Abstract
Objectives:
To study the association between gingival biotypes and inclination and position of the maxillary and mandibular incisors.
Methods:
This cross-sectional study included 142 consecutive orthodontic patients (64 males and 78 females) who were seeking orthodontic treatment at the Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia from February 2013 to January 2014. Gingival biotype was assessed independently for the maxillary and mandibular central incisors using the transparency of periodontal probe method. Maxillary and mandibular incisors’ inclination and position were measured using cephalometric analysis.
Results:
The mean age was 23.56 (±2.55) years. The prevalence of thin gingival biotype was 43% for the maxillary and 52.1% for the mandibular incisors. Females were 4 times more likely to have thin gingiva for the maxillary incisors and 5 times more likely for the mandibular incisors. A significant association was found between mandibular incisor inclination and position and thin gingival biotype, while there was no association between the maxillary incisor inclination and position and gingival biotypes.
Conclusion:
Mandibular incisor proclination and protrusion is associated with thin gingival biotype while no association is found in the maxilla. The evaluation of the gingival biotype is essential during diagnosis and treatment planning for potential orthodontic patients.
The inclination and position of incisor teeth is an important factor when planning orthodontic tooth movement. In recent years, there have been several investigations regarding the limits to the degree of incisor proclination in the dental arch.1-4 The effect of proclination may consequently lead to gingival recession. Gingival recession can be generalized or localized, affecting one tooth surface or more, and might lead to an esthetic impairment.5,6 Several factors were suggested to play a role in the development of gingival recession. The main known etiologic factors, among others, are periodontal diseases, and mechanical trauma.7 Periodontal health is a prerequisite prior to starting any orthodontic tooth movement. The role of orthodontic tooth movement in the development of gingival recession is still a debatable subject.8-10 Even though some found an increase in gingival recession in adolescents and adults, 3,4,9 others did not find that gingival recession was induced by orthodontic fixed appliance therapy.1,11 The inconsistencies between these studies could be attributed to the fact that the etiology of gingival recession is complex. Several factors were suggested to modulate the incidence of gingival recessions following orthodontic therapy, for example: the total orthodontic tooth movement, the quality of oral hygiene, and the gingival biotype.1-3,12 The evaluation of the gingival biotype is essential, especially prior to orthodontic tooth movement because it defines the soft and hard tissues surrounding teeth. Gingival biotype can be classified as thin or thick.13 The thin gingival biotype is characterized by delicate soft tissue with a minimal amount of attachment that is susceptible to trauma and inflammation while the thick gingival biotype is characterized by dense, fibrotic soft tissue with a large amount of attachment. Thick gingivae are generally suggested as the model of periodontal health.14 Reduction in gingival thickness is considered a predisposing factor to marginal tissue recession during orthodontic treatment, and proper clinical assessment of gingival biotype will insure accurate decision-making during planned incisor inclination. This is supported by one study where they observed an increase in the risk of gingival recession after orthodontic treatment when the thickness of free gingival margin is less than 0.5mm especially when it comes to incisor proclination.3 The prevalence of different gingival biotypes varies depending on the studied population. In a Saudi sample, the prevalence of thin gingival biotype was 25% among males and 64% in females.15 The association between dental malocclusion and the prevalence of gingival biotype has been previously studied and no significant association was demonstrated.15 However, the relationship between the maxillary or mandibular incisors inclination and position and gingival biotypes has not been previously studied. This study therefore aimed to evaluate the association between gingival biotypes and the inclination and position of the maxillary and mandibular incisors. A secondary aim was to study the relationship between gingival biotypes and space analysis in the anterior segment of both arches.
Methods
This cross-sectional study consisted of 142 consecutive orthodontic patients (64 males and 78 females) who were seeking orthodontic treatment at the Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia from February 2013 to January 2014. The study was reviewed and approved by the Research Ethics Committee at the Faculty of Dentistry, King Abdulaziz University, and was carried out in compliance with the Helsinki declaration. Informed consent was obtained from participants prior to their enrollment in the study. Exclusion criteria were: 1) patients with missing any of the maxillary or mandibular anterior teeth, 2) patients with gingival inflammation, crowns or extensive restorations on their anterior maxillary or mandibular teeth, 3) pregnant or lactating female patients, 4) patients who are taking certain medications with known effects on the periodontal soft tissues, 5) patients who required antibiotic pre-medication prior to dental examination, 6) smoking, and 7) history of previous periodontal surgery or orthodontic treatment.
The evaluation of gingival biotype was assessed for every patient by one calibrated investigator. Prior to evaluation of study subjects, intra-examiner repeatability was evaluated by assessing the gingival biotypes (thin or thick) of 10 subjects not involved in the study at 2 different occasions, 2 weeks apart. The investigator was able to achieve the same finding 90% of the time. Gingival biotype was assessed using the method described previously.16 This evaluation method was based on whether the periodontal probe (Michigan-O probe with William's color-coded markings, Hu-Friedy, Chicago, IL, USA) was visible through the gingival margin while probing the sulcus at the mid facial aspect of both maxillary and mandibular central incisors.17,18 When the underlying periodontal probe could be seen through the gingiva, it was classified as thin, otherwise it was considered thick.
Inclination (proclination/retroclination) and position (protrusion/retrosion) of the maxillary and mandibular incisors were assessed on lateral cephalometric radiographs using the Kodak 8000C digital panoramic and cephalometric System (Kodak-Trophy, Croissy-Beaubourg, Marne-la-Vallée, France). Each subject's head was stabilized by positioning the ear-rods of the cephalostat machine in the external auditory meatus with the Frankfort plane parallel to the horizon and sagittal plane at right angle to the path of the x-ray and the teeth in centric occlusion with the lips in a closed and relaxed position. The cephalogram images were then imported into VistadentOC® software (Vistadent®OC, Dentsply, Birmingham, AL, USA) and digitally traced by one investigator, and the landmarks used are shown in Figure 1. The measurements that are illustrated in Figure 1 were used to calculate the maxillary and mandibular incisor inclination and position.
Figure 1.
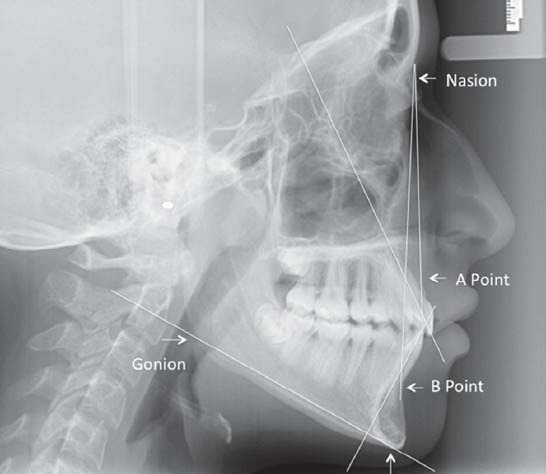
Cephalometric landmarks and planes used to measure the inclination and position of the maxillary and mandibular incisors. Nasion: The most anterior point on the fronto-nasal suture in the midsagittal plane. A Point: The most posterior midline point in the concavity between the anterior nasal spine and Prosthion (the inferior point on the alveolar bone overlying the maxillary central incisors). B Point: The most posterior midline point in the concavity of the mandible between the most superior point on the alveolar bone overlying the mandibular central incisors (Infradentale) and Pogonion. Gonion: A point on the curvature of the angle of the mandible located by bisecting the angle formed by lines tangent to the posterior ramus and the inferior border of the mandible. Menton: The lowest point on the symphyseal shadow of the mandible seen on a lateral cephalogram.
Maxillary incisor inclination
The angle formed by the intersection of a line from nasion to A point (NA) with a line drawn along the maxillary central incisor long axis (U1).
Maxillary incisor position
The distance formed from the most labial point on the upper central incisor (U1) to the NA line.
Mandibular incisor inclination
The angle formed by the intersection of a line drawn along the mandibular plane (Gonion-Menton) with a line drawn along the mandibular central incisor long axis (L1).
Mandibular incisor position
The distance formed from the most labial point on the mandibular incisor (L1) to the NB line.
Space analysis to measure the amount of spacing or crowding present in the anterior segment of each arch was performed by measuring the space available and space required in the maxillary and mandibular arches mesial to the canines. The available arch space mesial to the canines on each arch was measured with digital caliper accurate to 0.1 mm (Pittsburgh 4” Digital Caliper, Harbor Freight Tools, Calabasas, CA, USA). The space required was calculated by measuring the mesiodistal dimension of each incisor tooth at its greatest interproximal distance.
Statistical analysis
Data were tabulated and analyzed using the Statistical Package for Social Sciences Version 20.0 (IBM SPSS Statistics for Mac, Armonk, NY: IBM Corp, USA). Means and frequency distributions were calculated for continuous and categorical variables. The bivariate relationship between gingival biotype, and gender, inclination, and position of the maxillary or mandibular incisors was assessed using the Chi-square [x2] for categorical data and Student's t-test for continuous data. Multivariate analysis to evaluate the relationship between gingival biotypes and the study variables were conducted using the logistic regression models. A p-value less than 0.05 was considered the statistically significant level.
Results
The mean age in years of the study sample was 23.56 (±2.55) with no significant difference between those with thin (23.23±2.63) and thick (23.81±2.47) gingival biotype (p=0.18). The gender distribution of the maxillary and mandibular gingival biotype is presented in Table 1. Frequency of thin gingival biotype was significantly greater in females than males in both maxillary and mandibular incisors, p=0.001.
Table 1.
Gingival biotype for the maxillary and mandibular arches by gender among 142 consecutive orthodontic patients.
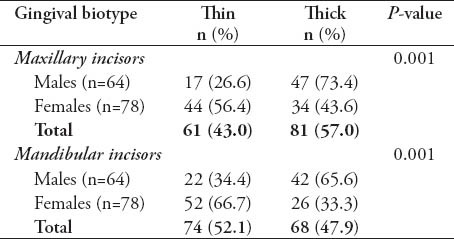
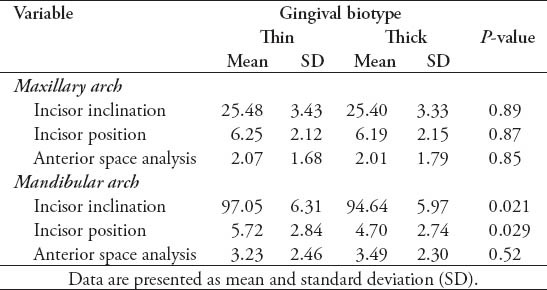
Table 2 shows the bivariate comparisons between thin and thick gingival biotypes with regards to incisor inclination and position and anterior spacing/crowding for the maxillary and mandibular teeth. For the maxillary incisors, there were no significant differences in the means of maxillary inclination, position, and space analysis between thin and thick gingival biotypes. For the mandible, the incisor inclination and position were significantly greater in the thin gingival biotype when compared to the thick gingival biotype. No significant difference in the space analysis was found between thin and thick gingival biotypes in the mandibular arch.
Table 2.
Incisor inclination and position and anterior space analysis in subjects with thin and thick gingival biotypes.
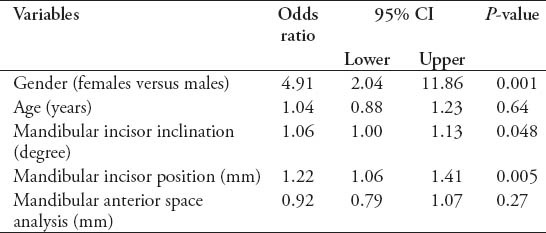
Regression analysis for the maxillary anterior incisors (Table 3) showed that females were 4.2 times more likely to have thin gingiva than males (p=0.001) controlling for age, maxillary incisor inclination, and position, and anterior space analysis. Other variables were not significantly associated with gingival biotypes. In the mandibular arch, the regression analysis (Table 4) showed that females were almost 5 times more likely than males to have thin gingival biotype. Furthermore, there was a significant association between thin gingival biotype and an increased mandibular incisor inclination (p=0.005) and position (p=0.048).
Table 3.
Multivariable association between the studied variables and gingival biotype in the maxilla
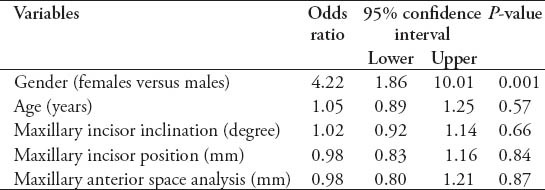
Table 4.
Multivariable association between the studied variables and gingival biotype in the mandible.
Discussion
The results of this study demonstrated that mandibular incisor proclination and protrusion were significantly associated with thin gingival biotype while no association was observed between the gingival biotypes and inclination and position of the maxillary incisors. Reduction in gingival thickness is one factor that might contribute to periodontal tissue breakdown.5 Hence, the direction and magnitude of orthodontic forces should be carefully controlled especially in subjects with thin gingival biotype. During orthodontic tooth movement, including proclination, several biologic events occur leading to bone remodeling of the alveolar process, which supports the teeth and their roots.19 Bone resorption takes place in the direction of tooth movement leading to reduction in the alveolar bone volume; however, if the alveolar bone is thin, it could be a complicating factor during orthodontic treatment. Therefore, the hard and soft tissue boundaries that outline the teeth, as suggested by Proffit et al20 should be carefully analyzed. Cook et al,17 demonstrated that thin gingival biotype is associated with a thin underlying labial plate while a thick gingival biotype is associated with a thicker labial plate. It was also suggested that one of the indications for surgical procedure to augment the gingival soft tissue is orthodontic movement outside the alveolus in the presence of thin gingival biotype.21 In one study, it was shown that when the roots are displaced away from the center of the alveolar bone, there would be an increased probability of alveolar dehiscence and gingival recession.3 Also, when teeth are moved more labial, thickness of the bone, and gingivae overlying the root could be affected.4,10,12 Accordingly, careful consideration should be taken when attempting labial movement since thin gingivae may be more prone to recession.22 Previous studies demonstrated that in 85% of the studied sample, the periodontium was not affected under controlled incisor proclination and proper oral hygiene. However, they emphasized that contributing risk factors such as gingival thickness should be identified.1,2 Nonetheless, in these studies cephalometric analysis to measure the actual inclination and position of the incisors was not performed. Earlier studies made no distinction between maxillary and mandibular gingival biotypes. However, a recent study, questioned the uniqueness of gingival biotype as it might differ between maxillary and mandibular arches.23 In the present study, the prevalence of thin gingival biotype was independently assessed for the maxillary and mandibular incisors and the results showed a prevalence of 43% in the maxillary and 52.1% in the mandibular incisors. The prevalence of thin gingival biotype was significantly more in females than males which is similar to previous reports.15,18 In the present study, females were 4 times more likely to have thin gingival biotype in the maxillary incisors than males, and 5 times more in the mandibular incisors than males.
To date, no previous study has assessed the association between gingival biotypes, and inclination and position of the maxillary and mandibular incisors prior to orthodontic treatment, which was addressed in this study. Proclination and protrusion of mandibular incisors were associated with thin gingival biotype, and labial movement of these teeth might increase the risk for the development of bone dehiscence and gingival recession in patients with thin gingival biotype. Knowledge concerning the prevalence of thin or thick gingival biotypes can be potentially useful during patient evaluation and risk appraisal for orthodontic patients. For example, certain patients with thin gingival biotype may benefit from gingival augmentation prior to orthodontic treatment. Therefore, further studies to evaluate this concept are merited.
The limitation of this study is that it was cross-sectional and hence, gives no indication of the sequence of events. Another limitation is that the sample was drawn from a pool of patients from one center and that may prejudice the findings.
In conclusion, mandibular incisor proclination and protrusion are associated with thin gingival biotype while no association is found in the maxilla. The evaluation of the gingival biotype is essential during diagnosis and treatment planning for potential orthodontic patients. The orthodontist should balance the pros and cons when deciding to procline or protrude incisors, particularly in the mandible. Future longitudinal studies are recommended to examine the relationship between gingival biotypes, symphysis width, facial index, and different orthodontic treatment modalities.
Footnotes
Disclosure.
Related Articles.
Balto HA, Al-Manei KK, Bin-Mohareb TM, Shakoor ZA, Al-Hadlaq SM. Cytotoxic effect of Salvadora persica extracts on human gingival fibroblast cells. Saudi Med J 2014; 35: 810-815.
Dayal P, Ahmed J, Ongole R, Boaz K. Solitary neurofibroma of the gingiva. Saudi Med J 2014; 35: 607-611.
Zawawi KH, Al-Harthi SM, Al-Zahrani MS. Prevalence of gingival biotype and its relationship to dental malocclusion. Saudi Med J 2012; 33: 671-675.
References
- 1.Allais D, Melsen B. Does labial movement of lower incisors influence the level of the gingival margin? A case-control study of adult orthodontic patients. Eur J Orthod. 2003;25:343–352. doi: 10.1093/ejo/25.4.343. [DOI] [PubMed] [Google Scholar]
- 2.Melsen B, Allais D. Factors of importance for the development of dehiscences during labial movement of mandibular incisors: a retrospective study of adult orthodontic patients. Am J Orthod Dentofacial Orthop. 2005;127:552–561. doi: 10.1016/j.ajodo.2003.12.026. quiz 625. [DOI] [PubMed] [Google Scholar]
- 3.Yared KF, Zenobio EG, Pacheco W. Periodontal status of mandibular central incisors after orthodontic proclination in adults. Am J Orthod Dentofacial Orthop. 2006;130:6.e1–6.e8. doi: 10.1016/j.ajodo.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 4.Renkema AM, Fudalej PS, Renkema AA, Abbas F, Bronkhorst E, Katsaros C. Gingival labial recessions in orthodontically treated and untreated individuals: a case-control study. J Clin Periodontol. 2013;40:631–637. doi: 10.1111/jcpe.12105. [DOI] [PubMed] [Google Scholar]
- 5.Al-Zahrani MS, Bissada NF. Predictability of connective tissue grafts for root coverage: clinical perspectives and a review of the literature. Quintessence Int. 2005;36:609–616. [PubMed] [Google Scholar]
- 6.Zawawi KH, Malki GA, Al-Zahrani MS, Alkhiary YM. Effect of lip position and gingival display on smile and esthetics as perceived by college students with different educational backgrounds. Clin Cosmet Investig Dent. 2013;5:77–80. doi: 10.2147/CCIDE.S53359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alghamdi H, Babay N, Sukumaran A. Surgical management of gingival recession: A clinical update. Saudi Dental Journal. 2009;21:83–94. doi: 10.1016/j.sdentj.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Closs LQ, Grehs B, Raveli DB, Rösing CK. Occurrence, extension, and severity of gingival margin alterations after orthodontic treatment. World J Orthod. 2008;9:e1–e6. [PubMed] [Google Scholar]
- 9.Slutzkey S, Levin L. Gingival recession in young adults: occurrence, severity, and relationship to past orthodontic treatment and oral piercing. Am J Orthod Dentofacial Orthop. 2008;134:652–656. doi: 10.1016/j.ajodo.2007.02.054. [DOI] [PubMed] [Google Scholar]
- 10.Vasconcelos G, Kjellsen K, Preus H, Vandevska-Radunovic V, Hansen BF. Prevalence and severity of vestibular recession in mandibular incisors after orthodontic treatment. Angle Orthod. 2012;82:42–47. doi: 10.2319/021411-108.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Artun J, Grobéty D. Periodontal status of mandibular incisors after pronounced orthodontic advancement during adolescence: a follow-up evaluation. Am J Orthod Dentofacial Orthop. 2001;119:2–10. doi: 10.1067/mod.2001.111403. [DOI] [PubMed] [Google Scholar]
- 12.Joss-Vassalli I, Grebenstein C, Topouzelis N, Sculean A, Katsaros C. Orthodontic therapy and gingival recession: a systematic review. Orthod Craniofac Res. 2010;13:127–141. doi: 10.1111/j.1601-6343.2010.01491.x. [DOI] [PubMed] [Google Scholar]
- 13.Kao RT, Fagan MC, Conte GJ. Thick vs. thin gingival biotypes: a key determinant in treatment planning for dental implants. J Calif Dent Assoc. 2008;36:193–198. [PubMed] [Google Scholar]
- 14.Kao RT, Lee S, Harpenau L. Clinical challenges in diagnosing and monitoring periodontal inflammation. J Calif Dent Assoc. 2010;38:263–270. [PubMed] [Google Scholar]
- 15.Zawawi KH, Al-Harthi SM, Al-Zahrani MS. Prevalence of gingival biotype and its relationship to dental malocclusion. Saudi Med J. 2012;33:671–675. [PubMed] [Google Scholar]
- 16.Kan JY, Morimoto T, Rungcharassaeng K, Roe P, Smith DH. Gingival biotype assessment in the esthetic zone: visual versus direct measurement. Int J Periodontics Restorative Dent. 2010;30:237–243. [PubMed] [Google Scholar]
- 17.Cook DR, Mealey BL, Verrett RG, Mills MP, Noujeim ME, Lasho DJ, et al. Relationship between clinical periodontal biotype and labial plate thickness: an in vivo study. Int J Periodontics Restorative Dent. 2011;31:345–354. [PubMed] [Google Scholar]
- 18.De Rouck T, Eghbali R, Collys K, De Bruyn H, Cosyn J. The gingival biotype revisited: transparency of the periodontal probe through the gingival margin as a method to discriminate thin from thick gingiva. J Clin Periodontol. 2009;36:428–433. doi: 10.1111/j.1600-051X.2009.01398.x. [DOI] [PubMed] [Google Scholar]
- 19.Henneman S, Von den Hoff JW, Maltha JC. Mechanobiology of tooth movement. Eur J Orthod. 2008;30:299–306. doi: 10.1093/ejo/cjn020. [DOI] [PubMed] [Google Scholar]
- 20.Proffit WR, Fields HW, Sarver DM. Contemporary Orthodontics. 4th ed. St. Louis (MO): Mosby Elsevier; 2007. [Google Scholar]
- 21.Mehta P, Lim LP. The width of the attached gingiva-much ado about nothing? J Dent. 2010;38:517–525. doi: 10.1016/j.jdent.2010.04.007. [DOI] [PubMed] [Google Scholar]
- 22.Baker P, Spedding C. The aetiology of gingival recession. Dent Update. 2002;29:59–62. doi: 10.12968/denu.2002.29.2.59. [DOI] [PubMed] [Google Scholar]
- 23.Cuny-Houchmand M, Renaudin S, Leroul M, Planche L, Guehennec LL, Soueidan A. Gingival biotype assessment: visual inspection relevance and maxillary versus mandibular comparison. Open Dent J. 2013;7:1–6. doi: 10.2174/1874210601307010001. [DOI] [PMC free article] [PubMed] [Google Scholar]


