Abstract
Background:
Disk herniation (DH) is one of the most common disk lesions, inducing low back pain (LBP). Various therapeutic options have been proposed for treatment of disk herniation (DH). Intradiscal injection of ozone has been suggested for treatment of DH.
Objectives:
To determine the effect of intradiscal ozone injection on pain score and disability in patients with LBP from disk prolapsed.
Patients and Methods:
Patients with LBP diagnosed with DH were enrolled in this clinical trial study. After prep and drape the area and under the fluoroscopy guide (c-arm), intradiscal injection of ozone/oxygen mixture (4 mL, 40 µg/mL) was performed. Pain score and functional ability of the patients according to Oswestry Disability Index (ODI) were measured prior to the injection (baseline) and then at 2 and 4 weeks and then at 3 and 6 months after the injection.
Results:
Thirty patients (17 females, 13 males) with the mean age of 58.6 y (range, 42-73 y) enrolled in the study. The mean ± standard deviation (SD) of pain score before intervention was 8.1 ± 0.8. After two weeks, it was reduced to 3.2 ± 0.6 (P < 0.001) and finally dropped to 2.0 ± 0.6 sixth months after intervention (P = 0.0001). Functional status of ODI was 28.5 ± 2.1 before intervention and showed significant reduction after two weeks (with the mean of 12.3), and it was almost sustained till sixth months after intervention, with the mean of 11.4 (P = 0.001).
Conclusions:
Altogether, ozone had significant positive effects on patients with disk herniation unresponsive to other conservative and minimally invasive treatments.
Keywords: Low Back Pain, Ozone, Prolapsed Disk
1. Background
Low back pain (LBP) is one of the most common disorders with prominent effects on patients’ clinical status, socioeconomic situation, and public health. Its one-year prevalence is estimated to be 22%-65%, besides 80% of adults are involved with mild to severe LBP at some points in their lives (1). In about 60%-80% of LBP cases, no specific cause is diagnosed, and in many cases, they are attributed to muscle or ligament strain. In 5% to 15% of cases, the origin of pain was attributed to degenerative joints and disk lesions. Disk or nucleus pulposus herniation is one of the most important disk lesions. Various therapeutic options have been proposed for the treatment of disk herniation (DH), including conservative treatments, less invasive methods (steroid injection, chemonucleosis, intrathecal decompression, laser and annuloplasty), and surgical methods. Non-invasive conservative methods are the first choice in many cases, but failed treatments pop up other less invasive options.
On the other hand, success rate of surgical approach is reported at 49%-95%. Therefore, researchers are seeking less invasive and safer methods. Some of the minimally invasive procedures are used to induce shrinkage of disk tissue, including intradiscal steroid, chemonucleosis, intradiscal decompression, laser, discectomy, and annuloplasty. The common sense of these techniques is a direct effect on disk structure without affecting spinal canal. In a surgical procedure, scar tissue is composed of epidural space, which compresses cord and induces bone adhesions.
Disk herniation induces mechanical compression in addition to biochemical, immunologic and inflammatory changes in the vicinity of disk area. Intradiscal injection is a minimally invasive and inexpensive procedure that induces disk shrinkage and alleviates nerve root inflammation. This procedure is used in many countries, including European countries. In this procedure, a mixture of ozone and oxygen is injected into the disk (2). Ozone affects nucleus pulposus macromolecular structures (proteoglycans and collagens) and has longer duration of action compared with steroid injection in previous reports (3). On the other hand, ozone directly affects disk structures without access to the spinal canal (2). It blocks inflammatory reactions in intraforaminal spaces (due to limited intradiscal space and leakage of gas into this space) and provides rapid and long-term pain relief with minimally invasive procedure and no significant side effect (4-7).
2. Objectives
In this study, we aimed to determine the effect of intradiscal ozone injection on pain score and disability of the patients with LBP caused by prolapsed disk.
3. Patients and Methods
3.1. Study Design
Patients with LBP were enrolled in this clinical trial study. Pain score and functional ability were measured prior to injection (baseline) and then at 2 and 4 weeks and later at 3 and 6 months after injection.
3.2. Primary and Secondary Outcome
Primary outcome of this study was to assess the pain score before and after injection of ozone. Secondary outcome was to assess the functional ability score at the time points mentioned above.
3.3. Sample and Setting
The study was reviewed and approved by the University Review Board and Hospital Ethics Committee. All patients gave their written informed consents prior to the study according to University Hospital Ethics Board Committee. After ethical approval, 30 patients who were referred to the pain clinic due to LBP with or without radicular pain were enrolled in the study. Inclusion criteria were as follows: patients with LBP due to disk disease and VAS Score ≥ 4, radicular pain concurring with imaging for more than 4 weeks and less than 1 year and unresponsive to conservative treatment. MRI findings has been missed in inclusion criteria, which were corrected in the revised manuscript. Discography for finding the correct level of pain and determining pure discogenic LBP were performed before ozone injection. MRI images concurring with dermatome pattern of pain, SLR ≤ 45 or equivocal SLR (LSP-leg pain), and functional impairment were included. Exclusion criteria were positive red flags, presence of bleeding disorder, local infection, uncontrolled or degenerative spine disease (spondylolysis and spondylolisthesis), pregnancy, multilevel disk involvement in discogenic studies, and patient refusal.
3.4. Data Collection
Demographic data, including age, weight, and BMI were obtained. Vital signs at the time of admission, during injection and after injection were collected. Pain score (using visual analogue scale), functional ability score (using Oswestry Disability Index) and laboratory tests, including FBS, Hgb, Hct, platelets, and coagulation tests (CT, BT, PT, PTT, INR) before and after ozone injection were recorded in the participants' questionnaire.
3.5. Intradiscal Ozone Injection
All procedures were performed in the operating room. Patients were monitored for heart rate, blood pressure, and oxygen saturation by pulse oximetry. An IV line access was inserted, and sedation was performed with administration of 0.02 mg/kg midazolam and 1 µg/kg fentanyl in prone position. After prep and drape and under fluoroscopy guide (c-arm) intradiscal injection of ozone/oxygen mixture (4 mL, 40 µg/mL) was performed. Afterward, patients were monitored for extra 4 hours in the recovery room for vital signs and sensory and motor reflexes. Then patients were advised for relative bed rest at home for 48 to 72 hours.
3.6. Statistical Analysis
The data were analyzed with the Software Package for the Social Sciences (SPSS, version 19.0). Data distribution was checked by histogram. Repeated measures ANOVA was used to compare within-subjects with between-subjects effects. 2-tailed P value lower than 0.05 was considered as significant. Sample size was calculated based on previous studies, presuming α = 0.05, power of 80%, and the prediction of pain relief in the ozone group as a minimum clinical difference of 40%.
4. Results
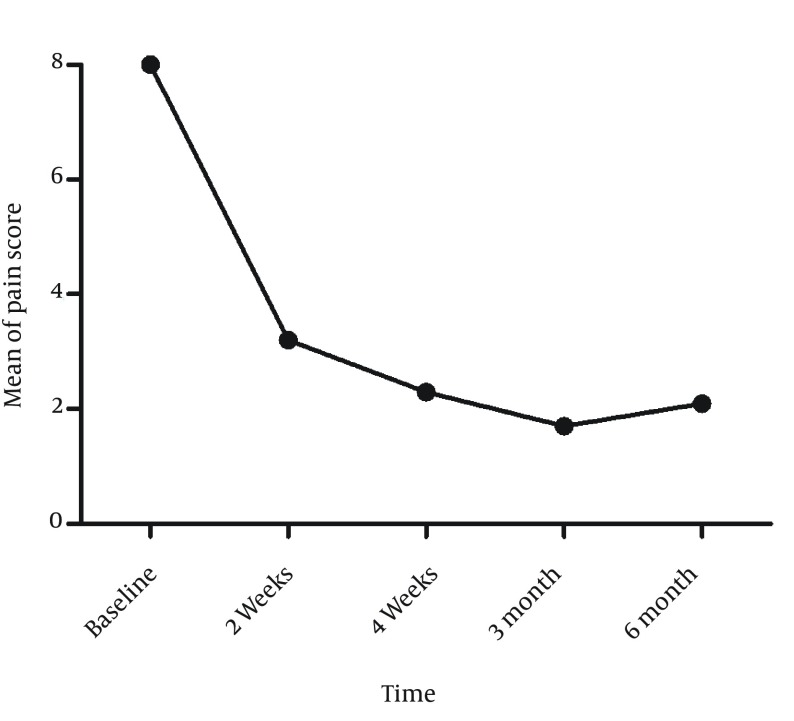
Thirty patients (17 females, 13 males) with the mean age of 58.6 y (range: 42-73 y) entered in the study. The mean ± standard deviation (SD) of pain score before intervention was 8.1 ± 0.8. Vital signs were not significantly different between patients within the group and between two groups. After two weeks, the mean and standard deviation of pain score was reduced to 3.2 ± 0.6 (P < 0.001). This significant reduction was observed in subsequent measurements and finally reached to 2.0 ± 0.6 sixth months after intervention, (tests of within-subjects effects; P < 0.001 and tests of within-subjects contrasts; P < 0.001) (Table 1 and Figure 1).
Table 1. Comparison of Pain Score Measured by Visual Analog scale (VAS) in Follow-up Period With the Baselinea.
| Time Points | VAS for pain (n = 30) | |
|---|---|---|
| Mean ± SD | 95% CI | |
| baseline | 8.1 ± 0.8 | 7.8-8.4 |
| 2 weeks b | 3.2 ± 0.6 | 3.0-3.4 |
| 4 weeks b | 2.1 ± 0.6 | 1.9-2.3 |
| 3 months b | 1.5 ± 0.5 | 1.3-1.7 |
| 6 months b | 2.0 ± 0.6 | 1.8-2.2 |
a Abbreviations: VAS, Visual analog scale; SD, standard deviation; CI, confidence interval.
b P Value < 0.001 compared to baseline.
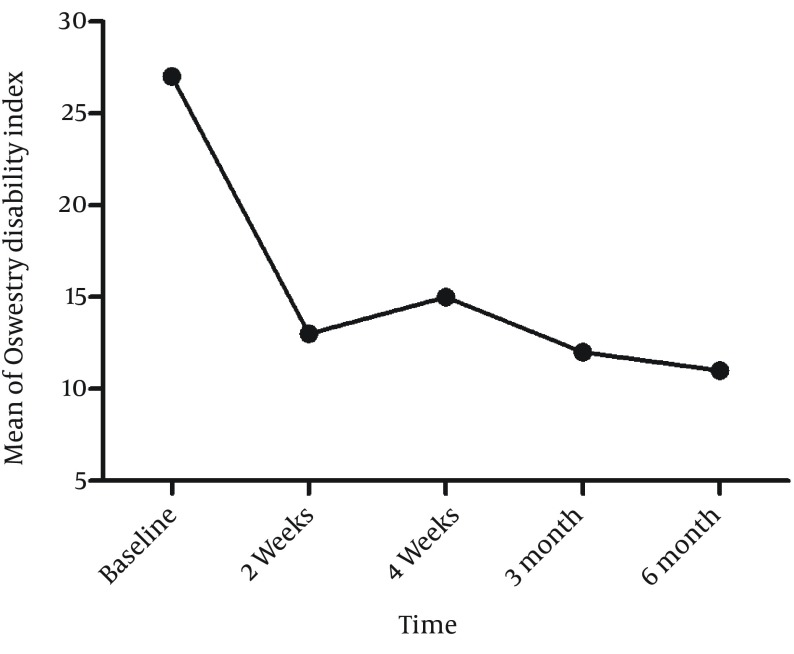
Figure 1. Oswestry Disability Index (ODI) During 6 Month After Ozone Injection.
Also, the functional status of the patients according to Oswestry disability index (ODI), showed a significant improvement in the follow-up period compared with the period before the intervention. The mean ± SD of ODI was 28.5 ± 2.1 before the intervention. There was more than 50% reduction in ODI after two weeks (the mean of 12.3) and it was almost sustained till sixth months after the intervention, with the mean of 11.4, (tests of within-subjects effects; P < 0.001 and tests of within-subjects contrasts; P < 0.001) (Table 2 and Figure 2).
Table 2. Comparison of Oswestry Disability Index in Follow-up Period With the Baselinea.
| ODI (n = 30) | ||
|---|---|---|
| Mean ± SD | 95% CI | |
| Baseline | 28.5 ± 2.1 | 27.7-29.3 |
| 2 weeks b | 12.3 ± 1.8 | 11.6-12.9 |
| 4 weeks b | 13.3 ± 2.0 | 12.6-14.1 |
| 3 months b | 12.0 ± 1.4 | 11.4-12.5 |
| 6 months b | 11.4 ± 1.8 | 10.7-12.1 |
a Abbreviations: ODI, Oswestry disability index; SD, standard deviation; CI, confidence interval.
b P value < 0.001 compared with the baseline.
Figure 2. Pain Score Measured by Visual Analogue Scale (VAS) 6 Months After Ozone Injection.
Patients' age did not show any significant correlation with pain score or ODI. There was no significant difference between males and females in terms of pain score or ODI (tests of between-subjects effects, P = 0.919 and P = 0.561, respectively).
5. Discussion
Disk herniation pathology is composed of both mechanical (nerve roots compression) and biochemical factors (immunologic and inflammatory factors) within the disk space. Ozone injection could significantly decrease intradiscal inflammation and inflammatory process (8). It is a minimally invasive and inexpensive procedure which directly minimizes intradiscal space inflammation and decreases intraforaminal adhesion bands, which induce short-term and long-term pain relief as showed in our results (9, 10). Although there was a significant decrease in pain score and disability two weeks after intradiscal ozone injection; however, the trend of this reduction was continued up to 6 months. Besides, VAS score is an objective scoring and minor flicks are expected during 6 months follow-up. Intradiscal ozone is effective in pain relief as we indicated in our study.
Notably, pain relief depends on many factors, including mechanical and chemical factors. It is well known that feeling pain (with or without radicular pain) is due to both mechanical and chemical factors. Mechanical factors affect disk and its innervations while chemical factors include systemic and local inflammatory reactions (4). Intradiscal ozone injection was first introduced by Muto et al. (5) with positive results. In later studies, positive results of intradiscal ozone injections were depicted. However, long-term efficacy is an issue in many previous studies (6, 11-13). Moreover, patients vary tremendously in their response to intradiscal ozone injection; therefore, its routine use in these patients has been called into question in pain clinics. In Das et al. study (14) both pain and disability scale decreased but long-term efficacy was not investigated.
In another interesting study, Alvarado et al. performed intradiscal ozone injection in 17 patients and paravertebral ozone injection in 103 patients. After 4 months, pain relief was observed in 94% of the patients with intradiscal injection and 86% of the patients with paravertebral injection (15). One important aspect of our study is that we showed a significant decrease in pain and functional disability in a very short period after injection (2 weeks), which remained reasonably stable for quite a long period (6 months). In Gallucci et al. study (16), treatment with intradiscal and intraforaminal injection of steroid and oxygen-ozone versus steroid alone were compared. ODI was better 2 weeks and 6 months after administration of ozone plus steroid compared with steroid alone group; however, they have used a control positive for their study, which was flawed by its non-specific results (on intradiscal ozone injection pain relief effects). Buric et al. study, (6) on 45 patients showed a positive effect of intradiscal ozone on pain scale. Muto et al. showed positive effects of intradiscal injection in 70% of 2200 patients with LBP (7). Same effect was observed in Anderola study by intradiscal injection of ozone and preganglionic injection of steroid in patients with resistant LBP (17).
Although major progress has been made in understanding the mechanism of ozone, but its major pathway is still enigmatic. Ozone not only decreases nerve root compression by reducing disk size, but also decreases vascular stasis by improving microcirculation and oxygen saturation and reduces pain through alleviating hypoxic related pain (18). As a matter of fact, ozone directly affects disk structures without access to the spinal canal (2). On the other hand, ozone inhibits inflammatory reaction by inhibition of prostaglandins and bradykinin in intraforaminal spaces (19). Altogether, ozone has significant and positive effect on patients with disk herniation unresponsive to other conservative and minimally invasive therapies. Nevertheless, the present study has several limitations, including lack of a control group, or blinding. Future studies with larger sample size are required to perform a better review of ozone effects on disk LBP.
Acknowledgments
The authors would like to thank Elaheh Safi for her devoted collaboration.
Footnotes
Authors’ Contributions:Dr. Hashemi suggested the study design; performed critical revision and approved the manuscript; Dr. Poorfarokh performed data collection, analysis, and interpretation; and Dr. Mohajerani drafted the manuscript.
References
- 1.Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J Spinal Disord. 2000;13(3):205–17. doi: 10.1097/00002517-200006000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Gautam S, Rastogi V, Jain A, Singh AP. Comparative evaluation of oxygen-ozone therapy and combined use of oxygen-ozone therapy with percutaneous intradiscal radiofrequency thermocoagulation for the treatment of lumbar disc herniation. Pain Pract. 2011;11(2):160–6. doi: 10.1111/j.1533-2500.2010.00409.x. [DOI] [PubMed] [Google Scholar]
- 3.Masini M, Calaca A. Minimally invasive treatment for refractory low back pain, targeted by epidural endoscopy with O2/O3 and steroid therapy. Acta Neurochir Suppl. 2011;108:33–7. doi: 10.1007/978-3-211-99370-5_6. [DOI] [PubMed] [Google Scholar]
- 4.Magalhaes FN, Dotta L, Sasse A, Teixera MJ, Fonoff ET. Ozone therapy as a treatment for low back pain secondary to herniated disc: a systematic review and meta-analysis of randomized controlled trials. Pain Physician. 2012;15(2):E115–29. [PubMed] [Google Scholar]
- 5.Muto M, Avella F. Percutaneous treatment of herniated lumbar disc by intradiscal oxygen-ozone injection. Interv Neuroradiol. 1998;4(4):279–86. doi: 10.1177/159101999800400403. [DOI] [PubMed] [Google Scholar]
- 6.Buric J, Molino Lova R. Ozone chemonucleolysis in non-contained lumbar disc herniations: a pilot study with 12 months follow-up. Acta Neurochir Suppl. 2005;92:93–7. doi: 10.1007/3-211-27458-8_20. [DOI] [PubMed] [Google Scholar]
- 7.Muto M, Andreula C, Leonardi M. Treatment of herniated lumbar disc by intradiscal and intraforaminal oxygen-ozone (O2-O3) injection. J Neuroradiol. 2004;31(3):183–9. doi: 10.1016/s0150-9861(04)96989-1. [DOI] [PubMed] [Google Scholar]
- 8.Bonetti M, Fontana A, Cotticelli B, Volta GD, Guindani M, Leonardi M. Intraforaminal O(2)-O(3) versus periradicular steroidal infiltrations in lower back pain: randomized controlled study. AJNR Am J Neuroradiol. 2005;26(5):996–1000. [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Jaziri AA, Mahmoodi SM. Painkilling effect of ozone-oxygen injection on spine and joint osteoarthritis. Saudi Med J. 2008;29(4):553–7. [PubMed] [Google Scholar]
- 10.Vaillant JD, Fraga A, Diaz MT, Mallok A, Viebahn-Hansler R, Fahmy Z, et al. Ozone oxidative postconditioning ameliorates joint damage and decreases pro-inflammatory cytokine levels and oxidative stress in PG/PS-induced arthritis in rats. Eur J Pharmacol. 2013;714(1-3):318–24. doi: 10.1016/j.ejphar.2013.07.034. [DOI] [PubMed] [Google Scholar]
- 11.Zhang Y, Ma Y, Jiang J, Ding T, Wang J. Treatment of the lumbar disc herniation with intradiscal and intraforaminal injection of oxygen-ozone. J Back Musculoskelet Rehabil. 2013;26(3):317–22. doi: 10.3233/BMR-130386. [DOI] [PubMed] [Google Scholar]
- 12.Melchionda D, Milillo P, Manente G, Stoppino L, Macarini L. Treatment of radiculopathies: a study of efficacy and tollerability of paravertebral oxygen-ozone injections compared with pharmacological anti-inflammatory treatment. J Biol Regul Homeost Agents. 2012;26(3):467–74. [PubMed] [Google Scholar]
- 13.Paradiso R, Alexandre A. The different outcomes of patients with disc herniation treated either by microdiscectomy, or by intradiscal ozone injection. Acta Neurochir Suppl. 2005;92:139–42. doi: 10.1007/3-211-27458-8_30. [DOI] [PubMed] [Google Scholar]
- 14.Das G, Ray S, Ishwarari S, Roy M, Ghosh P. Ozone nucleolysis for management of pain and disability in prolapsed lumber intervertebral disc. A prospective cohort study. Interv Neuroradiol. 2009;15(3):330–4. doi: 10.1177/159101990901500311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alvarado R, Jimenez J. Initial Experience of Oxygen-Ozone Treatment for Disc Herniation in Bolivia. Ital J oxygen ozone Ther . 2006;5:17–20. [Google Scholar]
- 16.Gallucci M, Limbucci N, Zugaro L, Barile A, Stavroulis E, Ricci A, et al. Sciatica: treatment with intradiscal and intraforaminal injections of steroid and oxygen-ozone versus steroid only. Radiology. 2007;242(3):907–13. doi: 10.1148/radiol.2423051934. [DOI] [PubMed] [Google Scholar]
- 17.Andreula CF, Simonetti L, De Santis F, Agati R, Ricci R, Leonardi M. Minimally invasive oxygen-ozone therapy for lumbar disk herniation. AJNR Am J Neuroradiol. 2003;24(5):996–1000. [PMC free article] [PubMed] [Google Scholar]
- 18.Bocci V, Luzzi E, Corradeschi F, Paulesu L, Di Stefano A. Studies on the biological effects of ozone: 3. An attempt to define conditions for optimal induction of cytokines. Lymphokine Cytokine Res. 1993;12(2):121–6. [PubMed] [Google Scholar]
- 19.Iliakis E, Valadakis V, Vynios DH, Tsiganos CP, Agapitos E. Rationalization of the activity of medical ozone on intervertebral disc-A histological and biochemical study. J Neuroradiol. 2001;14:23–30. [Google Scholar]