Abstract
Caudal epidural block is one of the most commonly performed neuraxial block techniques with reliable peri-operative and post-operative analgesia in pediatric patients. In our randomized, prospective, double-blinded, open level, parallel group study, we have established the effect of caudal epidural block on maintenance requirement of intravenous (IV) propofol in targeted bispectral (BIS) monitored patients.
Context:
Neuraxial anesthesia exhibits sedative properties that may reduce the requirement for general anesthesia. TIVA with propofol has been administered as an established method of maintaining general anesthesia in children. Caudal analgesia being a type of neuraxial block, also seems to reduce the requirement of sedative hypnotics in pediatric patients. Numerous studies show that for patients, administered with caudal epidural block, they require reduced intra-operative volatile inhalation anesthetics. In the present study, we have established the anesthetic sparing effect of Caudal Epidural Analgesia in children undergoing infra-umbilical surgical procedure and calculated the efficacy of propofol-infusion in maintaining adequate depth of anesthesia.
Aims:
(1) To study and compare the dose requirements of propofol using caudal epidural analgesia. (2) To calculate the efficacy of propofol as maintenance anesthetic agent in both groups and to compare hemodynamic stability of patients in both the techniques.
Settings and Design:
In our study, after administering general anesthesia to pediatric patients, we have administered caudal analgesia and IV analgesia to monitor the requirement of intra-operative propofol infusion using BIS monitor with a target value of 40-60 in both groups.
Materials and Methods:
82 patients (aged between 3 and 6 years) have been selected undergoing infra-umbilical surgery and randomly allocated into two groups containing 41 patients in each group. Both the groups group B and group A then intubated with glycopyrrolate, 2 mg/kg injection fentanyl, propofol till loss of verbal contact and atracurium at the rate of 0.5 mg/kg and group B has been administered caudal epidural blockade with 1 ml/kg 0.2% ropivacaine. Propofol infusion at the rate of 10 mg/kg/h is given as maintenance. BIS value has been recorded throughout and propofol requirement at the end of surgery has been calculated.
Statistical Analysis Used:
Numerical variables between groups have been analyzed using the Student's t-test and the Mann-Whitney U-test as applicable. Categorical variables have been analyzed using the Pearson's Chi-square test. P < 0.05 is considered statistically significant.
Results:
Consumption of propofol at the start of operation in the group A is 2.9 ± 0.17 and group B is 2.91 ± 0.17, which is not statistically significant (P > 0.05), whereas at the end of the operation in the group A is 11.33 ± 0.17 and group B is 7.83 ± 0.63, which is statistically significant (P < 0.05). Incidence of adverse effects is statistically insignificant between the two groups. The time for administration of rescue analgesic is 2.1 ± 0.88 in group A and 6.5 ± 0.17 in group B, which is statistically significant due to caudal analgesia.
Conclusions:
We conclude that in BIS-monitored patients (3-6 years) with infra-umbilical surgeries have shown a reduction in consumption of IV propofol due to caudal epidural blockade.
KEY WORDS: Anesthesia, bispectral index monitor, caudal, propofol
INTRODUCTION
Combination of general anesthesia with regional neuraxial anesthesia especially for infra-umbilical surgeries in pediatric patients lasting longer than an hour has been a well-established and accepted method.
Among the regional techniques, caudal epidural blockade is popular in children below 8 years, yields excellent results not only during peri-operative period but also post-operative analgesia.
TIVA with propofol has been administered as an established method of maintaining general anaesthesia in children.[1] Apart from its analgesic properties, caudal block reduces the sedative hypnotic requirement in general anesthesia through various mechanisms.[2] Numerous studies have shown this in cases, where volatile anesthetic namely Sevoflurane has been used for maintenance of intra-operative depth.[3,4]
MATERIALS AND METHODS
The study was performed in N.R.S Medical College and hospital in pediatric surgery operation theater over a period of 6 months, and the study was a randomized, prospective, double-blinded, open-level, parallel-group study.
After obtaining written informed-consent from all parents and approval by the institutional Ethical Committee (ASA-I), patients between the age of 3 and 6 years were selected. Sample size estimation was done after a thorough review of the literature. It was assumed that to detect a mean difference of propofol requirement of 50 mg with a study power of 80% and a probability of type I error as 5%, a total of 82 patients would be required for the study. The within group standard deviation was assumed to be 80 mg. Hence, a total of 82 patients was chosen for the study and allocated uniformly in 2 groups of 41 patients.
Exclusion criteria's taken into account
(i) Pediatric patients <3 years and more than 6 years, (ii) hemodynamically unstable patients, (iii) contraindication to caudal epidural block such as sacral anomaly, bleeding diathesis, (iv) patients with neuromuscular disease, history of epileptic disorder and lipid storage disorder, (v) any known allergy to the drugs used in our study or to the bispectral (BIS) probes.
After selecting the patients were divided into two groups caudal (group B) and control (group A) (n = 41) of age between 3 and 6 years posted for infra umbilical surgery lasting more than 1 h.
Patients were pre-medicated 1 h before surgery with 0.5 mg/kg oral midazolam syrup to ensure a smooth parental separation. Intravenous (IV) access was established with the appropriate size IV cannula after prior application of 50% EMLA cream over the venipuncture site. The patient was then taken inside OT, and ASA standard monitors were applied and BIS probes was applied over the forehead. After that patients were pre-oxygenated with 100% oxygen with a scented face mask of appropriate size.
Patients were pre-medicated with 0.01 mg/kg IV glycolpyrrolate and 2 mcg/kg injection fentanyl. IV propofol was given as a bolus at a pre-calculated value of 1.6-2 mg/Kg body weight or till loss of verbal contact in both the groups. Here, the BIS value and the amount of propofol given were recorded. Then 0.5 mg/Kg atracurium was given to both the groups IV as a loading dose, followed by 0.1 mg/Kg, as and when required. Patient was ventilated for 3 min and intubation was done using an adequately sized ET tube. BIS monitor was kept attached, and values were recorded throughout.
After proper positioning of the patient, caudal epidural block was given with 0.2% ropivacaine 1 ml/kg to the caudal group and nothing was administered to the control group. To overcome observer bias and undergo double blinding, we appointed a second observer, who was not present in the operation theater till the time and was called after positioning of the patients, so that he was not aware of which patient got caudal block and which patient did not.
In this period, when the BIS value went over 40, as monitored by a second observer who started propofol infusion at the rate of 10 mg/Kg/h to both groups targeting to maintain the intra-operative BIS value in the range of 40-60. Hence, patient was maintained by 50% oxygen, 50% nitrous oxide along with propofol infusion. Rescue analgesic in the form of fentanyl was given at the rate of 0.5 mcg/Kg after 1 h of surgery to the control group. If the intra-operative BIS value remained to be 60 persistently, bolus of propofol at 0.5 mg/kg was given, and if it was persistently below 30, propofol infusion was switched off and time was recorded till infusion was switched back on.
Five minute before arousal propofol infusion was switched off, and the amount of drug administered was recorded in both groups. Then the patient was reversed with 50 mg/Kg neostigmine and 10 mcg/Kg glycopyrrolate. The time to arousal and extubation was recorded.
Perioperative monitoring included standard ASA monitoring along with BIS (Aspect Medical Systems, US).
All raw data collected from case report forms were entered into a Microsoft Excel Spreadsheet and analyzed using available statistical software viz. PSPP manufactured by GNU and SPSS 12 manufactured by IBM.
Numerical variables between groups were analyzed using the Student's t-test and the Mann-Whitney U-test as applicable. Categorical variables were analyzed using the Pearson's Chi-square test. P < 0.05 was considered statistically significant.
RESULTS
Of the 82 patients recruited, six have been excluded due to caudal failure and two are excluded due to equipment failure, leaving 74 patients. There has been no significant difference between the two groups (A and B) with respect to age, sex, height, and weight [Table 1].
Table 1.
Demographic profile

We have recorded the important hemodynamic variables like heart rate, systolic blood pressure, diastolic blood pressure, SpO2 throughout the intraoperative period and also the duration of operation. On analyzing the results, we have not found any comparable significant difference between the groups. All the patients in group B have received caudal block and the time from induction to incision is much more, compared to patients of group A, with a statistically significant P = 0.00. The mean time duration from induction to incision of 10.31 min and 19.37 min in groups A and B, respectively, have been calculated.
The consumption of propofol has been recorded at the start and end of the operation, maintaining a targeted BIS value of 40-60 and the results show that Group B patients consumed much less propofol at the end of the operation in comparison to Group A with statistically significant P = 0.00 [Table 2].
Table 2.
Propofol consumption at the start of operation and the end of the operation maintaining BIS value in the range of 40-60

The results, when plotted in a bar diagram, as shown in Figure 1, depict that propofol consumption at the start of operation is 2.9 ± 0.17 and 2.91 ± 0.17 in Groups A and B, respectively (P > 0.05), whereas at the end of operation, in Group A, it is 11.33 ± 0.17 and in Group B, it is 7.83 ± 0.63. This is statistically significant with a P = 0.00.
Figure 1.
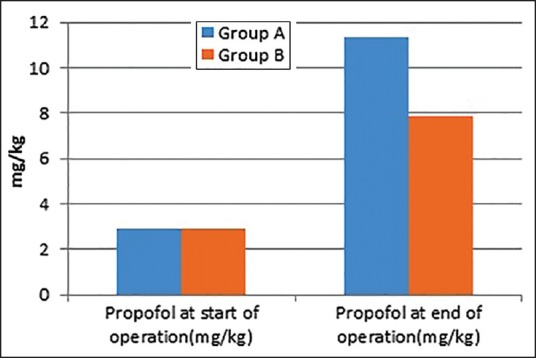
Distribution of propofol consumption during the intraoperative period maintaining bispectral between 40 and 60 in the bar diagram
Routine post-operative side effects like postoperative nausea and vomiting, hypoxia, pain, and electrocardiogram changes have been studied. The effects like sedation and hypotension due to propofol have been studied during immediate post-operative period for the first 8 h, where it is seen that only sedation has occurred in two patients of Group A and one patient of Group B, that is, statistically not significant.
The results also show that pain scores are much less, and time for administration of rescue analgesic is 6.5 ± 0.17 in Group B, in comparison of 2.1 ± 0.88 in Group A, which is statistically significant due to caudal analgesia.
Post-hoc analysis (t-test: Two-sample assuming equal variances) has been performed to verify the significant difference between the two groups A and B, regarding propofol consumption at the end of the operation. It is found that the results are statistically significant after Bonferroni correction. ANOVA single factor test has also been also performed to reconfirm the results.
DISCUSSION
Our results indicate that in children aged between 3 and 6 years, caudal blockade decreases the level of arousal and intra-operative anesthetic maintenance requirement as measured by BIS.
This is consistent with previously reported study for adults by Hodgson and Liu[5] demonstrating decreased scores and reduced anesthetic requirement followed by neuraxial blockade.
Intravenous propofol has been a very good and established drug for induction and maintenance of general anesthesia in children.[1] Caudal analgesia also reduces the requirement of sedative hypnotics in pediatric patients.[2] Reduction of intraoperative maintenance requirement of inhalation anesthetic like sevoflurane by caudal blockade has been well-established.[3,4,5,6,7,8]
Local anesthetics in the epidural space may affect arousal via three mechanisms. First, pain is considered to play the most important role in the arousal from anaesthesia,[9,10,11] caudal analgesia blocks the pain from the surgical site and decreases the general anesthetic demand. Second, neuraxial block reduces the anesthetic requirement by suppressing the movement in response to a noxious stimulus below the level of sensory block. The afferentiation theory proposes that tonic sensory and muscle-spindle activity modulate cerebral activity and maintain a state of wakefulness and decreased afferent input to the brain could lessen the excitatory descending modulation of the spinal cord motor neurons and suppress motor functions.[12,13,14] Third, rostral spread of the local anesthetic in CSF directly affects the brain.[15]
In our study, there has been a significant reduction in IV propofol consumption at the end of surgery in the caudal group (Group B, 7.83 ± 0.63) in comparison to the control group (Group A, 11.33 ± 0.17) with a P < 0.05. It also has been observed that time duration for requirement of rescue analgesic in the postoperative period was much more in Group B (6.5 ± 0.17) than Group A (2.1 ± 0.88).
There are some limitations of our study. First of all, we have allowed 20 min interval following administration of caudal blockade for ropivacaine to take its effect. It is possible that any sedative effect of caudal analgesia may not be seen in this time. There are no published data describing the onset of caudal analgesia, however, clinical experience indicates that the majority of caudal blocks are effective within this time. Second, we are not been able to assess the height of caudal blockade as the patient is under the drapes.
To overcome this limitation to a certain extent, we have administered a pre-calculated dose of ropivacaine, and we have chosen infra-umbilical surgeries mainly the lower ones restricted to perineum. Further, when using the BIS as a measure of arousal, it must be emphasized that BIS is an empiric derivative. Therefore, it should be considered as an ordinal and not in interval scale. The difference between BIS of 70 and 60 is not the same as the difference between 60 and 50. EEG pattern of children is different from that of the adults and BIS monitoring is standardized based on the algorithm developed for adults is definitely a limitation of accuracy of BIS in children; however, the literature[16] shows successful usage of BIS monitoring in children over 2 years age. It may be necessary to develop a standardized algorithm for BIS index in children to get more accurate results.
CONCLUSIONS
It can be concluded from the present study that caudal epidural blockade reduces the consumption of IV propofol during maintenance phase of targeted BIS monitored patients aged between 3 and 6 years posted for infra-umbilical surgeries lasting for more than 1 h. For monitoring the adequate depth of anesthesia, we have used BIS with a set target value of 40-60.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Grundmann U, Uth M, Eichner A, Wilhelm W, Larsen R. Total intravenous anaesthesia with propofol and remifentanil in paediatric patients: A comparison with a desflurane-nitrous oxide inhalation anaesthesia. Acta Anaesthesiol Scand. 1998;42:845–50. doi: 10.1111/j.1399-6576.1998.tb05332.x. [DOI] [PubMed] [Google Scholar]
- 2.Tverskoy M, Shagal M, Finger J, Kissin I. Subarachnoid bupivacaine blockade decreases midazolam and thiopental hypnotic requirements. J Clin Anesth. 1994;6:487–90. doi: 10.1016/0952-8180(94)90089-2. [DOI] [PubMed] [Google Scholar]
- 3.Song JH, Lee HS, Kim BG, Lim HK, Shinn HK, Jung SM. Caudal block reduces demand of sevoflurane for adequate depth of anesthesia in children. Korean J Anesthesiol. 2007;52:29–33. [Google Scholar]
- 4.Kim JS, Park WK, Lee MH, Hwang KH, Kim HS, Lee JR. Caudal analgesia reduces the sevoflurane requirement for LMA removal in anesthetized children. Korean J Anesthesiol. 2010;58:527–31. doi: 10.4097/kjae.2010.58.6.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hodgson PS, Liu SS. Epidural lidocaine decreases sevoflurane requirement for adequate depth of anesthesia as measured by the Bispectral Index monitor. Anesthesiology. 2001;94:799–803. doi: 10.1097/00000542-200105000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Davidson AJ, Ironfield CM, Skinner AV, Frawley GP. The effects of caudal local anesthesia blockade on the Bispectral Index during general anesthesia in children. Paediatr Anaesth. 2006;16:828–33. doi: 10.1111/j.1460-9592.2006.01868.x. [DOI] [PubMed] [Google Scholar]
- 7.Tverskoy M, Shifrin V, Finger J, Fleyshman G, Kissin I. Effect of epidural bupivacaine block on midazolam hypnotic requirements. Reg Anesth. 1996;21:209–13. [PubMed] [Google Scholar]
- 8.Aouad MT, Kanazi GE, Siddik-Sayyid SM, Gerges FJ, Rizk LB, Baraka AS. Preoperative caudal block prevents emergence agitation in children following sevoflurane anesthesia. Acta Anaesthesiol Scand. 2005;49:300–4. doi: 10.1111/j.1399-6576.2005.00642.x. [DOI] [PubMed] [Google Scholar]
- 9.Eappen S, Kissin I. Effect of subarachnoid bupivacaine block on anesthetic requirements for thiopental in rats. Anesthesiology. 1998;88:1036–42. doi: 10.1097/00000542-199804000-00024. [DOI] [PubMed] [Google Scholar]
- 10.Ben-David B, Vaida S, Gaitini L. The influence of high spinal anesthesia on sensitivity to midazolam sedation. Anesth Analg. 1995;81:525–8. doi: 10.1097/00000539-199509000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Shin SK, Hong JY, Kim WO, Koo BN, Kim JE, Kil HK. Ultrasound evaluation of the sacral area and comparison of sacral interspinous and hiatal approach for caudal block in children. Anesthesiology. 2009;111:1135–40. doi: 10.1097/ALN.0b013e3181bc6dd4. [DOI] [PubMed] [Google Scholar]
- 12.Motokizawa F, Fujimori B. Arousal effect of afferent discharges from muscle spindles upon electroencephalograms in cats. Jpn J Physiol. 1964;14:344–53. doi: 10.2170/jjphysiol.14.344. [DOI] [PubMed] [Google Scholar]
- 13.Lanier WL, Iaizzo PA, Milde JH, Sharbrough FW. The cerebral and systemic effects of movement in response to a noxious stimulus in lightly anesthetized dogs. Possible modulation of cerebral function by muscle afferents. Anesthesiology. 1994;80:392–401. doi: 10.1097/00000542-199402000-00019. [DOI] [PubMed] [Google Scholar]
- 14.Doufas AG, Wadhwa A, Shah YM, Lin CM, Haugh GS, Sessler DI. Block-dependent sedation during epidural anaesthesia is associated with delayed brainstem conduction. Br J Anaesth. 2004;93:228–34. doi: 10.1093/bja/aeh192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Iida R, Iwasaki K, Kato J, Ogawa S. Bispectral index is related to the spread of spinal sensory block in patients with combined spinal and general anaesthesia. Br J Anaesth. 2011;106:202–7. doi: 10.1093/bja/aeq359. [DOI] [PubMed] [Google Scholar]
- 16.Ganesh A, Watcha MF. Bispectral index monitoring in pediatric anesthesia. Curr Opin Anaesthesiol. 2004;17:229–34. doi: 10.1097/00001503-200406000-00006. [DOI] [PubMed] [Google Scholar]


