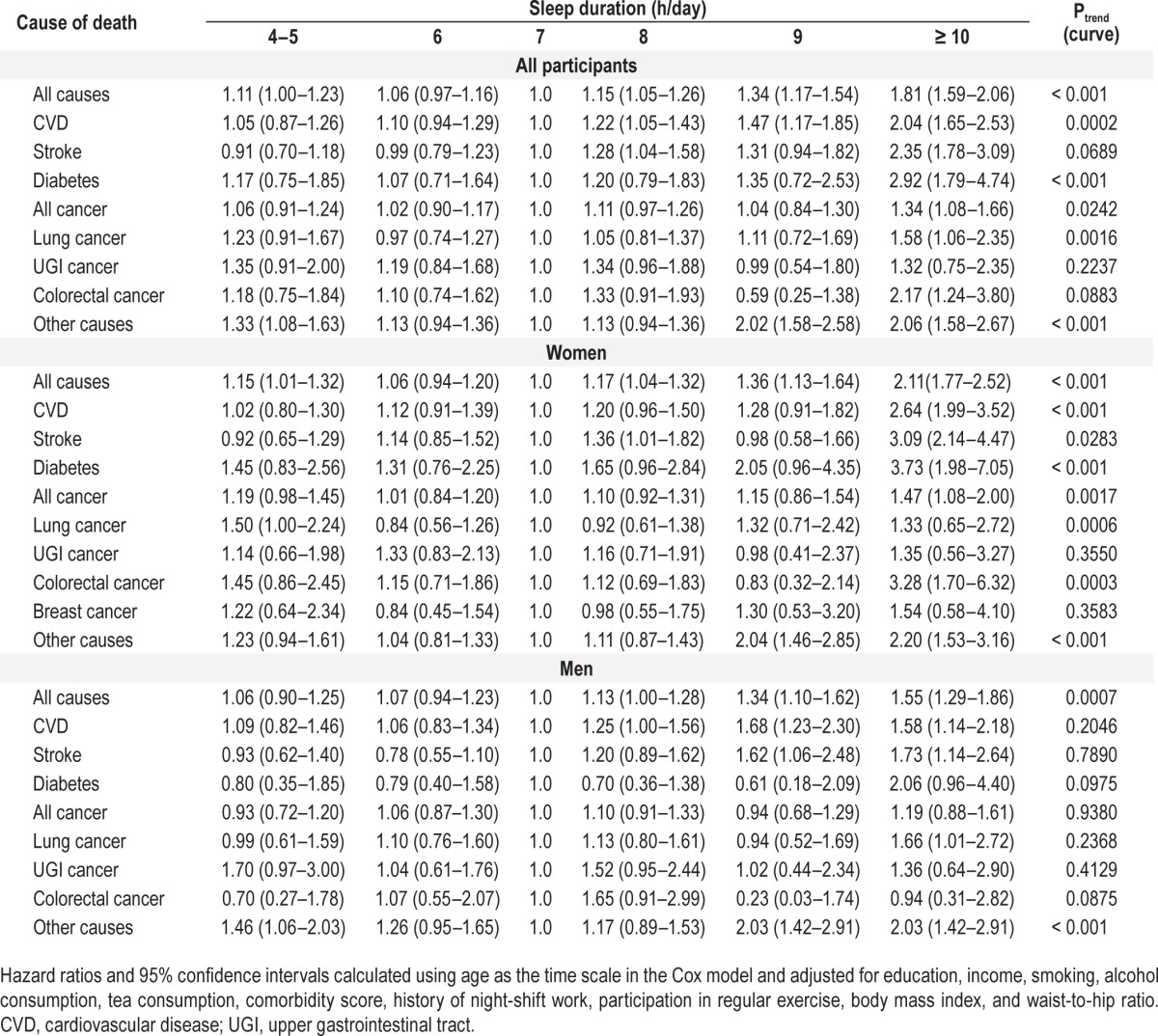
Figure 1.
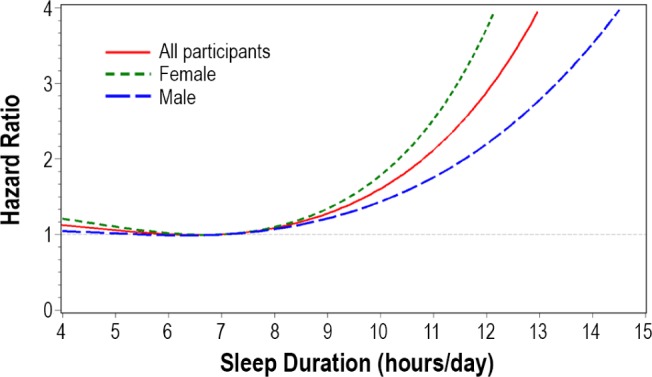
Association between overall survival and hours of sleep. There are J-shaped associations of overall survival and hours of sleep among both Chinese men and women using the 7 h/day group as a reference.
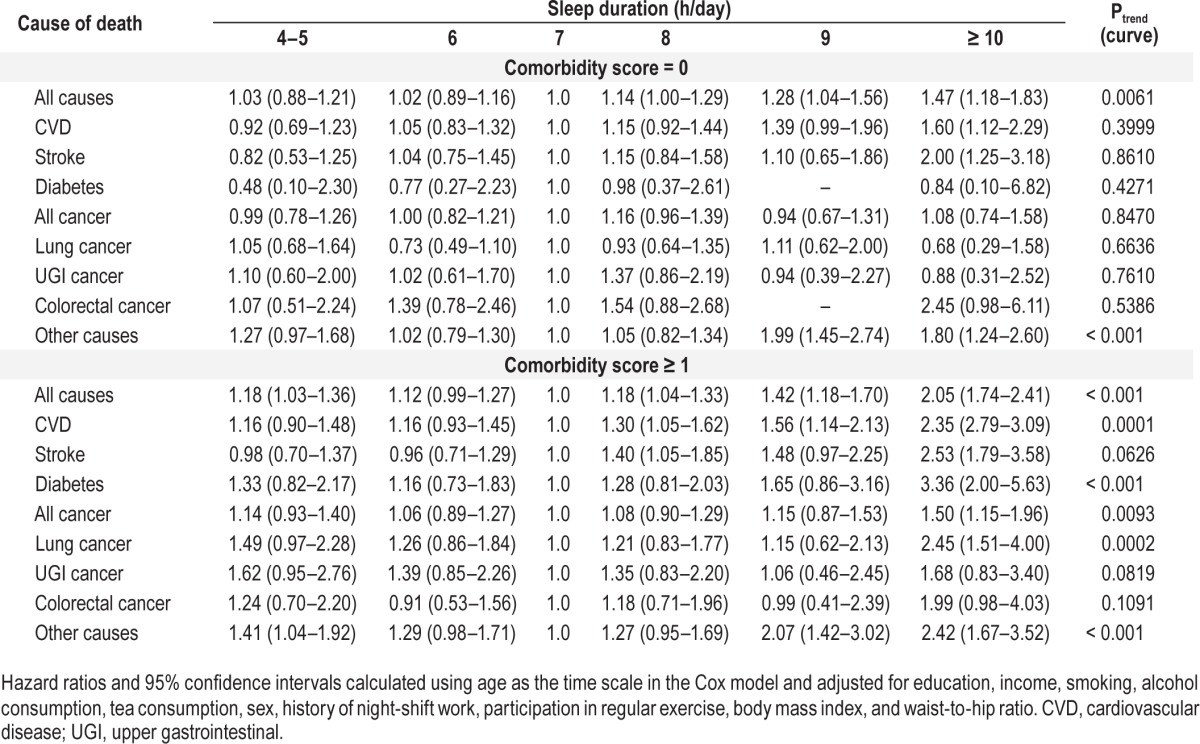
Table 3 presents associations between sleep duration and total mortality and disease-specific mortality stratified by comorbidity for all participants combined. As expected, the sleep duration and mortality association was evident among individuals with at least one comorbidity (score ≥ 1). Compared with the 7 h/day group, HRs for the ≥ 10 h/day group were 1.5–3.4 times higher with a statistically significant J-shaped trend for major causes of death, including CVD, stroke, diabetes, and cancer. However, among participants in the ≥ 10 h/day group with no comorbidities, higher mortality risk was observed only for CVD (HR = 1.60) and stroke (HR = 2.00). We analyzed associations of sleep duration with history of night-shift work and regular exercise participation for all participants combined. HRs for total mortality and disease-specific mortality were comparable among participants regardless of whether they reported a history of night-shift work or participation in regular exercise (data not presented). We also did a sensitivity analysis excluding those deceased individuals with follow-up duration < 2 y to avoid that disease status might have affected sleep patterns and got similar results (data not shown).
Table 3.
Associations of sleep duration with total mortality and disease-specific mortality by comorbidity score.
DISCUSSION
In this large, population-based cohort study of Chinese adults from Shanghai, we found that compared with a sleep duration of 7 h/day, both shorter (≤ 5 h/day) and longer (≥ 9 h/day) sleep durations were associated with increased total mortality and mortality from CVD, stroke, diabetes, cancer, and other diseases. These associations appeared to be independent of major confounders, and the magnitude of the associations appeared to be stronger for longer sleep durations than for shorter sleep durations, yielding a J-shaped relationship. These J-shaped associations were more evident among individuals with comorbidities and did not appear to be modified by history of night-shift work or regular exercise participation.
Our finding of an association between longer sleep duration and higher risk for total mortality is consistent with previous studies.16–18 A study in Great Britain found that those who sleep longer were at increased risk of mortality after 23 y of follow-up.19 A study of over 1 million American adults (aged 30–102 y) showed similar findings that were consistent across age and sex; sleep durations below 6.5 h/day and above 7.5 h/ day were associated with increasing risk for total mortality but mostly with longer sleep duration (≥ 7.5 h/day).17 Similar to our study, a Japanese study involving 104,010 participants (aged 40–79 y) found a J-shaped association between sleep and mortality among men. Specifically, sleep durations of more or less than 7 h were associated with increased mortality risk after an average of 10 y of follow-up.14 A recent study conducted in Brazil also reported a J-shaped association between sleep duration and total mortality.20
The biological mechanism driving this association is not completely understood. It has been postulated that worsening physical condition may be associated with both longer sleep duration and mortality.14 Magee et al.7 concluded that a previous finding suggesting a relationship between sleep duration and mortality could be affected by residual confounding by poor preexisting health because in their study they found that total mortality risk does not significantly vary according to sleep duration after prospective controlling for baseline health. However, in our study, we found that longer sleep durations were still associated with total mortality and CVD and stroke mortality even after excluding individuals with major comorbidities, including diabetes, myocardial infarction, cerebrovascular disease, and cancers diagnosed before the sleep assessment. A possible explanation is that the effect of residual confounding on the association could be reduced because we had a median follow-up time of 7.12 y for women and 6.07 y for men. The association between sleep duration and total mortality are consistent by health status (P for interaction = 0.061) in our study. Similarly, longer sleep duration was found to be associated with higher mortality among older adults with good health status in a Spanish population.21 Thus, the association between long sleep duration and total mortality cannot be completely explained by comorbidities or by the physical condition of individuals. It is likely that poor quality of sleep, such as sleep fragmentation, waking after sleep onset, sleep latency, and feelings of fatigue and lethargy after a long sleep, may induce sleep extension22–24 and decrease resistance to disease, which, in turn, may lead to increased mortality.25 Unfortunately, we were not able to investigate this mechanism because of a lack of relevant information. In our study, sleep duration was positively associated with BMI, WHR, and waist circumference, known risk factors for diabetes, CVD, and stroke. Thus, obesity may mediate the association between longer sleep duration and total or disease-specific mortality.
Consistent with prior studies, the increased risk of mortality among our participants with longer sleep durations did not appear to be limited to one cause of death.6,26 We observed similar patterns for various disease-specific mortalities. Among them, CVD mortality is a very interesting topic in sleep duration studies. An early National Health and Nutrition Examination Survey (NHANES)-I study reported that longer sleep duration was independently associated with CVD during a 10-y follow-up.27 Subsequent studies have confirmed this finding among elderly people, women, and other populations.28–31 A recent meta-analysis by Cappuccio et al.32 also found that long sleep duration was associated with a greater risk of CVD (relative risk [RR] = 1.41, 95% CI: 1.19–1.68) and stroke (RR = 1.65, 95% CI: 1.45–1.87) with no evidence of publication bias and suggested that long sleep duration is a predictor or marker of cardiovascular outcomes. It could be argued that an observed association between longer sleep duration and CVD mortality may be caused by underlying disease that caused subjects to sleep more, i.e., an increased need for sleep plus reduced physiologic reserve resulted in reduced ability to survive the underlying serious illness.28 A large epidemiologic study found that longer sleep durations are associated with snoring and with metabolic disturbances, including insulin resistance, abnormal lipid profile, and elevated markers of increased cortisol levels and abnormal growth hormone secretion.33 In our study, an association between longer sleep duration and CVD/ stroke mortality was also observed among participants with no comorbidities, although the association was weaker than that observed among participants with comorbidities (HR = 2.35 for CVD and HR = 2.53 for stroke, P < 0.01), suggesting that underlying disease may be partially responsible for the observed associations with sleep duration. However, a recent review examined the underlying mechanisms of association between sleep deprivation and CVD and considered that levels of markers of obesity and appetite control, energy metabolism, glucose homoeostasis, inflammation, thrombosis, and hemostasis, which are affected by short sleep duration, might be useful predictors of the risk of developing CVD,34 suggesting several possible biological mechanisms linking sleep duration and mortality.
There has been increasing interest in possible associations between sleep disorders and the prevalence/incidence of glucose metabolism disorders and diabetes. Several retrospective35 and prospective36 studies have shown a relationship between sleep duration and type 2 diabetes mellitus. A literature review by Alvarez and Ayas37 indicated that longer sleep duration is a moderate risk factor for development of diabetes. A recent US cohort study found that sleep disorders are an independent predictor of diabetes, although the association disappeared after additional adjustment for physical health.38 We found that sleep duration was associated with diabetes mortality after adjustment for comorbidities and BMI. Although less well supported, it is possible that longer sleep duration may cause inflammation, because it has been associated with increased sleep fragmentation and more frequent awakenings, which can influence cytokine expression and risk of diabetes.26,39 In the only study of sleep duration and inflammation conducted in a non-Western population, a strong positive relationship was found between longer sleep duration and several markers of inflammation (e.g. C-reactive protein, interleukin-6, and fibrinogen), among Chinese adults with an average age of 66.1 y (standard deviation = 10.4 y).39 Cappuccio et al. reported that the mechanisms underlying association between habitual sleep disturbances and diabetes may be different: low-grade inflammation and reduced acute insulin response to glucose are activated during short sleep duration, thus predisposing individuals to type 2 diabetes. However, there is a less clear indication of possible mechanisms mediating the effect of long sleep duration as a cause of type 2 diabetes.40
Association between sleep duration and mortality varies by sex. Meisinger et al. reported that a modest association between short sleep and incident myocardial infarction was observed in middle-aged women but not men in the MONICA (Monitoring trends and determinants on cardiovascular diseases) study.41 In our study, sex differences were observed in association of sleep duration and total mortality and disease-specific mortality although these associations had similar patterns. Ideally, longer follow-up would be appropriate to assess the influence of sleep duration on mortality over the life course,5 especially for the SMHS. Night-shift work is a common cause of insomnia and reduced sleep time, because it causes individuals to try to sleep at times that are less than ideal because of both circadian influences and environmental cues. In addition, night-shift work may have adverse health consequences, including heart disease and breast cancer.42,43 In our previous study, history of night-shift work was associated with both shorter and longer sleep durations.8 In analyses stratified by history of night-shift work, we found that ever having held a night-shift job did not modify the association of sleep duration with total mortality or with mortality from CVD, stroke, or other causes.
A meta-analysis, including over two million people from 23 prospective studies, reported that the risk of total mortality was increased by 10–12% among those with shorter sleep durations and 23–30% among those with longer sleep durations, yielding a U-shaped relationship.1 In our study the risk of total mortality was increased 11% among those with shorter sleep durations, which is consistent with the results of the meta-analysis. However, total mortality risk was increased 81% among those with longer sleep durations, which resulted in a J-shaped association between sleep duration and total mortality in our Chinese population.
The advantages of our study include its large sample size, the population-based design, and our ability to adjust for a wide range of lifestyle factors and health conditions. Some limitations of the data need to be discussed. First, sleep duration was derived from a self-reported questionnaire item without investigating questionnaire reliability or objective sleep patterns, which may also have introduced bias. Lauderdale and colleagues44 reported a moderate correlation between self-reported sleep duration and actigraph measures of sleep duration of 0.47. Second, we did not collect data of sleep quality, sleep disturbances, depression, self-rated health and use of hypnotics at the survey, which may provide more information to understand the association between sleep duration and mortality. Third, as many large cohort studies do, we used a single item to assess sleep duration and assumed that sleep patterns were consistent over the preceding 1–2 y, which could lead to biased estimation because sleep duration could be changed along with changes of working and living environment and health conditions. Therefore, further research should assess association of repeated measures of sleep duration and mortality. Last, like most observational studies, we were unable to determine causality for the sleep-mortality associations.
CLINICAL SIGNIFICANCE AND CONCLUSION
Our study found that sleep duration is a good predictor of total mortality and several disease-specific mortalities among middle-aged and elderly Chinese women and men. Because information on sleep duration is easy to obtain, it may serve as a useful tool for the identification of high-risk populations in clinical practice for possible intervention.
DISCLOSURE STATEMENT
This was not an industry supported study. The study was supported by grants (R37 CA070867 to Wei Zheng and R01 CA082729 and UM1 CA173640 to Xiao-Ou Shu) from the US National Institutes of Health and the Intramural Research Program of the National Institutes of Health, National Cancer Institute. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the participants and staff members of the SMHS and the SWHS for their important contributions and Ms. Bethanie Rammer and Mrs. Stern Jacqueline for editing and preparing the manuscript.
REFERENCES
- 1.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18:148–58. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 2.Hublin C, Partinen M, Koskenvuo M, Kaprio J. Sleep and mortality: a population-based 22-year follow-up study. Sleep. 2007;30:1245–53. doi: 10.1093/sleep/30.10.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–92. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferrie JE, Shipley MJ, Cappuccio FP, et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007;30:1659–66. doi: 10.1093/sleep/30.12.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Sleep duration associated with mortality in elderly, but not middle-aged, adults in a large US sample. Sleep. 2008;31:1087–96. [PMC free article] [PubMed] [Google Scholar]
- 6.Ikehara S, Iso H, Date C, et al. Association of sleep duration with mortality from cardiovascular disease and other causes for Japanese men and women: the JACC study. Sleep. 2009;32:295–301. doi: 10.1093/sleep/32.3.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Magee CA, Holliday EG, Attia J, Kritharides L, Banks E. Investigation of the relationship between sleep duration, all-cause mortality, and preexisting disease. Sleep Med. 2013;14:591–6. doi: 10.1016/j.sleep.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 8.Tu X, Cai H, Gao YT, et al. Sleep duration and its correlates in middle-aged and elderly Chinese women: the Shanghai Women's Health Study. Sleep Med. 2012;13:1138–45. doi: 10.1016/j.sleep.2012.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gialason T, Almqvist M. Somatic diseases and sleep complaints. An epidemiological study of 3,201 Swedish men. Acta Med Scand. 1987;221:475–81. [PubMed] [Google Scholar]
- 10.Barbar SI, Enright PL, Boyle P, et al. Sleep disturbances and their correlates in elderly Japanese American men residing in Hawaii. J Gerontol A Biol Sci Med Sci. 2000;55:M406–11. doi: 10.1093/gerona/55.7.m406. [DOI] [PubMed] [Google Scholar]
- 11.Cai H, Zheng W, Xiang YB, et al. Dietary patterns and their correlates among middle-aged and elderly Chinese men: a report from the Shanghai Men's Health Study. Br J Nutr. 2007;98:1006–13. doi: 10.1017/S0007114507750900. [DOI] [PubMed] [Google Scholar]
- 12.Zheng W, Chow WH, Yang G, et al. The Shanghai Women's Health Study: rationale, study design, and baseline characteristics. Am J Epidemiol. 2005;162:1123–31. doi: 10.1093/aje/kwi322. [DOI] [PubMed] [Google Scholar]
- 13.National Cancer Institute. Surveillance, Epidemiology, and End Results Program. [Accessed February 20, 2014]. http://seer.cancer.gov/tools/conversion/
- 14.Tamakoshi A, Ohno Y. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep. 2004;27:51–4. [PubMed] [Google Scholar]
- 15.Grunau GL, Sheps S, Goldner EM, Ratner PA. Specific comorbidity risk adjustment was a better predictor of 5-year acute myocardial infarction mortality than general methods. J Clin Epidemiol. 2006;59:274–80. doi: 10.1016/j.jclinepi.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 16.Kojima M, Wakai K, Kawamura T, et al. sleep patterns and total mortality: a 12-year follow-up study in Japan. J Epidemiol. 2000;10:87–93. doi: 10.2188/jea.10.87. [DOI] [PubMed] [Google Scholar]
- 17.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 18.Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: a 12-year follow-up study of a middle-aged Swedish population. J Intern Med. 2002;251:207–16. doi: 10.1046/j.1365-2796.2002.00941.x. [DOI] [PubMed] [Google Scholar]
- 19.Gale C, Martyn C. Larks and owls and health, wealth, and wisdom. BMJ. 1998;317:1675–77. doi: 10.1136/bmj.317.7174.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Castro-Costa E, Dewey ME, Ferri CP, et al. Association between sleep duration and all-cause mortality in old age: 9-year follow-up of the Bambui Cohort Study, Brazil. J Sleep Res. 2011;20:303–10. doi: 10.1111/j.1365-2869.2010.00884.x. [DOI] [PubMed] [Google Scholar]
- 21.Mesas AE, Lopez-Garcia E, Leon-Munoz LM, Guallar-Castillon P, Rodriguez-Artalejo F. Sleep duration and mortality according to health status in older adults. J Am Geriatr Soc. 2010;58:1870–7. doi: 10.1111/j.1532-5415.2010.03071.x. [DOI] [PubMed] [Google Scholar]
- 22.Youngstedt SD, Kripke DF. Long sleep and mortality: rationale for sleep restriction. Sleep Med Rev. 2004;8:159–74. doi: 10.1016/j.smrv.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 23.Grandner MA, Kripke DF. Self-reported sleep complaints with long and short sleep: a nationally representative sample. Psychosom Med. 2004;66:239–41. doi: 10.1097/01.psy.0000107881.53228.4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taub JM, Berger RJ. Performance and mood following variations in the length and timing of sleep. Psychopharmacology (Berl) 1973;10:559–70. doi: 10.1111/j.1469-8986.1973.tb00805.x. [DOI] [PubMed] [Google Scholar]
- 25.Dantzer R. Cytokine-induced sickness behavior: mechanisms and implications. Ann N Y Acad Sci. 2001;933:222–34. doi: 10.1111/j.1749-6632.2001.tb05827.x. [DOI] [PubMed] [Google Scholar]
- 26.Grandner MA, Drummond SP. Who are the long sleepers? Towards an understanding of the mortality relationship. Sleep Med Rev. 2007;11:341–60. doi: 10.1016/j.smrv.2007.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Qureshi AI, Giles WH, Croft JB, Bliwise DL. Habitual sleep patterns and risk for stroke and coronary heart disease: a 10-year follow-up from NHANES I. Neurology. 1997;48:904–11. doi: 10.1212/wnl.48.4.904. [DOI] [PubMed] [Google Scholar]
- 28.Patel SR, Ayas NT, Malhotra MR, et al. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27:440–4. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
- 29.Lan TY, Lan TH, Wen CP, Lin YH, Chuang YL. Nighttime sleep, chinese afternoon nap, and mortality in the elderly. Sleep. 2007;30:1105–10. doi: 10.1093/sleep/30.9.1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Suzuki E, Yorifuji T, Ueshima K, et al. Sleep duration, sleep quality and cardiovascular disease mortality among the elderly: a population-based cohort study. Prev Med. 2009;49:135–41. doi: 10.1016/j.ypmed.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 31.Chien KL, Chen PC, Hsu HC, et al. Habitual sleep duration and insomnia and risk of cardiovascular events and all-cause death: report from a community-based cohort. Sleep. 2010;33:177–84. doi: 10.1093/sleep/33.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32:1484–92. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 33.Williams CJ, Hu FB, Patel SR, Mantzoros CS. Sleep duration and snoring in relation to biomarkers of cardiovascular disease risk among women with type 2 diabetes. Diabetes Care. 2007;50:1233–40. doi: 10.2337/dc06-2107. [DOI] [PubMed] [Google Scholar]
- 34.Miller MA, Cappuccio FP. Biomarkers of cardiovascular risk in sleep-deprived people. J Hum Hypertens. 2013;27:583–8. doi: 10.1038/jhh.2013.27. [DOI] [PubMed] [Google Scholar]
- 35.Punjabi NM, Shahar E, Redline S, et al. Sleep-disorders breathing, glucose intolerance and insulin resistance. Am J Epidemiol. 2004;160:521–30. doi: 10.1093/aje/kwh261. [DOI] [PubMed] [Google Scholar]
- 36.Al-Delaimy WK, Manson JE, Willett WC, Stampfer MJ, Hu FB. Snoring as a risk factor for type II diabetes mellitus: a prospective study. Am J Epidemiol. 2002;155:387–93. doi: 10.1093/aje/155.5.387. [DOI] [PubMed] [Google Scholar]
- 37.Alvarez GG, Ayas NT. The impact of daily sleep duration on health: a review of the literature. Prog Cardiovasc Nurs. 2004;19:56–9. doi: 10.1111/j.0889-7204.2004.02422.x. [DOI] [PubMed] [Google Scholar]
- 38.Grandner MA, Jackson NJ, Pak VM, Gehrman PR. Sleep disturbance is associated with cardiovascular and metabolic disorders. J Sleep Res. 2012;21:427–33. doi: 10.1111/j.1365-2869.2011.00990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dowd JB, Goldman N, Weinstein M. Sleep duration, sleep quality, and biomarkers of inflammation in a Taiwanese population. Ann Epidemiol. 2011;21:799–806. doi: 10.1016/j.annepidem.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes. Diabetes Care. 2010;33:414–20. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meisinger C, Heier M, Lowel H, Schneider A, Doring A. Sleep duration and sleep complaints and risk of myocardial infarction in middle-aged men and women from the general population: the MONICA/KORA Augsburg cohort study. Sleep. 2007;30:1121–7. doi: 10.1093/sleep/30.9.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schernhammer ES, Razavi P, Li TY, Qureshi AA, Han J. rotating night shifts and risk of skin cancer in the nurses' health study. J Natl Cancer Inst. 2011;103:602–6. doi: 10.1093/jnci/djr044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hansen J, Stevens RG. Case-control study of shift-work and breast cancer risk in Danish nurses: impact of shift systems. Eur J Cancer. 2012;48:1722–9. doi: 10.1016/j.ejca.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 44.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;196:838–45. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]


