Abstract
Objective
Among married prostate cancer (PC) patients, the spouse is often the primary provider of emotional support and personal care. However, few studies have investigated spouses’ illness beliefs (i.e., about disease duration and treatment control) and their impact on patients’ quality of life (QOL). Spouses’ beliefs about disease duration (timeline) were hypothesised to mediate relationships between spouses’ treatment control beliefs and patients’ QOL six months later.
Methods
Fifty-three patients, who underwent localised treatment for PC, and their spouses, completed an illness beliefs measure (the revised Illness Perception Questionnaire). Patients completed a QOL measure (the Functional Assessment of Cancer Therapy – General) six months later.
Results
Spouse timeline beliefs mediated the association between spouse treatment control beliefs and patient QOL six months later (total indirect effect = −0.71, 95% CI 0.02-2.03). That is, spouse beliefs that the treatment would control their loved one's illness led to beliefs that the disease would be of shorter duration, which in turn led to improved patient QOL six months later. This relationship did not occur with patients’ beliefs.
Conclusions
Results highlight the important influence of spouse illness beliefs over time on patient QOL with implications for clinical care and dyadic research.
Keywords: cancer, spouses, prostate cancer, quality of life, illness beliefs, treatment control
Introduction
Prostate cancer (PC) is the most common cancer diagnosis in men in the US and the second leading cause of cancer death in US men after lung cancer (American Cancer Society, 2012). Although survival rates for those with localised PC are high (Howlader et al., 2011), the quality of life (QOL) of men with PC may still be negatively affected by the various treatments available to them (e.g., surgery, radiation therapy, active surveillance; Thompson et al., 2007). Sexual dysfunction and urinary dysfunction, for example, are potential adverse effects of surgery and radiation therapy (Dunn & Kazer, 2011; Galbraith, Ramirez, & Pedro, 2001). Active surveillance may be associated with increased psychological distress and worries about cancer progression or metastasis (Bailey, Wallace, & Mishel, 2007; Hedestig, Sandman, & Widmark, 2003; Wallace, 2003).
The experience of cancer itself has often been construed as a stressful event for patients and their spouses (Butler et al., 2005; Jim & Jacobsen, 2008; Kangas, Henry, & Bryant, 2002). The cognitive processing literature on adjustment to trauma suggests that when a traumatic event occurs, it can challenge an individual's core assumptions about the self and other people (Epstein, 1973; Janoff-Bulman, 1992; Parkes, 1971). Such core assumptions may also include beliefs about the controllability and predictability of the world a person inhabits (Janoff-Bulman, 1992). Following diagnosis, PC patients and their spouses may be faced with multiple opinions by multiple doctors regarding how to proceed (American Urological Association, 2007). Hence, once the chosen treatment has been undertaken, beliefs about the ability of the treatment to control the disease will likely be salient to patients and spouses.
Research has shown that patients’ beliefs about their illness are important predictors of QOL in a wide range of illnesses (e.g., Alsen, Brink, Persson, Brandstrom, & Karlson, 2010; Covic, Seica, Gusbeth-Tatomir, Gavrilovici, & Goldsmith, 2004; Tiemensma et al., 2011) including PC (Traeger et al., 2009). Leventhal and colleagues’ self-regulation theory (Leventhal, Nerenz, & Steele, 1984) has provided a useful framework for describing patients’ beliefs and expectations of their illness. In short, illness beliefs regarding a health threat lead patients to engage in behaviors to manage the event, which then lead to appraisals to evaluate the outcome of those actions. Such illness beliefs (also referred to as illness representations or illness perceptions) include the following components: identity, consequences, timeline, control/cure and cause). Traeger and colleagues (2009) investigated illness beliefs in men who were within 18 months of completing treatment for localised PC. A number of illness beliefs (treatment control, illness coherence, negative consequences, or personality and behavioural causes of PC) combined explained a significant variance in emotional well-being.
Among married cancer patients, the spouse is often the primary provider of emotional support and personal care, and can promote health behaviours (Hodgkinson et al., 2007). Not only are most familial caregivers women, but they are also likely to experience more burden than male caregivers of female patients (e.g., greater negative impact on employment, greater disruption of personal routines; Siegel, Raveis, Mor, & Houts, 1991). Despite the important role spouse caregivers play in the care of their loved one, few studies have examined illness beliefs among spouses and their potential impact on patients’ QOL. One study that did examine illness beliefs in cardiac patients and their spouses focused on the impact of dissimilarities in illness beliefs on patient self-rated health and coping strategies (Karademas, Zarogiannos, & Karamvakalis, 2010). The study findings revealed no significant association between dissimilarities in illness perceptions and patients’ self-rated health, although they did find relations with certain coping strategies. For example, when the couple shared the same view of the illness as being coherent, predictable and manageable, patients reported using less palliative coping and wishful thinking strategies and more instrumental coping strategies. A second study examined the level of patient and partner agreement of their appraisals of PC as they related to health-related QOL. Overall, findings suggested that (dis)agreement was generally associated with worse adjustment outcomes for both patients and partners (Merz et al., 2011).
With improved treatment options and excellent survival rates for PC patients, certain illness beliefs may be particularly salient for patients and spouses – specifically, treatment control beliefs, and by extension, beliefs about the timeline of the illness (i.e., whether it will be of short or long duration). Most studies that have examined relations between illness beliefs and QOL in cancer patients have focused on patients’ illness beliefs, have been cross-sectional in nature and have not investigated relationships between different individuals’ illness beliefs (e.g., Rozema, Vollink, & Lechner, 2009; Scharloo et al., 2010; Traeger et al., 2009). With respect to the variables of interest in the present study, Cameron and Moss-Morris (2006) note that treatment control beliefs are typically associated with timeline beliefs and there is evidence in the literature to support this relation (Moss-Morris et al., 2002; Shah, Hull, & Riley, 2009). Furthermore, they appear to be distinct constructs as evidenced by their modest correlation (Moss-Morris et al., 2002) and have been found to be related to QOL (e.g., Griva, Jayasena, Davenport, Harrison, & Newman, 2009). Clarifying the nature of this association, and in turn, its impact on patients’ QOL, would help health care practitioners in the identification and treatment of individuals who might be most prone to QOL difficulties.
Due to the likely salience of treatment control and timeline beliefs for both PC patients and their spouses, it is important to examine the magnitude and the direction of associations among these illness beliefs and patients’ QOL. It is likely that for both patients and spouses, believing that the treatment will be efficacious (i.e., better treatment control) will be associated with beliefs that the patient's illness will be of short rather than long duration (i.e., shorter timeline). The larger scale study did not measure behavioural actions that might have arisen from the illness beliefs. However, we envisaged that this association would influence coping behaviours and adaptation responses, reinforce daily life activities and shape interactions between the couple that would likely bolster the patient's QOL (Leventhal, Brissette, & Leventhal, 2003). For example, the belief that the illness is treatable, and thus be of short duration, might lead a spouse to plan more active couple activities “as if” the patient is healthy, and that actually promote QOL in the patient.
In sum, the purpose of the present study was to explore whether illness beliefs about the timeline of the illness mediates relations between illness beliefs about treatment control and patient QOL six months later. We hypothesised that stronger patient beliefs about treatment control would be associated with stronger patient timeline beliefs (i.e., that their illness would be of short rather than long duration), which, in turn, would be associated with more positive perspectives of patient QOL at a later date. Due to the vital role that spouses often play in their loved one's care and daily life activities, we anticipated that spousal beliefs would be significant in predicting QOL in their loved ones at a later time point. Thus, we hypothesised that stronger spousal beliefs about treatment control would be associated with stronger spousal beliefs that their loved one's illness would be of short (rather than long) duration, which, in turn, would be associated with better patient QOL six months later.
Method
Participants and Procedures
Data for this study come from a large-scale longitudinal study examining QOL and illness beliefs in PC patients. Spouses were also included in the study in order to examine their illness beliefs related to their partner's illness and treatment. All study procedures were approved by the institutional review board at the study site. Informed consent was received prior to any patient's or their spouse's study involvement. Patients were men diagnosed with early-stage, localised PC who had not yet decided on a form of treatment, were free of substantial comorbidity, and fluent in English. Collaborating physicians mailed an informed consent form and questionnaire to interested and eligible patients and spouses. In order to capture patients’ illness representations following treatment, this study assessed patients and spouses six months after recruitment into the study at which time 99% of the patients had begun or completed treatment (Time 1 for the present secondary analyses). Patients were assessed again at Time 2 (an additional six months later). Spouses were also assessed at Time 1. Participants received $10 for each questionnaire they returned. One hundred and twenty-two couples completed the Time 1 assessment, and 53 couples completed the Time 2 assessment. Data from patients and spouses who responded to both time points were included in the analyses (n = 53).
Participant characteristics are given in Table 1. The patient sample consisted of 53 men who had undergone localised treatment for non-metastatic PC. Their average age was 64.52 years (SD = 9.02 years). Most were Caucasian (92.5%). Just over half of the sample (56.6%) had completed a college education. The average age of their spouses was 60.59 years (SD = 9.54 years). Spouses were also mostly Caucasian (94.3%), and 39.6% had completed a college education. For the patients, PC diagnosis had occurred on average 94 days (SD = 100 days) prior to the baseline (pre-treatment) time point for the larger scale study. The first assessment time point for the current analyses occurred six months after that time point to ensure that patients had already completed localised treatment. Most of the patient participants received radiation therapy (56.6%).
Table 1.
Participant characteristics (n=53).
| Characteristic | n | % | M | SD | Range |
|---|---|---|---|---|---|
| Patient age | 64.5 | 9.0 | 43-84 | ||
| Spouse age | 60.6 | 9.5 | 46-79 | ||
| Patient ethnicitya: | |||||
| Caucasian | 49 | 92.5 | |||
| African American | 3 | 5.7 | |||
| Spanish/Latino/Hispanic | 1 | 1.9 | |||
| Spouse ethnicitya: | |||||
| Caucasian | 50 | 94.3 | |||
| African American | 2 | 3.8 | |||
| Spanish/Latino/Hispanic | 1 | 1.9 | |||
| Patient educational levelb: | |||||
| Grade school | 6 | 11.3 | |||
| High school | 17 | 32.1 | |||
| College degree | 18 | 34.0 | |||
| Post graduate degree | 12 | 22.6 | |||
| Spouse educational levelb: | |||||
| Grade school | 1 | 1.9 | |||
| High school | 31 | 58.5 | |||
| College degree | 12 | 22.6 | |||
| Post graduate degree | 9 | 17.0 | |||
| Days since diagnosis to Time 1 | 94.4 | 99.5 | 24-556 | ||
| Type of treatmentc: | |||||
| Radiation therapy | 28 | 52.8 | |||
| Surgery | 14 | 26.4 | |||
| Radioactive seed implantation | 5 | 9.4 | |||
| Surgery and radiation therapy | 1 | 1.9 | |||
| Radiation therapy and seed implantation | 1 | 1.9 | |||
| Radiation therapy and watchful waiting | 1 | 1.9 | |||
| Missing | 3 | 5.7 |
Notes
For analyses, ethnicity was coded as 0=non-Caucasian, 1=Caucasian.
For analyses, educational level was coded as 0=less than college degree, 1=college degree or higher
For analyses, type of treatment was coded as 0=non-surgical treatment, 1=surgery
Measures
Treatment control and timeline beliefs were measured using the treatment control and the timeline (acute/chronic) subscales of the revised Illness Perception Questionnaire – revised (IPQ-R; Moss-Morris et al., 2002), a well-validated self-report measure of illness beliefs as described by Leventhal's self-regulatory model (Leventhal et al., 1984). Although the IPQ-R has a subscale for timeline (cyclical), this was not used for the study due to the fact that PC patients in the early stages of their disease are more likely to deal with a relatively discrete treatment course (e.g., radical prostatectomy, external beam radiation therapy) and less likely to deal with a cyclical illness experience as might be found in other illnesses (e.g., asthma, schizophrenia). An example of a treatment control item is ‘My treatment will be effective in curing my PC’ and an example of a timeline item is ‘The prostate cancer will last a short time’. Patients and spouses rated items on a five-point Likert response scale, ranging from 1 = strongly disagree to 5 = strongly agree. Negatively valenced items were reverse coded so that higher scores on these subscales equated with more positive beliefs about treatment control and a shorter PC timeline. Internal consistency for patients on this measure was good (Cronbach's α = 0.88) and acceptable for spouses (Cronbach's α = 0.74).
Patient general QOL was assessed with the Functional Assessment of Cancer Therapy – General instrument (Cella et al., 1993). This 27-item scale is a commonly used and well-validated measure of the functional status of cancer patients. It measures four primary QOL domains: physical well-being (e.g., ‘I am bothered by side effects of treatment’), social/family well-being (e.g., ‘I get emotional support from my family’), emotional well-being (e.g., ‘I worry that my condition will get worse’) and functional well-being (e.g., ‘I am able to work [include work at home]’). Negatively valenced items were reverse-coded. A total general QOL score was generated by summing all subscale scores. Higher total scores represent better general QOL. In this study, internal reliability was excellent (Cronbach's α = 0.90).
Sociodemographic and medical variables included self-reported age, race, and level of education. Medical variables were gathered from medical chart review and self-report, and included days since diagnosis and type of treatment received. Additional medical variables were gathered about sexual function and urinary function. Sexual function was measured using three items from the sexual adjustment questionnaire (Waterhouse & Metcalfe, 1986) assessing ‘whether the patient has had the desire for sexual activity’, ‘whether he is too tired for sexual activity’ and ‘whether he had been able to get and keep an erection when sexually excited’. The second item was reverse coded so that higher scores had a positive valence. Items were scored on a five-point scale (1 = not at all; 5 = very much) with higher scores pointing to higher levels of sexual function. Principal component analysis (PCA) of the three items in our earlier work yielded a single component (Diefenbach & Mohamed, 2007). Cronbach's α for this study was 0.52. Urinary function was measured using three items from the American Urological Association symptom index (Barry et al., 1992). That is, ‘whether the patient had a sensation of his bladder not emptying completely after he finished urinating’, ‘whether frequent day time urination has been a problem’, and ‘whether frequent night time urination has been a problem’. Results of PCA in our earlier work (Diefenbach & Mohamed, 2007) indicated a single component. Accordingly, we combined the three items to construct a scale to assess urinary function. Cronbach's α for the present study was 0.80. Items were reverse coded so that higher scores had a positive valence. Note that all medical variables were measured at Time 1.
Statistical Analyses
Potential covariates were selected from sociodemographic and medical variables that had been found to be associated with adjustment and QOL in previous research (i.e., age, ethnicity/race, years of education, treatment type, time since diagnosis, sexual functioning and urinary functioning; Diefenbach & Mohamed, 2007; Rosenfeld, Roth, Gandhi, & Penson, 2004; Sanda et al., 2008). Bivariate correlations (or point biserial correlations for dichotomized variables) were then used to determine the sociodemographic and medical covariates that were significantly related to patient QOL at Time 2. The covariates used in all mediation analyses were patient age, patient sexual function, and patient QOL at Time 1.
Mediation analyses were conducted while adjusting for covariates (i.e., patient age, sexual function, and Time 1 QOL). We predicted that spouses’ beliefs about the timeline of their loved one's illness would mediate relations between spouses’ treatment control beliefs and patients’ QOL six months later. In parallel analyses, we also predicted that patients’ beliefs about the timeline of their illness would mediate relations between their treatment control beliefs and QOL six months later. To test mediation effects, we conducted mediation analyses using bootstrapping. This analysis provides estimates of the effect of an independent variable on a mediator (a path), the effect of a mediator on a dependent variable (b path), the direct effect of an independent variable on a dependent variable (c path) and then the indirect effect of an independent variable on a dependent variable whilst accounting for a mediator (c’ path). In Baron and Kenny's (1986) approach, certain statistical criteria must be met – i.e., the independent variable must be correlated with the dependent variable, the independent variable must be correlated with the mediator, the mediator must affect the dependent variable, and then if path c’ is closer to zero than c, the potential mediator is deemed to be a mediator of the relationship between X and Y. However, the causal steps approach has been heavily criticised for having very low statistical power to detect real mediation effects (Fritz & Mackinnon, 2007; MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). The a and b paths are mutually related so that a strong a path could limit the significance of the b path (Lundgren, Dahl, & Hayes, 2008).
Bootstrapping is a statistical method that involves repeatedly sampling from the data set to obtain multiple estimates of the indirect effect (i.e., the effect of the independent variable on the dependent variable through the mediator). Using this method, we were able to generate 5,000 bootstrapped samples. Point estimates and 95% bias corrected and accelerated confidence intervals for indirect and total effects were generated. Advantages to using this statistical approach to testing mediation effects compared to Baron and Kenny's (1986) causal steps approach include: (i) bootstrapping of the sampling distribution (a non-parametric approach to effect-size estimation and hypothesis testing) does not rely on the assumption of normal sampling distributions of the indirect effects; (ii) type II error is reduced because it requires fewer inferential tests; and (iii) multiple mediators can be tested at the same time (Preacher & Hayes, 2004). These analyses allowed for statistical control of covariates that were not proposed to be mediators of the total effect. Whereas inferential testing bases significant findings typically on p-values of less than 0.05, bootstrapping bases significant findings upon confidence intervals that do not contain zero.
Results
When participants who completed the Time 2 assessment (n = 53) were compared with participants who did not complete the Time 2 assessment (n = 69) on sociodemographic and pre-treatment symptom variables for which data were available, only one difference was noted. T-tests indicated that patients who completed the Time 2 assessment were more likely to report better urinary function at Time 1 (M = 4.34, SD = 0.72) than patients who did not complete the Time 2 assessment (M = 3.80, SD = 0.96; t[97] = 3.15, p = 0.002).
Bivariate correlations and descriptive data for study variables are shown in Table 2. Descriptive data analyses showed that both patients and spouses generally agreed that treatment would control the disease (patients M = 3.95, SD = 0.65; spouses M = 3.91, SD = 0.72), but did not expect either a short or a long disease timeline (patients M = 3.28, SD = 0.88; spouses M = 3.20, SD = 0.84).
Table 2.
Correlations among study variables (n = 53).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. Patient QOL T1 | — | 0.86*** | 0.15 | 0.20 | 0.15 | 0.09 | 0.39** | 0.41** |
| 2. Patient QOL T2 | — | 0.10 | 0.07 | 0.26 | 0.22 | 0.33* | 0.28* | |
| 3. Patient treatment control beliefs T1 | — | 0.40** | 0.33* | 0.24 | −0.29* | 0.37** | ||
| 4. Patient timeline beliefs T1 | — | 0.19 | 0.30* | −0.05 | 0.20 | |||
| 5. Spouse treatment control beliefs T1 | — | 0.35* | −0.12 | 0.12 | ||||
| 6. Spouse timeline beliefs T1 | — | −0.08 | 0.29* | |||||
| 7. Patient age (covariate) | — | −0.01 | ||||||
| 8. Sexual function T1 (covariate) | — | |||||||
| M | 98.08 | 93.82 | 3.95 | 3.28 | 3.91 | 3.20 | 64.02 | 3.13 |
| SD | 10.37 | 10.70 | 0.65 | 0.88 | 0.72 | 0.84 | 8.52 | 0.94 |
| Range | 50-108 | 46-108 | 2.67-5.00 | 1-5 | 2.33-5.00 | 1.67-5.00 | 42-83 | 1-5 |
Note
p ≤ 0.05
p ≤ 0.01
p ≤ 0.001
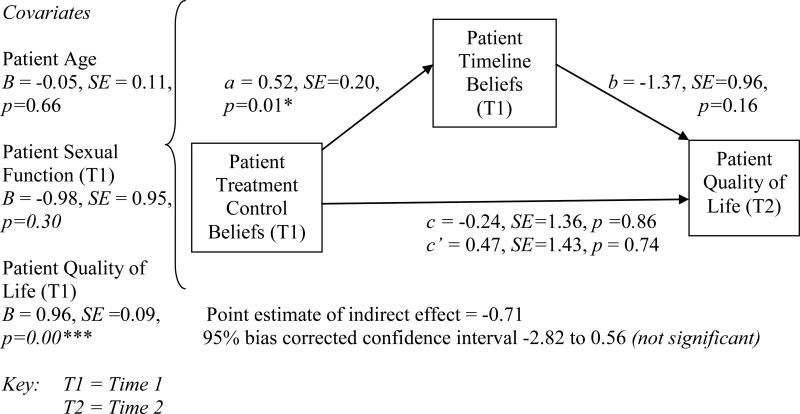
The mediation designs tested in the present study (using unstandardised coefficients) are depicted in Figures 1 and 2. We first examined the role of patients’ treatment control and timeline beliefs on patients’ QOL. In Figure 1, the total effect of patient treatment control beliefs at Time 1 on patients’ QOL at Time 2 (six months later) is represented by path c, and path c’ is the direct effect of patient treatment control beliefs on patients’ QOL after controlling for patient timeline beliefs. The indirect effect is exerted on patients’ QOL through the proposed mediator of patient timeline beliefs. After controlling for covariates (patient age, patient sexual functioning and patients’ QOL) at Time 1, results indicated that patient timeline beliefs did not mediate the effect of patient treatment control beliefs on patients’ QOL because the bias corrected and accelerated bootstrap confidence interval included zero. Note that the coefficients of the covariates presented are the partial regression weights for the covariates in the model of the outcome variable.
Figure 1. Mediation design with patient timeline beliefs as mediator.
Patient treatment control beliefs are hypothesised to exert indirect effects on patients’ QOL through patient timeline beliefs; *p ≤ 0.05; ***p ≤ 0.001.
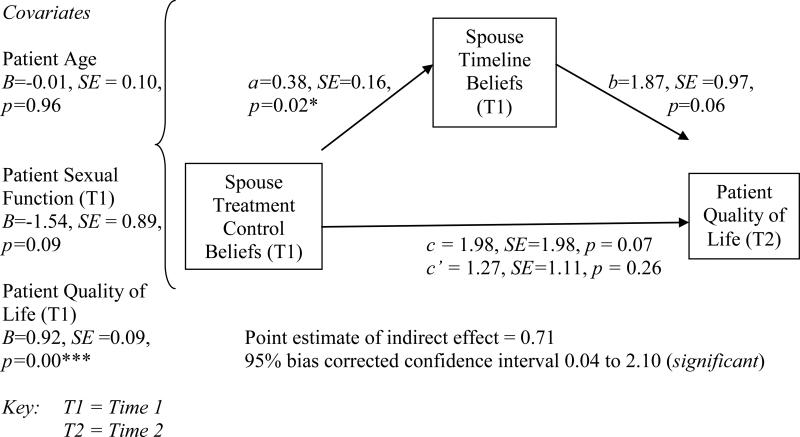
Figure 2. Mediation design with spouse timeline beliefs as mediator.
Spouse treatment control beliefs are hypothesised to exert indirect effects on patients’ QOL through spouse timeline beliefs; *p ≤ 0.05; ***p ≤ 0.001.
We then examined the role of spouses’ treatment control and timeline beliefs on patients’ QOL. In Figure 2, the total effect of spouse treatment control beliefs at Time 1 on patients’ QOL at Time 2 (six months later) is represented by path c, and path c’ is the direct effect of spouse treatment control beliefs on patients’ QOL after controlling for spouse timeline beliefs. The indirect effect is exerted on patients’ QOL through the proposed mediator of spouse timeline beliefs. After controlling for covariates (i.e., patient age, patient sexual functioning and patient urinary functioning at Time 1), patients’ QOL at Time 1 was found to be the most important predictor of their QOL 6 months later (p < 0.001). Results also indicated that spouse timeline beliefs mediated the effect of spouse treatment control beliefs on patients’ QOL, over and above the effect of patients’ QOL at Time 1 on QOL at Time 2, as evidenced by the bias corrected and accelerated bootstrap confidence interval, which did not include zero.
Discussion
This study examined associations among patients’ and spouses’ beliefs about treatment control and disease timeline and the patients’ QOL over a six-month period following localised PC treatment. Study results revealed significant mediation effects of spouses’ timeline beliefs on the association between spouses’ treatment control beliefs and patients’ QOL. No significant mediation effect of patients’ timeline beliefs on the association between patients’ treatment control beliefs and their QOL was found.
Descriptive data analyses showed that both patients and spouses generally agreed that the treatment would control the PC. There are two potential reasons for these outcomes. First, we included only patients with early stage, localised diseases in this study. Because treatment of localised PC is quite effective with an average 5-year survival rate of 95% regardless of type of treatment, it is likely that communication with the physician regarding the efficacy of PC treatment might have strengthened the patient's and spouse's beliefs about treatment control. Second, control beliefs, in general, among cancer patients and caregivers are important in understanding coping and adaptation to illness (Lobchuk, McPherson, McClement, & Cheang, 2011; Osowiecki & Compas, 1998; Taylor, Lichtman, & Wood, 1984). Therefore, and according to the self-regulation model, higher levels of treatment control beliefs might reflect ongoing adaptive coping responses to cancer and treatment among both patients and spouses (Cameron & Moss-Morris, 2006). With respect to the finding that both patients and their spouses expect neither a short nor a long disease timeline (suggesting that they believed the illness would be of moderate duration), there are likely to be variations in how patients understand ‘moderate’. In the absence of a clearer indication of what moderate means to them (e.g., a few months vs. weeks), we can only speculate at this stage. Future research would benefit from a more specific measurement of patients’ and spouses’ duration beliefs.
Results also indicated that patient timeline beliefs did not mediate the effect of patient treatment control beliefs on patient's QOL. Although illness perceptions have indeed predicted emotional QOL in a range of medical populations (Alsen et al., 2010; Covic et al., 2004; Tiemensma et al., 2011; Traeger et al., 2009), it is likely that the lack of significant mediation effect of timeline beliefs on associations between their treatment control beliefs and QOL six months later might be related to the strength of the association between initial QOL (Time 1) and QOL six months later (Time 2). In other words, regardless of patients’ illness beliefs, patients’ QOL (i.e., the composite of social/family, emotional, functional, and physical QOL) dominates illness beliefs as the most important predictor of their QOL at a later time point.
Unlike for patients, spouse timeline beliefs mediated the effect of spouse treatment control beliefs on patient's QOL at Time 2 even after controlling for their QOL at Time 1. Spouses experience their loved one's illness vicariously and, thus, their cognitions (i.e., beliefs) are likely to exert significant influence on patients’ adjustment. Patients of spouses who reported higher treatment control beliefs and, in turn, shorter expected disease timelines, were more likely to report better QOL at a later time point. In the stress and coping literature, Lazarus and Folkman (1984) state that the extent to which a stressful event is perceived as controllable, is important in influencing the number and type of coping responses that an individual will use. Indeed, there is reason to believe that caregiver expectations about the efficacy of treatment and, in turn, the timeline of their loved one's illness, may impact patient outcomes through adaptation processes and coping responses. Spouses are often the primary caregiver for cancer patients (Hodgkinson et al., 2007) and many patients also view their spouse as a partner in coping with cancer (Butler, Downe-Wamboldt, Marsh, Bell, & Jarvi, 2000). Learman and colleagues (Learman, Avorn, Everitt, & Rosenthal, 1990) noted a ‘Pygmalion effect’ in their research with nursing home patients and their caregivers. In their study, the clinical status of nursing home residents was found to be positively influenced by caregiver expectations, particularly emotional aspects of their well-being and the incidence of severe illness (though not their functional independence). There is reason to believe that a similar Pygmalion effect occurred with the PC patients in this study because spouses’ beliefs about treatment control (i.e., their expectations about the efficacy of treatment) and, in turn, the timeline of the disease, influenced patients’ general QOL following treatment. That is, spouses’ beliefs likely shaped interactions between the couple, reinforced daily life activities, and influenced coping behaviors that bolstered patients’ QOL.
One limitation of this study is that we did not specifically examine behavioural actions that arose from the illness beliefs under study. The analyses did, however, provide an indication of possible mechanisms that need to be explored in future studies. There are also limitations to the generalisability of the present findings. First, this sample focused exclusively on PC patients and their spouses. Men diagnosed with early-stage PC have better prognosis and treatment control relative to many other cancer patients (American Cancer Society, 2011). Thus, principles obtained from this research might not be applicable to other health conditions in which disease controllability might not be guaranteed. Second, the sample was largely Caucasian, well-educated, and middle-class. Therefore, it is not known to what extent the present findings would apply to patients and spouses of different ethnic backgrounds or socioeconomic status. Third, the representativeness of the sample may be further limited by selection bias, in that those who completed the study tended to report better urinary functioning than those who did not complete the study.
Conclusions and Future Directions
We have demonstrated evidence of a mediation effect of spouses’ timeline beliefs on the association between their treatment control beliefs and PC patients’ QOL. These findings highlight the powerful influence of spouses’ beliefs and expectations about treatment outcomes on patients’ QOL. Although this study provides us with valuable insights into the importance of involving spouses in psychological interventions focused upon improving patient's QOL, there is a great need for future research that focuses on understanding the interrelationships between patients’ and spouses’ illness beliefs (such as the similarity or dissimilarity of beliefs), how they might influence both patients’ and spouses’ QOL at different stages of the cancer experience (e.g., at diagnosis, during treatment, and after initial treatment), the mechanisms through which spouses’ beliefs impact patients’ QOL (e.g., behavioural/coping mechanisms), and whether there is a gender effect (e.g., Kim et al., 2008). In sum, this study highlights the important influence of spouses’ illness beliefs on patients’ QOL, and the need for more research and development of interventions in dyadic coping and patient adjustment. It also demonstrates the importance of accepting and including spouses as partners in the health care team and, thus, involving them in the disease and treatment consultation process.
Acknowledgements
We wish to thank Daniel Toulson, B.A. for his help in checking the final version of this manuscript. This research was supported by funding from the following sources: American Cancer Society: PF-12-041-01-CPPB; DAMD: 17-01-0006; Commonwealth of Pennsylvania: PADOH ME-98155; National Cancer Institute: R01CA118682 and National Cancer Institute: 2P01-CA057586-09A2.
References
- Alsen P, Brink E, Persson LO, Brandstrom Y, Karlson BW. Illness perceptions after myocardial infarction: relations to fatigue, emotional distress, and health-related quality of life. The Journal of Cardiovascular Nursing. 2010;25(2):E1–E10. doi: 10.1097/JCN.0b013e3181c6dcfd. doi:10.1097/JCN.0b013e3181c6dcfd. [DOI] [PubMed] [Google Scholar]
- American Cancer Society . Cancer Facts and Figures 2011. American Cancer Society; Atlanta: 2011. [Google Scholar]
- American Cancer Society [1 July 2012];Prostate cancer. 2012 Retrieved from http://www.cancer.org/acs/groups/cid/documents/webcontent/003134-pdf.pdf.
- American Urological Association [14 December 2011];Prostate cancer: Guideline for the management of clinical localized prostate cancer. 2007 update. 2007 Available at www.auanet.org/content/guidelines-and-quality-care/clinical-guidelines/main-reports/proscan07/content.pdf.
- Bailey DE, Jr, Wallace M, Mishel MH. Watching, waiting and uncertainty in prostate cancer. Journal of Clinical Nursing. 2007;16(4):734–741. doi: 10.1111/j.1365-2702.2005.01545.x. doi:10.1111/j.1365-2702.2005.01545.x. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barry MJ, Fowler FJ, Jr, O'Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, Cockett AT. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. The Journal of Urology. 1992;148(5):1549–57. doi: 10.1016/s0022-5347(17)36966-5. discussion 1564. [DOI] [PubMed] [Google Scholar]
- Butler L, Downe-Wamboldt B, Marsh S, Bell D, Jarvi K. Behind the scenes: partners' perceptions of quality of life post radical prostatectomy. Urologic Nursing. 2000;20(4):254–258. [PubMed] [Google Scholar]
- Butler LD, Field NP, Busch AL, Seplaki JE, Hastings TA, Spiegel D. Anticipating loss and other temporal stressors predict traumatic stress symptoms among partners of metastatic/recurrent breast cancer patients. Psycho-Oncology. 2005;14(6):492–502. doi: 10.1002/pon.865. doi:10.1002/pon.865. [DOI] [PubMed] [Google Scholar]
- Cameron LD, Moss-Morris R. Illness-related cognition and behaviour. In: Kaptein A, Weinman J, editors. Health Psychology. Blackwell Publishers; Oxford, UK: 2006. pp. 84–110. [Google Scholar]
- Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, Brannon J. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. Journal of Clinical Oncology : Official Journal of the American Society of Clinical Oncology. 1993;11(3):570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- Covic A, Seica A, Gusbeth-Tatomir P, Gavrilovici O, Goldsmith DJ. Illness representations and quality of life scores in haemodialysis patients. Nephrology, Dialysis, Transplantation : Official Publication of the European Dialysis and Transplant Association - European Renal Association. 2004;19(8):2078–2083. doi: 10.1093/ndt/gfh254. doi:10.1093/ndt/gfh254. [DOI] [PubMed] [Google Scholar]
- Diefenbach MA, Mohamed NE. Regret of treatment decision and its association with disease-specific quality of life following prostate cancer treatment. Cancer Investigation. 2007;25(6):449–457. doi: 10.1080/07357900701359460. doi:10.1080/07357900701359460. [DOI] [PubMed] [Google Scholar]
- Dunn MW, Kazer MW. Prostate cancer overview. Seminars in Oncology Nursing. 2011;27(4):241–250. doi: 10.1016/j.soncn.2011.07.002. doi:10.1016/j.soncn.2011.07.002. [DOI] [PubMed] [Google Scholar]
- Epstein S. The self-concept revisited. Or a theory of a theory. The American Psychologist. 1973;28(5):404–416. doi: 10.1037/h0034679. [DOI] [PubMed] [Google Scholar]
- Fritz MS, Mackinnon DP. Required sample size to detect the mediated effect. Psychological Science. 2007;18(3):233–239. doi: 10.1111/j.1467-9280.2007.01882.x. doi:10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galbraith ME, Ramirez JM, Pedro LW. Quality of life, health outcomes, and identity for patients with prostate cancer in five different treatment groups. Oncology Nursing Forum. 2001;28(3):551–560. [PubMed] [Google Scholar]
- Griva K, Jayasena D, Davenport A, Harrison M, Newman SP. Illness and treatment cognitions and health related quality of life in end stage renal disease. British Journal of Health Psychology. 2009;14(Pt 1):17–34. doi: 10.1348/135910708X292355. doi:10.1348/135910708X292355. [DOI] [PubMed] [Google Scholar]
- Hedestig O, Sandman PO, Widmark A. Living with untreated localized prostate cancer: a qualitative analysis of patient narratives. Cancer Nursing. 2003;26(1):55–60. doi: 10.1097/00002820-200302000-00008. [DOI] [PubMed] [Google Scholar]
- Hodgkinson K, Butow P, Hunt GE, Wyse R, Hobbs KM, Wain G. Life after cancer: couples' and partners' psychological adjustment and supportive care needs. Supportive Care in Cancer : Official Journal of the Multinational Association of Supportive Care in Cancer. 2007;15(4):405–415. doi: 10.1007/s00520-006-0148-0. doi:10.1007/s00520-006-0148-0. [DOI] [PubMed] [Google Scholar]
- Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Waldron W, Edwards BK. SEER Cancer Statistics Review, 1975-2008. 2011 Retrieved from http://seer.cancer.gov/csr/1975_2008/
- Janoff-Bulman R. Shattered assumptions: Towards a new psychology of trauma. Free Press; New York: 1992. [Google Scholar]
- Jim HS, Jacobsen PB. Posttraumatic stress and posttraumatic growth in cancer survivorship: a review. Cancer Journal (Sudbury, Mass.) 2008;14(6):414–419. doi: 10.1097/PPO.0b013e31818d8963. doi:10.1097/PPO.0b013e31818d8963. [DOI] [PubMed] [Google Scholar]
- Kangas M, Henry JL, Bryant RA. Posttraumatic stress disorder following cancer. A conceptual and empirical review. Clinical Psychology Review. 2002;22(4):499–524. doi: 10.1016/s0272-7358(01)00118-0. [DOI] [PubMed] [Google Scholar]
- Karademas EC, Zarogiannos A, Karamvakalis N. Cardiac patient-spouse dissimilarities in illness perception: Associations with patient self-rated health and coping strategies. Psychology & Health. 2010;25(4):451–463. doi: 10.1080/08870440802652089. doi:10.1080/08870440802652089. [DOI] [PubMed] [Google Scholar]
- Kim Y, Kashy DA, Wellisch DK, Spillers RL, Kaw CK, Smith TG. Quality of life of couples dealing with cancer: dyadic and individual adjustment among breast and prostate cancer survivors and their spousal caregivers. Annals of Behavioral Medicine : A Publication of the Society of Behavioral Medicine. 2008;35(2):230–238. doi: 10.1007/s12160-008-9026-y. doi:10.1007/s12160-008-9026-y. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer; New York: 1984. [Google Scholar]
- Learman LA, Avorn J, Everitt DE, Rosenthal R. Pygmalion in the nursing home. The effects of caregiver expectations on patient outcomes. Journal of the American Geriatrics Society. 1990;38(7):797–803. doi: 10.1111/j.1532-5415.1990.tb01472.x. [DOI] [PubMed] [Google Scholar]
- Leventhal H, Brissette I, Leventhal EA. The common-sense model of self-regulation of health and illness. In: Cameron LD, Leventhal H, editors. The Self-Regulation of Health and Illness Behaviour. Routledge; London: 2003. pp. 42–65. [Google Scholar]
- Leventhal H, Nerenz DR, Steele DJ. Illness representations and coping with health threats. In: Baum A, Taylor SE, Singer DJ, editors. Handbook of psychology and health: Social psychological aspects of health. Erlbaum; Hillsdale, NJ: 1984. pp. 219–252. [Google Scholar]
- Lobchuk MM, McPherson CJ, McClement SE, Cheang M. A comparison of patient and family caregiver prospective control over lung cancer. Journal of Advanced Nursing. 2011 doi: 10.1111/j.1365-2648.2011.05819.x. doi:10.1111/j.1365-2648.2011.05819.x; 10.1111/j.1365-2648.2011.05819.x. [DOI] [PubMed] [Google Scholar]
- Lundgren T, Dahl J, Hayes SC. Evaluation of mediators of change in the treatment of epilepsy with acceptance and commitment therapy. Journal of Behavioral Medicine. 2008;31(3):225–235. doi: 10.1007/s10865-008-9151-x. doi:10.1007/s10865-008-9151-x. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merz EL, Malcarne VL, Ko CM, Sadler M, Kwack L, Varni JW, Sadler GR. Dyadic concordance among prostate cancer patients and their partners and health-related quality of life: does it matter? Psychology & Health. 2011;26(6):651–666. doi: 10.1080/08870441003721251. doi:10.1080/08870441003721251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss-Morris R, Weinman J, Petrie KJ, Horne R, Cameron LD, Buick D. The revised illness perception questionnaire (IPQ-R). Psychology & Health. 2002;17(1):1–16. [Google Scholar]
- Osowiecki D, Compas BE. Psychological adjustment to cancer: Control beliefs and coping in adult cancer patients. Cogn Ther Res. 1998;22(5):483–499. [Google Scholar]
- Parkes CM. Psycho-social transitions: a field for study. Social Science & Medicine. 1971;5(2):101–115. doi: 10.1016/0037-7856(71)90091-6. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers : A Journal of the Psychonomic Society, Inc. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Rosenfeld B, Roth AJ, Gandhi S, Penson D. Differences in health-related quality of life of prostate cancer patients based on stage of cancer. Psycho-Oncology. 2004;13(11):800–807. doi: 10.1002/pon.797. doi:10.1002/pon.797. [DOI] [PubMed] [Google Scholar]
- Rozema H, Vollink T, Lechner L. The role of illness representations in coping and health of patients treated for breast cancer. Psycho-Oncology. 2009;18(8):849–857. doi: 10.1002/pon.1488. doi:10.1002/pon.1488. [DOI] [PubMed] [Google Scholar]
- Sanda MG, Dunn RL, Michalski J, Sandler HM, Northouse L, Hembroff L, Wei JT. Quality of life and satisfaction with outcome among prostate-cancer survivors. The New England Journal of Medicine. 2008;358(12):1250–1261. doi: 10.1056/NEJMoa074311. doi:10.1056/NEJMoa074311. [DOI] [PubMed] [Google Scholar]
- Scharloo M, Baatenburg de Jong RJ, Langeveld TP, van Velzen-Verkaik E, Doorn-Op den Akker MM, Kaptein AA. Illness cognitions in head and neck squamous cell carcinoma: predicting quality of life outcome. Supportive Care in Cancer : Official Journal of the Multinational Association of Supportive Care in Cancer. 2010;18(9):1137–1145. doi: 10.1007/s00520-009-0728-x. doi:10.1007/s00520-009-0728-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah P, Hull T, Riley GA. Associations between the Illness Perception Questionnaire for Schizophrenia and engagement in treatment in a secure setting. Clinical Psychologist. 2009;13(2):69–74. doi: http://dx.doi.org/10.1080/13284200902849450. [Google Scholar]
- Siegel K, Raveis VH, Mor V, Houts P. The relationship of spousal caregiver burden to patient disease and treatment-related conditions. Annals of Oncology : Official Journal of the European Society for Medical Oncology / ESMO. 1991;2(7):511–516. doi: 10.1093/oxfordjournals.annonc.a058005. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Lichtman RR, Wood JV. Attributions, beliefs about control, and adjustment to breast cancer. Journal of Personality and Social Psychology. 1984;46(3):489–502. doi: 10.1037//0022-3514.46.3.489. [DOI] [PubMed] [Google Scholar]
- Thompson I, Thrasher JB, Aus G, Burnett AL, Canby-Hagino ED, Cookson MS, AUA Prostate Cancer Clinical Guideline Update Panel Guideline for the management of clinically localized prostate cancer: 2007 update. J.Urol. 2007;177(6):2106–2131. doi: 10.1016/j.juro.2007.03.003. [DOI] [PubMed] [Google Scholar]
- Tiemensma J, Kaptein AA, Pereira AM, Smit JW, Romijn JA, Biermasz NR. Negative illness perceptions are associated with impaired quality of life in patients after long-term remission of Cushing's syndrome. European Journal of Endocrinology / European Federation of Endocrine Societies. 2011 doi: 10.1530/EJE-11-0307. doi:10.1530/EJE-11-0307. [DOI] [PubMed] [Google Scholar]
- Traeger L, Penedo FJ, Gonzalez JS, Dahn JR, Lechner SC, Schneiderman N, Antoni MH. Illness perceptions and emotional well-being in men treated for localized prostate cancer. Journal of Psychosomatic Research. 2009;67(5):389–397. doi: 10.1016/j.jpsychores.2009.03.013. doi:10.1016/j.jpsychores.2009.03.013. [DOI] [PubMed] [Google Scholar]
- Wallace M. Uncertainty and quality of life of older men who undergo watchful waiting for prostate cancer. Oncology Nursing Forum. 2003;30(2):303–309. doi: 10.1188/03.onf.303-309. doi:10.1188/03.ONF.291-300. [DOI] [PubMed] [Google Scholar]
- Waterhouse J, Metcalfe MC. Development of the sexual adjustment questionnaire. Oncology Nursing Forum. 1986;13(3):53–59. [PubMed] [Google Scholar]