Abstract
Background:
The best treatment for scaphoid nonunion fractures is still controversial. The main aim of this study was to determine the results of the modified Matti-Russe method of surgery on scaphoid nonunion.
Materials and Methods:
In this prospective interventional study, 30 patients with nonunion scaphoid fracture recruited from clinics of the Isfahan University of Medical Sciences between October 2007 and March 2011 underwent the modified Matti-Russe method of surgery. Union rate was evaluated four and six months after the procedure. Mayo wrist score (MWS) was calculated for the subjects six months after surgery.
Results:
Mean age of the subjects was 25.9 ± 7.8 years, ranging from 16 to 35 years. Twenty-seven (90%) were men, and three (10%) were women. Four and six months after surgery, 10 (33%) and 26 (86.7%) subjects had a united fracture. Mean MWS was 75.0 ± 8.8 in all the subjects, ranging from 54 to 90 six months after surgery. Three subjects (10%) were grouped as excellent, 9 (30%) good, 16 (53.3%) satisfactory, and 3 (6.7%) poor.
Conclusion:
A fracture or nonunion of the scaphoid bone can be a complex and troubling injury, but the modified Matti-Russe method showed satisfactory results six months after surgery.
Keywords: Matti-Russe, Mayo wrist score, scaphoid nonunion
INTRODUCTION
A scaphoid fracture is a fracture of the scaphoid bone and is the most common type of carpal bone fractures. It often occurs after a fall on the outstretched hand or in a motor vehicle accident, after hyperextension of the wrist joint, but any sufficiently strong force on the hand may break the wrist.[1,2] Patients usually present with pain, decrease in range of motion specifically in extension and radial deviation, and tenderness and swelling in the snuffbox. The fracture might show up in a poster anterior and semi-phonated X-ray view but it is not always the case. These patients often have to wear casts or splints and a second set of X-rays is taken about 7 to 10 days later.[3,4]
Delays in diagnosis and inadequate treatment of acute scaphoid fractures can lead to osteoarthritis, avascular necrosis, and nonunion. In subjects with fractures in the middle part of the bone (waist of scaphoid) or the proximal pole, healing is more difficult. These areas of the scaphoid do not have a very good blood supply. In fresh acute fractures less than four weeks old, a union rate of 95% can be achieved using common treatments.[3,5,6]
Despite the advent of new surgical methods, the rate of nonunion for scaphoid fractures remains as high as 10%. Scaphoid nonunion can present with or without avascular necrosis of the proximal pole and may show a humpback deformity on the radiograph. Scaphoid nonunion can progress to carpal collapse and degenerative arthritis, causing personal and economic costs, and decrease in the quality of life.[7,8]
Surgical treatment is directed at correcting the deformity with open reduction and internal fixation by placing a screw in the scaphoid together with bone grafting. There are different types of bone graft, including nonvascular zed and vascularized bone grafts (blood vessels of the patients themselves) that have recently gained popularity in the treatment of scaphoid nonunion, particularly in cases with avascular necrosis.[2,9,10]
In one study, in patients undergoing three different surgical methods including the Herbert screw fixation, the Matti-Russe bone grafting, or the Kohlman modification of vascularized muscle pedicle graft procedure, there was no significant difference between the union rate in the three methods, but time to union was earliest in the Kohlman modification of vascularized muscle pedicle graft procedure.[1]
One study showed that internal fixation of the scaphoid using the Herbert bone screw, although technically demanding, has fewer complications and appears to offer significant advantages over other methods of treatment.[11] Three other studies evaluated the Matti-Russe method, and it proved to be a satisfactory method for the treatment of long-standing or neglected scaphoid nonunion, showing high percentages of healing and functional improvement.[7,12,13,14]
The Matti-Russe method is an established well-accepted method which is simple and inexpensive for the treatment of scaphoid surgery presented by Hermann Matt in 1937 and modified by Otto Russe in 1960. Satisfaction of the patient after this surgery is usually high.[15] In this study, we decided to evaluate the results of the Matti-Russe method of surgery on scaphoid nonunion fractures.
MATERIALS AND METHODS
In this prospective interventional study, a total of 30 patients with nonunion scaphoid fracture were included in the study. The subjects were recruited from clinics of the Isfahan University of Medical Sciences between October 2007 and March 2011. Written informed consent was obtained from all subjects prior to the study.
All subjects between the ages 15 and 50 years, who had a waist scaphoid fracture (fracture in the middle third of the scaphoid bone) during the six months before initiation of the study were included. Subjects with a history of systemic disorders affecting the musculoskeletal system, bone tumors, or bone infection were excluded. We also excluded subjects with a simultaneous fracture of other wrist bones, apparent degenerative changes in wrist bones, or radiologically proven scapholunate dissociation from the study.
We evaluated avascular necrosis in the proximal pole of the scaphoid bone by X-ray and magnetic resonance imaging (MRI) modalities. Overall, 30 patients underwent surgery with the modified Matti-Russe method after the initial examinations. In the modified Matti-Russe method, by adopting a palmar approach (which would be less likely to cause damage to the blood supply of the scaphoid), the proximal and distal parts of the bone were excavated by removing all the necrotic bone, cartilage, and fibrous tissue at the fracture site using a dental burr through a dorsal incision, and were replaced with a plug of corticocancellous graft; then, the mean proximal and distal parts of the fracture and the bone graft of these three parts were fixed using two pins inserted longitudinally in a parallel position. The corticocancellous graft was harvested from the iliac crest, and was then shaped to fit the excavated cavity better.[15] In our study, after assessing the fracture alignment with a C-arm three-dimensional imaging system, in case of instability, internal fixation with a pair of parallel K-wires was performed.
The union was considered to have occurred when there was no tenderness at the anatomical snuffbox and there was evidence of bony trabeculae crossing the fracture line or a sclerotic band present at the site of the fracture on at least three views. Mean time to radiological union for all fractures is nine weeks.[3,16] Thus, we evaluated the union in patients four and six months after surgery, to ensure that the surgery had its effect on the patient.
The patients were assessed based on the Mayo wrist Sscore (MWS) questionnaire on a follow-up after six months. The questionnaire consists of questions assessing pain intensity, functional status, range of motion, and grip strength. Scores are recorded in four groups: 90-100: Excellent, 80-90: Good, 60-80: Satisfactory, below 60: poor.
Pain was categorized in four levels of “No pain”, “Mild occasional”, “Moderate tolerable”, and “Severe to intolerable”. Physical activity was also categorized as “Returned to regular employment”, “Restricted employment”, and “Able to work but unemployed”. Range of motion in dorsiflexion, palmar flexion, radial flexion, and ulnar flexion in the affected wrist was measured using a goniometer, and was reported as a percentage. Grip strength was measured by asking the patient to squeeze the index finger of the examiner, and the strength was compared on the contralateral side using a dynamometer, and reported as a percentage.
Statistical analysis was performed using SPSS (version 18, Chicago, IL, USA). Data are expressed as mean ± standard deviation for numerical variables and as percent (%) for categorical variables. Independent t-test, paired t-test, and Chi-square were used to analyze the data.
RESULTS
A total of 30 patients with nonunion scaphoid fracture were evaluated in this study. Mean age of the subjects was 25.9 ± 7.8 years ranging from 16 to 35 years. Twenty-seven (90%) were men, and three (10%) were women. Mean age of the men and women was 25.6 ± 5.7 and 26.3 ± 6.5 years, respectively, with no significant differences.
According to MRI evaluation, 18 subjects (60%) suffered from proximal pole avascularity at submission. All of these 18 cases were men. However, Fisher's exact test did not show a statistically significant difference between men and women (P = 0.054). Mean age of the subjects who suffered from avascularity was not also significantly different from those who did not have proximal pole avascularity (P = 0.5).
Sixteen weeks after surgery [Table 1], fracture in 10 patients (33%) was united, and there were 20 cases of nonunion. Only two cases (11.1%) with avascularity had a united fracture, and union occurred in eight patients (66.7%) without avascularity. Union was more possible in subjects without avascularity, and the difference was statistically significant (P = 0.004). Mean age of the subjects was not statistically different between the union and nonunion groups.
Table 1.
Union rate four and six months after surgery according to avascularity
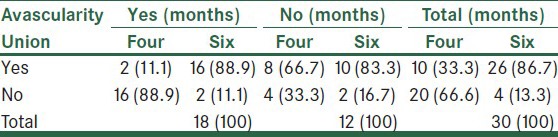
Six months after surgery [Table 1], 26 subjects (86.7%) had a united fracture, whereas four patients (13.3%) still suffered from nonunion. Two subjects, of the four nonunion cases, had a history of avascularity (11.1%), but the other two did not (16.7%). The difference was not significant. Mean age of the subjects with union six months after surgery was 26.0 ± 4.7 years, whereas in subjects with nonunion, it was 25.8 ± 2.9 years, and the difference was not statistically significant (P = 0.21).
MWS
Six months after surgery, mean MWS was 75.0 ± 8.8 in all the subjects, ranging from 54 to 90. Three subjects (10%) were grouped as excellent, 9 (30%) good, 16 (53.3%) satisfactory, and 3 (6.7%) poor [Figure 1].
Figure 1.
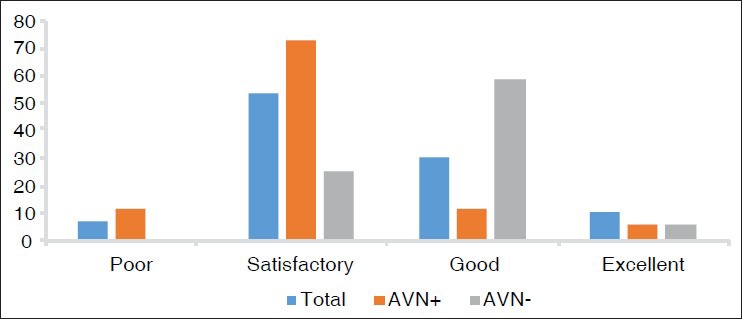
Mayo wrist score in subjects six months after surgery according to avascularity
Mean MWS was 73.3 ± 8.6 in subjects affected by proximal pole avascularity, and 75.9 ± 7.5 in subjects without avascularity, and the difference between these two groups was not statistically significant (P = 0.06).
Overall, 5.6% of subjects with avascularity had an excellent MWS, whereas this was 16.7% in subjects without avascularity. Again, 11.1% of the subjects in the avascularity group and 58.3% of those without avascularity had a good score, respectively, whereas in the satisfactory group, this value was 72.2% in the avascularity and 25% in the vascularity groups, and for the poor grade category, it was 11.1% for the avascularity group. Although the means of the two groups was not significantly different based on the student's t-test, according to Fisher's exact test, the difference was significant with a P value of 0.006.
DISCUSSION
In this study, we evaluated 30 patients with nonunion scaphoid fracture who underwent the modified Matti-Russe method for surgery after four and six months. The results were satisfactory based on the Mayo wrist score questionnaire.
In another study performed by Kolodziej et al., nonunion rate after the Matti-Russe surgery method was compared in patients with bone union and patients with persistent nonunion after a long-term follow-up of 2 to 27 years (mean: 8.8 years), and it was reported to be 28%. This is almost higher than in our study, with a nonunion rate of 13.3% after six months. This might be due to stabilization after undergoing the Matti-Russe method in our study. Grip strength and range of movement were similar in both groups. Better clinical outcome in patients with bone union was of course observed.[17]
In a study by Bullens et al., 29 symptomatic scaphoid nonunions treated by a simple, minimally invasive procedure using a percutaneous autologous corticocancellous bone graft were evaluated after an average follow-up of 3.5 years. None of the patients had pain at work and all had an almost-normal range of motion and grip strength. No progression to osteoarthritis was observed.[18]
In one study, in patients undergoing three different surgical methods including the Herbert screw fixation, the Matti-Russe bone grafting, or the Kohlman modification of vascularized muscle pedicle graft procedure, there was no significant difference between the union rate in the three methods, but the time to union was earliest in the Kohlman modification of vascularized muscle pedicle graft procedure, which is recommended for patients with old nonunion (>1 year) or proximal pole fractures.[1] However, the Matti-Russe method had a high union rate, which is consistent with our study, and is better specifically for united fractures.
Another study compared the clinical outcomes of the three different bone graft techniques, namely, the Matti-Russe technique, the Fisk-Fernandez technique, and vascularized bone grafting, and reported no statistically significant difference in clinical and radiological outcomes; however, vascularized bone grafting had the shortest time to achieve bone union.[19] Considering the costs, it seems that the nonvascularized Matti-Russe method is worth performing.
Bertelli et al. studied the persistence of nonunion in patients with scaphoid nonunion present for longer than two years, who were treated using a vascularized bone graft harvested from the thumb and pedicled on the first dorsal metacarpal artery by a palmar approach. After one year, 90% of the patients had bone healing with significant pain relief with an improved range of motion and grip strength.[19] This union rate is also almost the same as in our study.
In two other studies, a vascularized interposition graft was recommended as the primary treatment when avascular necrosis was present; it is preferred to make it from the medial femoral condyle (not a distal radial pedicle graft) for the surgical treatment of scaphoid waist nonunion with avascularity of the proximal pole and carpal collapse.[20,21]
In another study, no association was found between the union rate following surgery and either the age of the patient or the interval between the original injury and subsequent nonunion surgery.[22]
In one study evaluating patients with scaphoid fracture that led to pseudoarthritis, the Matti-Rusee technique was reported to be satisfactory. Fracture healing was observed in 81% cases after surgery. Pronation and supination were unaffected; however, radial deviation and extension were impaired. All but one patient could return to work.[12]
Another study also showed that the operative treatment of scaphoid pseudarthrosis by the Matti-Russe method is a reliable procedure with 97% of bony union, and it was reported that this open operation has great technical advantages over Murray's blind method.[13]
Gröner et al. investigated 60 patients with scaphoid nonunion after the Matti-Russe procedure. They found that patients of age younger than 30 years at the time of operation with nonunion diagnosis of a scaphoid fracture less than two years old derive more benefits. In this study, 85% of the autologous corticocancellous bone grafting was successful.[23]
In another study in a pediatric population comparing operative methods including Matti-Russe and Herbert screw fixation with nonoperative method, mean standard immobilization techniques in patients with scaphoid fracture nonunion revealed no significant differences in range of motion and strength between these routes of cure.[24]
This study shows that the modified Matti-Russe method, although old, is still a reliable and inexpensive method for the treatment of scaphoid bone nonunion, showing high percentages of healing and functional improvement, and it can be used in line with the new vascularized surgery methods. It is very helpful to know that our ability to treat scaphoid nonunions has improved dramatically.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Raju P, Kini SG. Fixation techniques for non-union of the scaphoid. J Orthop Surg (Hong Kong) 2011;19:80–4. doi: 10.1177/230949901101900119. [DOI] [PubMed] [Google Scholar]
- 2.Pao VS, Chang J. Scaphoid non-union: Diagnosis and treatment. Plast Reconstr Surg. 2003;112:1666–77. doi: 10.1097/01.PRS.0000086090.43085.66. [DOI] [PubMed] [Google Scholar]
- 3.Leslie I, Dickson R. The fractured carpal scaphoid. Natural history and factors influencing outcome. J Bone Joint Surg Br. 1981;63:225–30. doi: 10.1302/0301-620X.63B2.7217146. [DOI] [PubMed] [Google Scholar]
- 4.Khalid M, Jummani ZR, Kanagaraj K, Hussain A, Robinson D, Walker R. Role of MRI in the diagnosis of clinically suspected scaphoid fracture: Analysis of 611 consecutive cases and literature review. Emerg Med J. 2010;27:266–9. doi: 10.1136/emj.2008.058750. [DOI] [PubMed] [Google Scholar]
- 5.Cooney W, Dobyns JH, Linscheid RL. Fractures of the scaphoid: A rational approach to management. Clin Orthop Relat Res. 1980;149:90–7. [PubMed] [Google Scholar]
- 6.Waters PM, Stewart SL. Surgical treatment of non-union and avascular necrosis of the proximal part of the scaphoid in adolescents. J Bone Joint Surg. 2002;84:915–20. doi: 10.2106/00004623-200206000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Triantafillopoulos I, Zoubos A, Babis G, Soucacos P. Orthopaedica et Traumatologica Hellenica. J Hellenic Ass Orthop Traumatol. 2005:56. [Google Scholar]
- 8.Herbert TJ, Fisher WE. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br. 1984;66:114–23. doi: 10.1302/0301-620X.66B1.6693468. [DOI] [PubMed] [Google Scholar]
- 9.Maruthainar N, Rasquinha V, Gallagher P. The treatment of scaphoid non-union: A review of a novel technique using precision bone grafting compared with Herbert screw fixation and bone graft. J Hand Surg Br. 2000;25:427–30. doi: 10.1054/jhsb.2000.0465. [DOI] [PubMed] [Google Scholar]
- 10.Kawamura K, Chung KC. Treatment of scaphoid fractures and non-unions. J Hand Surg. 2008;33:988–97. doi: 10.1016/j.jhsa.2008.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Filan S, Herbert T. Herbert screw fixation of scaphoid fractures. J Hand Surg Br. 1996;78:519–29. [PubMed] [Google Scholar]
- 12.Stark A, Broström L, Svartengren G. Scaphoid non-union treated with the Matti-Russe technique. Long-term results. Clin Orthop Relat Res. 1987;214:175. [PubMed] [Google Scholar]
- 13.Mulder J. The results of 100 cases of pseudarthrosis in the scaphoid bone treated by the Matti-Russe operation. J Hand Surg Br. 1968;50:110–5. [PubMed] [Google Scholar]
- 14.Panchal A, Kubiak EN, Keshner M, Fulkerson E, Paksima N. Comparison of fixation methods for scaphoid nonunions: A biomechanical model. Bull NYU Hosp Jt Dis. 2007;65:271–5. [PubMed] [Google Scholar]
- 15.Green D. The effect of avascular necrosis on Russe bone grafting for scaphoid non-union. J Hand Surg Am. 1985;10:597–605. doi: 10.1016/s0363-5023(85)80191-x. [DOI] [PubMed] [Google Scholar]
- 16.Parajuli N, Shrestha D, Dhoju D, Shrestha R, Sharma V. Scaphoid fracture: Functional outcome following fixation with herbert screw. Kathmandu Univ Med J (KUMJ) 2012;9:267–73. doi: 10.3126/kumj.v9i4.6342. [DOI] [PubMed] [Google Scholar]
- 17.Ko³odziej R, Blacha J, Bogacz A, Mazurkiewicz T. Long-term outcome of scaphoid non-union treated by the Matti-Russe operation. Ortop Traumatol Rehabil. 2006;8:507–12. [PubMed] [Google Scholar]
- 18.Bullens P, Driesprong M, Lacroix H, Vegter J. Treatment of scaphoid non-union with a percutaneous corticocancellous bone graft. J Hand Surg Br. 2005;30:365–8. doi: 10.1016/j.jhsb.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 19.Bertelli J, Peruchi F, Rost J, Tacca C. Treatment of scaphoid non-unions by a palmar approach with vascularised bone graft harvested from the thumb. J Hand Surg Eur Vol. 2007;32:217–23. doi: 10.1016/J.JHSB.2006.10.014. [DOI] [PubMed] [Google Scholar]
- 20.Jones DB, Jr, Bürger H, Bishop AT, Shin AY. Treatment of scaphoid waist non-unions with an avascular proximal pole and carpal collapse. J Bone Joint Surg Am. 2008;90:2616–25. doi: 10.2106/JBJS.G.01503. [DOI] [PubMed] [Google Scholar]
- 21.Trumble T, Nyland W. Scaphoid non-unions: Pitfalls and pearls. Hand Clin. 2001;17:611–24. [PubMed] [Google Scholar]
- 22.Trezies A, Davis T, Barton N. Factors influencing the outcome of bone grafting surgery for scaphoid fracture non-union. Injury. 2000;31:605–7. doi: 10.1016/s0020-1383(00)00059-0. [DOI] [PubMed] [Google Scholar]
- 23.Gröner R, Zellner PR. Results of follow-up of Matti-Russe surgical treatment of scaphoid pseudarthroses. Handchir Mikrochir Plast Chir. 1995;27:43–5. [PubMed] [Google Scholar]
- 24.Mintzer CM, Waters PM. Surgical treatment of pediatric scaphoid fracture nonunions. J Pediatr Orthop. 1999;19:236–9. doi: 10.1097/00004694-199903000-00020. [DOI] [PubMed] [Google Scholar]


