Abstract
Objectives:
To assess the level of knowledge regarding cervical cancer and the acceptance of the human papilloma virus (HPV) vaccine among Saudi female students in health colleges.
Methods:
This cross-sectional study of a convenient sample encompassed 1400 students in Health Colleges at Princess Nora Bint Abdul Rahman University, Riyadh, Saudi Arabia was conducted between December 2013 and February 2014. A self-administrated questionnaire was distributed to all participants. Data collected included socio-demographic data, knowledge of cervical cancer risk factors and clinical presentation, Pap smear, and HPV vaccine acceptance. The questionnaire reliability as tested by Cronbach’s alpha was 0.82.
Results:
The response rate was 89.9%, and data analysis revealed that 95.7% of students had poor knowledge level. The Pap smear was poorly recognized as a screening tool, with 46.7% of students having heard of the test. Senior and medical students had a significantly higher knowledge score. Father’s health profession, high monthly income, and presence of cervical cancer among family members or friends increased the level of knowledge. Vaccine acceptance is influenced by its price, approximately 80% of students thought that an affordable vaccine price should not exceed 300 Saudi Riyals. Perceived barriers to the vaccine were fear of injections and vaccine side effects.
Conclusion:
There is a lack of knowledge and misinformation regarding cervical cancer, Pap smear, and HPV as a major risk factor for cancer of the cervix. These data can be used as a benchmark to formulate effective awareness programs.
Cancer of the cervix uteri is a frequent cancer affecting women, and is a leading cause of mortality worldwide.1 The highest incidence rates have been reported from sub-Saharan Africa, Central and South America, Southeast Asia, and Brazil. In contrast, the incidence rates were the lowest in the Middle East, particularly among Muslims and Jews, as compared to other religious groups.2,3 In the Kingdom of Saudi Arabia, carcinoma of the cervix uteri accounts for 2.6% of female cancers, and is ranked ninth among all carcinomas affecting Saudi females.4 The pathogenesis of cervical cancer in Muslim countries might be different from that of Western societies because of differences in cultural and religious factors that influence human behavior, and reduce the risk of exposure to cervical cancer.4-7 Among all known risk factors, persistent infection with high-risk human papillomavirus (HPV) plays a considerable role in the pathogenesis of cervical cancer.8-11 The worldwide HPV prevalence in cervical cancer was estimated to be between 85-99%.10,12 The HPVs are grouped according to their association with cervical cancer and their genomic sequence into oncogenic high, probable high, and non-oncogenic low-risk.11-14 The strong association of oncogenic HPV infection and the development of cervical cancer provides an opportunity for primary prevention through prophylactic vaccination. Human papillomavirus vaccines (bivalent and quadrivalent) have been shown to be immunogenic, safe, and highly effective in preventing chronic infection and precancerous lesions in women.15,16 The vaccine is available in the KSA market, but national campaigns to vaccinate females are not launched yet.
Cytological screening based on Pap smear plays a major role in reducing both the incidence and mortality of invasive cervical cancer. In the USA and Canada, the reduction in the incidence of cervical cancer and the subsequent reduction of female mortality rate was attributed to the widespread introduction of the Pap smear screening program as a secondary preventive measure for early detection of cases.17-19 However, in Saudi Arabia, most cases present at advanced stages that require extensive chemoradiation therapy. This might be due to lack of proper screening programs,20,21 and inadequate knowledge among the target population. Noteworthy, most female cancer awareness campaigns in KSA are mainly focused on breast cancer. Appropriate level of knowledge, attitude, and beliefs are key elements for adopting a healthy lifestyle, influencing human behaviors, and accepting newly introduced preventive measures. Concerning cervical cancer, the gap of knowledge of clinical presentation, risk factors, primary and secondary prevention has been documented in several studies both in developed and developing countries.22-24 However, few studies have been reported from Saudi Arabia. The present study was designed to assess the level of knowledge and beliefs regarding cervical cancer, and the acceptance of the HPV vaccine among Saudi university students enrolled in health colleges because of their important role as health care providers to raise community awareness and to modify population behavior.
Methods
Study design and study sample
A descriptive cross-sectional study was conducted at the Health Colleges of Princes Nora Bint Abdul Rahman University (PNU) Riyadh, Saudi Arabia between December 2013 and February 2014. The study followed the principals of the Helsinki Declaration, and was approved by the Research and Ethical Committee at PNU. A convenient sample of students aged between 18-25 years were invited to participate in the study. The objectives of the study were explained to the students, and a verbal consent was obtained from each of the participants. The total sample size amounted to 1400 representing students enrolled in Medical, Dental, Nursing, Pharmacy and Health and Rehabilitation Colleges. Lack of consent to complete the questionnaire was the exclusion criteria.
Data collection
A self-administered close ended questionnaire consisting of 48 questions was developed by investigators, guided by study objectives and review of literature.22-24 The questionnaire included 4 sections: the first section comprises socio-demographic data such as age, college, year of study, profession of parents, and monthly income. The second section included 27 items for assessment of knowledge regarding risk factors and symptoms of cancer of the cervix. The responses to these questions included true, false, and don’t know. The third section was related to awareness of the Pap smear as a screening test. In the fourth section, questions related to participants’ perception of safety, efficacy, and acceptance of HPV vaccination were asked in a 5-point Likert scale format, where one indicated strongly disagree and 5 indicated strongly agree. Questions were prepared in the English language and translated into Arabic by 2 experts for better understanding of students. The questionnaire was tested for face and content validity as well as reliability by a pilot study carried out on 20 students, and Cronbach’s alpha was found to be 0.82.
Data analysis
The data were compiled, checked for completeness, and analyzed using the Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, USA) version 20. Results of descriptive analysis of socioeconomic variables, knowledge of cervical cancer, Pap smear, attitude, and acceptance of HPV vaccine were tabulated. The knowledge score represents the sum of the correct answers of the 27 questions in the second section of the questionnaire. The value one was given for the correct answer, and zero for wrong answers, and for “don’t know” responses. The cutoff for a poor knowledge score was set at values below 60% of the total score. Testing the normality distribution of knowledge score revealed skewed distribution; hence, Mann-Whitney test and Kruskal-Wallis were used to compare knowledge scores among different subgroups. P-values of less than 0.05 were considered statistically significant. Multivariate linear regression analysis was adopted to adjust the effect of independent variables on the knowledge score.
Results
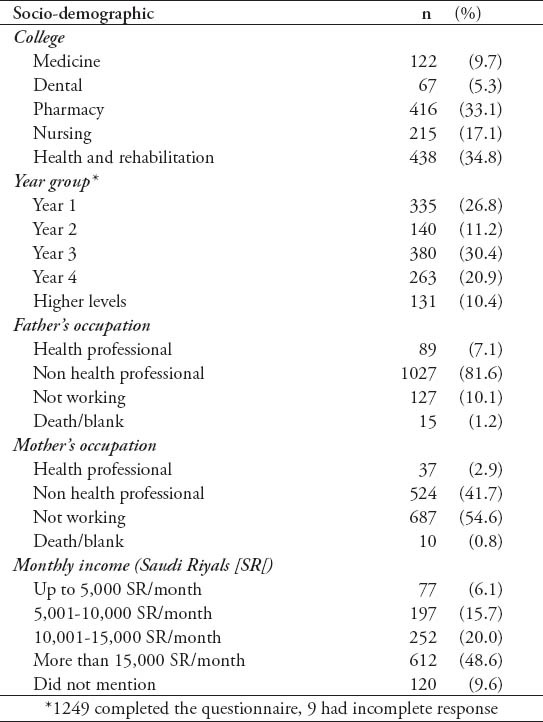
The response rate was 89.9%, and 1258 questionnaires were collected out of the total 1400 students representing the Health Colleges. Table 1 shows the distribution of students according to socio demographic characteristics; a total of 1258 students participated in the survey; their average age was 20.4±1.3 years. Students were distributed between different colleges; comparable percentages were from Pharmacy and Health Rehabilitation (33.1% and 34.8%), and the lowest percentage was from the Dentistry College (n=67, 5.3%). All year groups participated in the study with various percentages; the most common group was year 3 (n=380, 30.4%) whilst the least were from fifth or higher levels (n=131, 10.4%). Regarding parents work, most fathers were working in a non-health professions (81.6%) while most of the mothers were house wives (54.6%). Approximately 1% of students left these fields blank or wrote death as an answer. Only 6.1% of students reported low monthly income (<5,000 Saudi Riyals [SR]) and approximately 49% of students declared high income (more than 15,000 SR/month); moreover, approximately 10% of students did not answer this question.
Table 1.
Distribution of students according to socio-demographic characteristics (1258 items).
The responses to different items for knowledge assessment are displayed in Table 2. Approximately 80% of students recognized breast cancer as the most common cancer among females in Saudi Arabia, and nearly half of them (51.1%) considered cancer cervix as a preventable disease. More than half of the students identified sexually transmitted disease as a risk factor for cancer cervix (59.6%), and a comparable proportion of them marked AIDS (48.9%) and other immunosuppressive disorders as risk factors (48.8%), whereas, nearly 25% of students thought that old age and sexual/perianal warts are risk factors for cancer cervix.
Table 2.
Knowledge on cervical cancer: symptoms, risk factors, secondary and primary prevention.
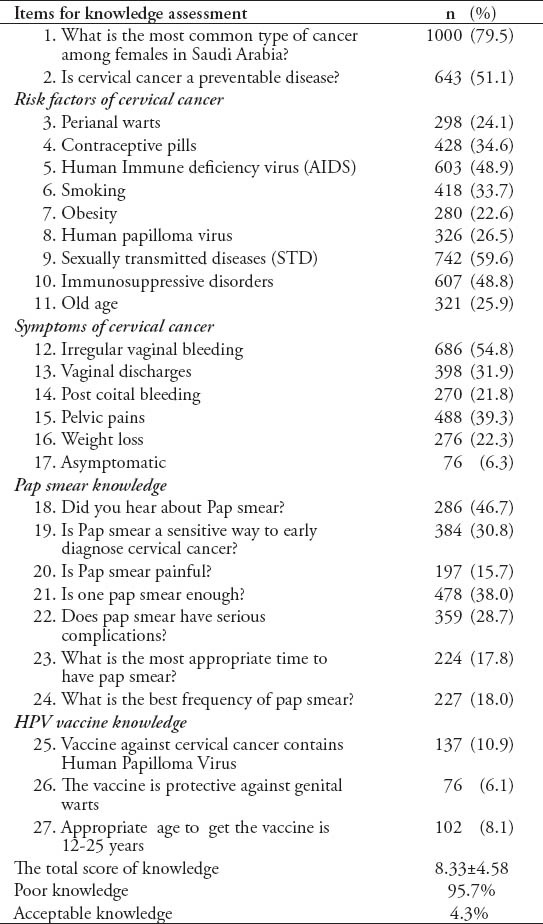
As for clinical presentation of cancer of the cervix, 54.8% knew that irregular vaginal bleeding was a symptom of cervical cancer, whereas 6% deemed that cervical cancer may be asymptomatic (Table 2). Fewer than half of students had heard of the pap smear (46.7%), and nearly 30% of them reported it as sensitive in early detection of cancer cervix. Concerning the frequency of the Pap smear, 38% of students thought that one Pap smear is enough, and 28.7% consider that it has serious complications (Table 2).
Knowledge of the HPV vaccine revealed that merely 10.9% could correctly recognize the viral component of the HPV vaccine, and 6.1% of students positively defined that the HPV vaccine is protective against genital warts, whilst 8% recognized the suitable age for vaccination (Table 2).
Table 3 demonstrates the mean, median, and interquartile range of knowledge score according to the independent variables. For most of the items, the means, and the medians are closely related. The average total score of knowledge among students was 8.33±4.58, the minimum score was (0 out of 27) and the maximum was (24/27). Considering poor knowledge as correctly answering less than 60%, 1080 students (95.7%) were found to have poor knowledge. Further analyses of total knowledge score according to socioeconomic characteristics revealed that students whose parents work in the health professional field showed relatively higher scores (9.05±4.46 for health professional father, and 8.50±3.56 for health professional mother) when compared to those from non-health professions fathers (8.47±4.57) and mothers (8.43±4.62); however, this difference was not conclusive, p>0.05. Average knowledge scores were not widely dissimilar among students of various family income groups (p=0.29); the top average score was 8.53 (monthly income more than 15,000 SR group), whilst the least average score was 7.72 among students whose family income was ranging from 10,001 SR to 15,000 SR per month.
Table 3.
Average knowledge scores, median, and interquartile range (IQR) according to various subgroups in the studied sample.
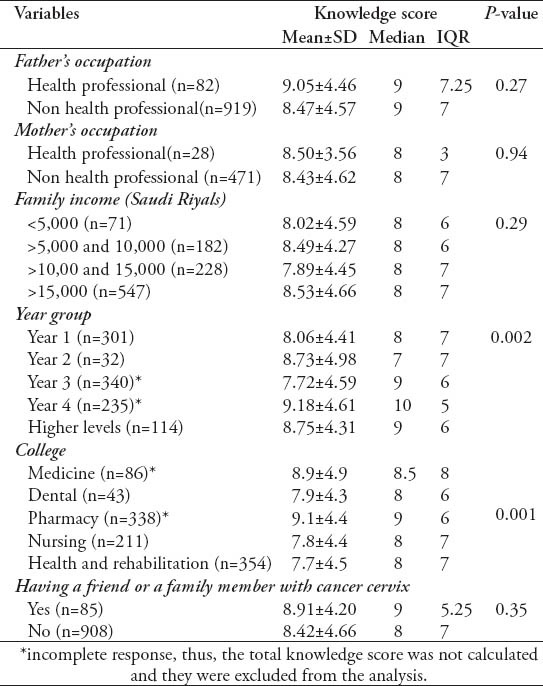
Inequality of knowledge score among different year groups was evident (p=0.002), with the uppermost average score reported for year 4 students (9.18±4.61), and the least was obtained by third-year students (7.72±4.59). The Post-Hoc test (Mann-Whitney) identified that the score of students enrolled in year 3 is significantly lower than other groups, and year 4 students scored significantly higher than other groups (p<0.05). A significant difference among different colleges was also reported; students from colleges of medicine and pharmacy showed significantly higher scores than students from nursing and rehabilitation colleges (Table 3). The linear regression model was used to test the effect of year group on the knowledge score with adjustment of college. The mean knowledge score was found to increase by 0.4 points with each increase in the year group holding the colleges constant (beta coefficient =0.4, p<0.001). Validation of the model was tested via testing the distribution of the residuals, which were found normally distributed.
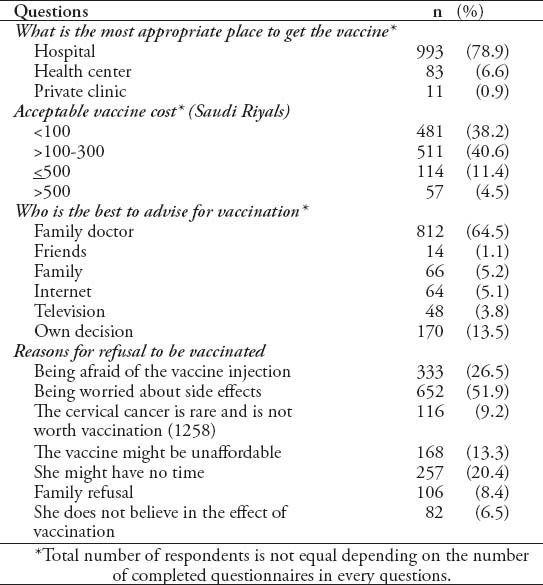
Table 4 demonstrates vaccine acceptance, the principal proportion of students preferred to have the vaccine in hospitals (n=993, 78.9%); however, less than 1% of them preferred the private clinics as a venue for vaccination. Approximately 80% of students thought that the affordable cost of vaccine should not exceed 300 Saudi Riyals (SR) and merely 4.5% will accept the cost to surpass 500 SR. Most students trust the family doctor as the main source of information regarding the vaccine, yet, 13.5% of students would accept to be vaccinated based merely on their own judgment. Regarding barriers for HPV vaccination, being worried regarding side effects was the first reason (51.9%) followed by being afraid of the injection (26.5%). Skepticism in the efficiency of the vaccine was the last reasons behind rejection of the vaccine (6.5%), whereas family refusal was reported by 8.5% of students as a barrier to obtaining the vaccine.
Table 4.
Acceptance and barriers for human papillomavirus vaccine.
Discussion
It is becoming important to raise awareness of cervical cancer in KSA, and the level of knowledge and perception are key elements for adopting healthy behaviors and accepting newly introduced preventive measures. The HPV-related cancer studies have reported the presence of HPV infection, according to the WHO, the HPV accounts for 99% of cases of cervical cancer.25 The vaccine against HPV cervical cancer-related strains has been available in the market since 2006;26 however, most of the available data generally portray a picture of widespread ignorance among the target population regarding HPV infection and vaccination.27-29 In KSA, although there has been increased attention to community health awareness programs, yet, most of the available research has focused on breast cancer, diabetes, and obesity. In contrast, very few studies with a limited sample size have been undertaken to assess the level of knowledge of cervical cancer, and the acceptance of HPV vaccine among Saudis.30,31
Results of the present study regarding knowledge of risk factors of cervical cancer demonstrate knowledge deficits in all items, with a percentage of less than 60% for correct answer in all the 9 questions. Moreover, student’s responses demonstrate confusion, while the percent of correct answers were 59.6% for sexually transmitted diseases, 48.9% for HIV, and 48.8% for immune suppression, only 26.9% considered HPV virus a risk factor for cervical cancer. In addition, students’ knowledge of the link between HPV and the primary prevention of cervical cancer by HPV vaccine is very poor. In 2014, a study was performed among 181 Saudi medical students at King Faisal University, and most of the students had poor knowledge of the early warning signs, symptoms, and risk factors of cervical cancer. On average, the percentages of correct answers ranged from 43.7-55%. In addition, most of the students (67%) were not aware of the availability of a vaccine against HPV.30 Moreover, among Saudi physicians at the Faculty of Medicine, King Abdulaziz University Hospital, Jeddah, only 60.5% of non-gynecological doctors knew that HPV is the major risk factor for cervical cancer, and only 33.8% believed that cervical cancer could be a curable disease.31 Similarly, in Western countries, general awareness of cervical cancer among 17-26 year old students in Poland is insufficient. The HPV infection is not considered to be the major etiological factor.22 Surprisingly, a report from a recent study in Greece among health caregivers demonstrated a significant gap in knowledge of HPV, where only 30% of the sample appears to be aware that HPV infection plays a considerable role in carcinogenesis.23 In accordance with this, findings from a recent survey in Thailand revealed that the level of knowledge regarding HPV is very low.24 However, it can be argued that this study sample represents the top academic level of university students, in addition, a good percentage of them (48.6%) belong to a high socioeconomic standard where the monthly income exceeds 15,000 SR. These 2 factors are expected to impose a positive influence on the level of knowledge both directly and indirectly with good opportunities for better education of family members, which is usually associated with passion to acquire knowledge, in addition to better chances of a high standard of healthcare facilities where health care providers have more time to raise the awareness of their customers.
Questions regarding clinical presentation of cervical cancer revealed lack of knowledge and misinformation, 54.8% consider irregular vaginal bleeding as the presenting symptom, around one third of students thought that vaginal discharge and pelvic pain are the presenting symptoms. The response to post-coital bleeding was 21.8%, while only 6% thought that cervical cancer could be asymptomatic. Lack of knowledge of disease symptomatology might have serious consequences on quality of life as well as on health expenditure. In Saudi Arabia, due to the lack of a national screening program, most cases of cervical cancer present at the advanced stages and require extensive treatment plans with more disabilities and hazards to individual health,20,21 in addition to the burden on the health system and tremendous expenditure of health budget. The influence of clinical presentation of diseases on human attitude and behavior should be considered while planning awareness intervention programs, several studies pointed out that absence of symptoms and vulnerability to the disease might influence the attitude towards preventive measures.32-34
In the present study, the value of the Pap smear as a screening tool for cervical cancer is poorly recognized. Only 46.7% of students have heard about the Pap smear. The percentages of correct answer concerning the test sensitivity to diagnose cervical cancer, frequency of performing Pap smear, and the appropriate time to have it carried out are all low. It is worth mentioning that misconceptions regarding the Pap smear were observed; the test was deemed to be painful by 15.7%, and cause serious complications by 28.7% of participants. Contrary to this, in the USA, and Poland, the data obtained on cytology and the need for regular testing demonstrated a good level of knowledge. The percentage of women who have heard about cytological screening was approximately 90%.22,35-38 The contributing factors for the observed difference are multifactorial including; the widespread introduction of Pap smear as a screening program, gender education programs in schools, an intensive public awareness campaign, and the onset of HPV vaccine programs in Western countries started earlier than in the Middle East and the Gulf region.
In broad terms, the vast majority of students had a low level of knowledge, the mean knowledge score amounted to 8.33±4.58, and overall 95% of participants had poor knowledge. Although father’s health profession, monthly income >15,000 SR, and presence of cervical cancer among a family member or a friend increased the level of knowledge, yet, none of these factors imposed a conclusive effect on the knowledge score. A significantly higher knowledge score was reported for year 4 students, as well as for students enrolled in Medical and Pharmacy schools than for junior students or students from other colleges. This might be related to the content of curricula exposing students to more in-depth information in topics pertaining to viral infection and cancers. The association between age and knowledge of causes of cervical cancer and transmission of HPV is a reflection of the educational level as shown in studies carried out among nurses from Tanzania and Thailand.39-41 Assessment of knowledge of 289 adults recruited from a local university health service, and 2 family practice clinics in Michigan confirmed that knowledge score is positively correlated with years of education, female gender, and being married.42
Data pertaining to vaccine acceptance demonstrate that most students preferred to obtain the vaccine in hospitals. Despite the relatively high monthly income, around 80% of students thought that the affordable vaccine price should not exceed 300SR. Several studies have confirmed that the price of the vaccine is an important motivating factor to accept the HPV vaccine.43-46 Among Hungarian school children, 80% of respondents would get vaccinated if the vaccine were available free of charge.47 It is worth mentioning that vaccine side effects and fear of injections are perceived barriers for HPV vaccine among a considerable proportion of students enrolled in the present study. Similarly, concerns regarding the vaccine’s side effects and other factors related to vaccine efficacy, age of target population, religious consideration have been reported.48
The limitations of the present study were; the dissimilar proportions of the numbers of respondents in different colleges, also, males and students from non-health colleges are not represented. However, the results provide valuable information on the awareness of Saudi female university students pertaining to cervical cancer. This study is the first phase of a 2 phase project, the second intervention phase will be guided by the results of the present study. Also, this data will be useful for health caregivers in planning community education.
In conclusion, this study indicates a poor level of knowledge of cervical cancer and misinformation regarding primary and secondary preventive measures among Saudi female students enrolled in health colleges at Princess Nora University in Riyadh City. The data provide a benchmark on the level of knowledge, which can be used to formulate effective awareness program.
Footnotes
Related Articles.
Wang YH, Chen DJ, Yi TN, Liu XH. The relationship among human papilloma virus infection, survivin, and p53 gene in lung squamous carcinoma tissue. Saudi Med J 2010; 31: 1331-1336.
Sait KH. Attitudes, knowledge, and practices in relation to cervical cancer and its screening among women in Saudi Arabia. Saudi Med J 2009; 30: 1208-1212.
Jamal A, Al-Maghrabi JA. Profile of Pap smear cytology in the Western region of Saudi Arabia. Saudi Med J 2003; 24: 1225-1229.
References
- 1.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 2.Christoperson WM, Lundin FE, Jr, Mendez WM, Parker JE. Cancer cervical control. Study of morbidity and mortality trends over a twenty-one-year period. Cancer. 1976;38:1357–1366. doi: 10.1002/1097-0142(197609)38:3<1357::aid-cncr2820380340>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 3.Konno R, Sagae S, Yoshikawa H, Basu PS, Hanley SJ, Tan JH, et al. Cervical Cancer Working Group Report. Jpn J Clin Oncol. 2010;40(Suppl 1):i44–i50. doi: 10.1093/jjco/hyq126. [DOI] [PubMed] [Google Scholar]
- 4.Special Edition. Riyadh (KSA): Saudi Cancer Registry, Ministry of Health; 2011. Saudi Cancer Registry. Cancer Incidence and Survival Report: Saudi Arabia 2007. [Google Scholar]
- 5.Jamal A, Al-Maghrabi JA. Profile of Pap smear cytology in the Western region of Saudi Arabia. Saudi Med J. 2003;24:1225–1229. [PubMed] [Google Scholar]
- 6.Bhurgri Y, Bhurgri A, Rahim A, Bhutto K, Pinjani PK, Usman A, et al. The pattern of malignancies in Karachi (1995 to 1996) J Pak Med Assoc. 1999;49:157–161. [PubMed] [Google Scholar]
- 7.Raza SA, Franceschi S, Pallardy S, Malik FR, Avan BI, Zafar A, et al. Human papillomavirus infection in women with and without cervical cancer in Karachi, Pakistan. Br J Cancer. 2010;102:1657–1660. doi: 10.1038/sj.bjc.6605664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hausen H. Papillomaviruses in the causation of human cancers-a brief historical account. Virology. 2009;384:260–265. doi: 10.1016/j.virol.2008.11.046. [DOI] [PubMed] [Google Scholar]
- 9.Bosch FX, Manos MM, Munoz N, Sherman M, Jansen AM, Peto J, et al. Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. International biological study on cervical cancer (IBSCC) Study Group. J Natl Cancer Inst. 1995;87:796–802. doi: 10.1093/jnci/87.11.796. [DOI] [PubMed] [Google Scholar]
- 10.Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189:12–19. doi: 10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 11.Muñoz N, Bosch FX, de Sanjosé S, Herrero R, Castellsagué X, Shah K. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348:518–527. doi: 10.1056/NEJMoa021641. [DOI] [PubMed] [Google Scholar]
- 12.Sanjose S, Quint WG, Alemany L, Geraets DT, Klaustermeier JE, Lloveras B, et al. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 2010;11:1048–1056. doi: 10.1016/S1470-2045(10)70230-8. [DOI] [PubMed] [Google Scholar]
- 13.Bernard HU, Burk RD, Chen Z, van Doorslaer K, Hausen H, de Villiers EM. Classification of papillomaviruses (PVs) based on 189 PV types and proposal of taxonomic amendments. Virology. 2010;401:70–79. doi: 10.1016/j.virol.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Human papillomaviruses. IARC Monogr Eval Carcinog Risks Hum. 2007;90:1–636. [PMC free article] [PubMed] [Google Scholar]
- 15.FUTURE II Study Group. Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N Engl J Med. 2007;356:1915–1927. doi: 10.1056/NEJMoa061741. [DOI] [PubMed] [Google Scholar]
- 16.Paavonen J, Naud P, Salmerón J, Wheeler CM, Chow SN, Apter D, et al. Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young women. Lancet. 2009;374:301–314. doi: 10.1016/S0140-6736(09)61248-4. [DOI] [PubMed] [Google Scholar]
- 17.Wang SS, Sherman ME, Hildesheim A, Lacey JV, Jr, Devesa S. Cervical adenocarcinoma and squamous cell carcinoma incidence trends among white women and black women in the United States for 1976-2000. Cancer. 2004;100:1035–1044. doi: 10.1002/cncr.20064. [DOI] [PubMed] [Google Scholar]
- 18.Sherman ME, Wang SS, Carreon J, Devesa SS. Mortality trends for cervical squamous and adenocarcinoma in the United States. Relation to incidence and survival. Cancer. 2005;103:1258–1264. doi: 10.1002/cncr.20877. [DOI] [PubMed] [Google Scholar]
- 19.Mathew A, George PS. Trends in incidence and mortality rates of squamous cell carcinoma and adenocarcinoma of cervix--worldwide. Asian Pac J Cancer Prev. 2009;10:645–650. [PubMed] [Google Scholar]
- 20.Dosoky M, Ismail N, Dagastani M. Preinvasive cervical carcinoma in Saudi Arabia. Lancet. 1995;345:650. doi: 10.1016/s0140-6736(95)90551-0. [DOI] [PubMed] [Google Scholar]
- 21.Manji M. Cervical cancer screening program in Saudi Arabia: action is overdue. Ann Saudi Med. 2000;20:355–357. doi: 10.5144/0256-4947.2000.355. [DOI] [PubMed] [Google Scholar]
- 22.Kamzol W, Jaglarz K, Tomaszewski KA, Puskulluoglu M, Krzysztof K. Assessment of knowledge about cervical cancer and its prevention among female students aged 17–26 years. Eur J Obstet Gynecol Reprod Biol. 2013;166:196–203. doi: 10.1016/j.ejogrb.2012.10.019. [DOI] [PubMed] [Google Scholar]
- 23.Notara V, Soultatou P, Tselika A. Lay knowledge of HPV infection and the vaccine against HPV in Greece. Health Science Journal. 2012;6:270–279. [Google Scholar]
- 24.Kietpeerakool C, Phianmongkhol Y, Jitvatcharanun K, Siriratwatakul U, Srisomboon J. Knowledge, awareness, and attitudes of female sex workers toward HPV infection, cervical cancer, and cervical smears in Thailand. Int J Gynaecol Obstet. 2009;107:216–219. doi: 10.1016/j.ijgo.2009.07.023. [DOI] [PubMed] [Google Scholar]
- 25.Geneva: WHO; 2008. World Health Organization. Cervical cancer, human papillomavirus (HPV), and HPV vaccines. [Google Scholar]
- 26.Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H, Unger ER, et al. Quadrivalent Human Papillomavirus Vaccine: Recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2007;56(RR-2):1–24. [PubMed] [Google Scholar]
- 27.Das A, Madhwapathi V, Davies P, Brown G, Dearnley E, Spencer A, et al. Knowledge and acceptability of the HPV vaccine by school children and their parents in Birmingham. Vaccine. 2010;28:1440–1446. doi: 10.1016/j.vaccine.2009.11.041. [DOI] [PubMed] [Google Scholar]
- 28.Picerno I, Sturniolo G, Spadafora M, Nasso E, Di Pietro A, Spataro P. Secondary school students knowledge and awareness of HPV infections and vaccine. Prev Med. 2010;51:427–428. doi: 10.1016/j.ypmed.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 29.Agius PA, Pitts MK, Smith AM, Mitchell A. Human papillomavirus and cervical cancer: Gardasil vaccination status and knowledge amongst a nationally representative sample of Australian secondary school students. Vaccine. 2010;28:4416–4422. doi: 10.1016/j.vaccine.2010.04.038. [DOI] [PubMed] [Google Scholar]
- 30.Al-Darwish AA, Al-Naim AF, Al-Mulhim KS, Al-Otaibi NK, Morsi MS, Aleem AM. Knowledge about Cervical Cancer Early Warning Signs and Symptoms, Risk Factors and Vaccination among Students at a Medical School in Al-Ahsa, Kingdom of Saudi Arabia. Asian Pac J Cancer Prev. 2014;15:2529–2532. doi: 10.7314/apjcp.2014.15.6.2529. [DOI] [PubMed] [Google Scholar]
- 31.Sait KH. Knowledge, attitudes, and practices regarding cervical cancer screening among physicians in the Western Region of Saudi Arabia. Saudi Med J. 2011;32:1155–1160. [PubMed] [Google Scholar]
- 32.Roy B, Tricia ST. Cervical cancer screening in Kolkata, India: Beliefs and predictors of cervical cancer screening among women attending a women's Health Clinic in Kolkata. J Cancer Educ. 2008;23:253–259. doi: 10.1080/08858190802189105. [DOI] [PubMed] [Google Scholar]
- 33.Ackerson K, Gretebeck K. Factors influencing cancer screening practices of underserved women. J Am Acad Nurse Pract. 2007;19:591–601. doi: 10.1111/j.1745-7599.2007.00268.x. [DOI] [PubMed] [Google Scholar]
- 34.Byrd TL, Petterson SK, Chavez R, Heckert A. Cervical cancer screening beliefs among young Hispanic women. Prev Med. 2004;38:192–197. doi: 10.1016/j.ypmed.2003.09.017. [DOI] [PubMed] [Google Scholar]
- 35.Doescher MP, Jackson JE. Trends in cervical and breast cancer screening practices among women in rural and urban areas of the United States. Journal of Public Health Management and Practice. 2009;15:200–209. doi: 10.1097/PHH.0b013e3181a117da. [DOI] [PubMed] [Google Scholar]
- 36.Nelson W, Moser RP, Gaffey A, Waldron W. Adherence to cervical cancer screening guidelines for U.S. women aged 25–64: data from the 2005 Health Information National Trends Survey (HINTS) Journal of Women's Health. 2009;18:1759–1768. doi: 10.1089/jwh.2009.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hawkins NA, Cooper CP, Saraiya M, Gelb CA, Polonec L. Why the pap test? Awareness and use of the Pap test among women in the United States. Journal of Women's Health. 2011;20:511–515. doi: 10.1089/jwh.2011.2730. [DOI] [PubMed] [Google Scholar]
- 38.Smith RA, Cokkinides V, Brooks D, Saslow D, Shah M, Brawley OW. Cancer screening in the United States, 2011: a review of current American Cancer Society guidelines and issues in cancer screening. CA Cancer J Clin. 2011;61:8–30. doi: 10.3322/caac.20096. [DOI] [PubMed] [Google Scholar]
- 39.Urasa M, Darj E. Knowledge of cervical cancer and screening practices of nurses at a regional hospital in Tanzania. Afr Health Sci. 2011;11:48–57. [PMC free article] [PubMed] [Google Scholar]
- 40.Duval B, Gilca V, Boulianne N, Pielak K, Halperin B, Simpson MA, et al. Cervical cancer prevention by vaccination: nurses’ knowledge, attitudes and intentions. J Adv Nurs. 2009;65:499–508. doi: 10.1111/j.1365-2648.2008.04900.x. [DOI] [PubMed] [Google Scholar]
- 41.Tessaro I, Herman C. Changes in public health nurses’ knowledge and perception of counselling and clinical skills for breast and cervical cancer control. Cancer Nurs. 2000;23:401–405. doi: 10.1097/00002820-200010000-00012. [DOI] [PubMed] [Google Scholar]
- 42.Holcomb B, Bailey JM, Crawford K, Ruffin MT. Adults’ Knowledge and Behaviors Related to Human Papillomavirus Infection. J Am Board Fam Pract. 2004;17:26–31. doi: 10.3122/jabfm.17.1.26. [DOI] [PubMed] [Google Scholar]
- 43.Dinas K, Nasioutziki M, Arvanitidou O, Mavromatidis G, Loufopoulos P, Pantazis K, et al. Awareness of human papillomavirus infection, testing and vaccination in midwives and midwifery students in Greece. J Obstet Gynaecol. 2009;29:542–546. doi: 10.1080/01443610902977684. [DOI] [PubMed] [Google Scholar]
- 44.Madhivanan P, Krupp K, Yashodha MN, Marlow L, Klausner JD, Reingold AL. Attitudes toward HPV vaccination among parents of adolescent girls in Mysore, India. Vaccine. 2009;27:5203–5208. doi: 10.1016/j.vaccine.2009.06.073. [DOI] [PubMed] [Google Scholar]
- 45.Donders GG, Bellen G, Declerq A, Berger J, Van Den Bosch T, Riphagen I, et al. Change in knowledge of women about cervix cancer, human papillomavirus (HPV) and HPV vaccination due to introduction of HPV vaccines. Eur J Obstet Gynecol Reprod Biol. 2009;145:93–95. doi: 10.1016/j.ejogrb.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 46.Sauvageau C, Duval B, Gilca V, Lavoie F, Ouakki M. Human papillomavirus vaccine and cervical cancer screening acceptability among adults in Quebec, Canada. BMC Public Health. 2007;7:304. doi: 10.1186/1471-2458-7-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marek E, Dergez T, Rebek-Nagy G, Kricskovics A, Kovacs K, Bozsa S, et al. Adolescents’ awareness of HPV infections and attitudes towards HPV vaccination 3 years following the introduction of the HPV vaccine in Hungary. Vaccine. 2011;29:8591–8598. doi: 10.1016/j.vaccine.2011.09.018. [DOI] [PubMed] [Google Scholar]


