Abstract
Objectives
We estimated the informal caregiving hours and costs associated with stroke.
Methods
We selected persons aged 65 and older in 2006 and who were also included in the 2008 follow-up survey from the Health and Retirement Study. We adapted the case-control study design by using self-reported occurrence of an initial stroke event during 2006 and 2008 to classify persons into the stroke (case) and the non-stroke (control) groups. We compared informal caregiving hours between case and control groups in 2006 (pre-stroke period for case group) and in 2008 (post-stroke period for case group) and estimated incremental informal caregiving hours attributable to stroke by applying a difference-in-differences technique to propensity-score matched populations. We used a replacement approach to estimate the economic value of informal caregiving.
Results
The weekly incremental informal caregiving hours attributable to stroke were 8.5 hours per patient. The economic value of informal caregiving per stroke survivor was $8,211 per year, of which $4,356 (53%) was attributable to stroke. At the national level, the annual economic burden of informal caregiving associated with stroke among elderly was estimated at $14.2 billion in 2008.
Conclusions
Recent changes in public health and social support policies recognize the economic burden of informal caregiving. Our estimates reinforce the high economic burden of stroke in the US and provide up-to-date information for policy development and decision-making.
Keywords: Cost effectiveness/economics, All Cerebrovascular disease/Stroke, All rehabilitation
1. Introduction
Post-stroke morbidity often requires a substantial amount of informal caregiving1. Informal caregiving for stroke survivors is one of the largest cost components for stroke2, 3. However, only one study investigated the cost of informal caregiving related to stroke in the U.S. using 1990’s data4 and only one cost-of-illness study of stroke in the U.S. has included informal caregiving cost2.
An issue in estimating the cost of stroke-related informal caregiving is determining informal caregiving needs which are the direct and exclusive result of stroke and not due to age-related disability or other chronic health conditions. Two approaches were used to resolve this issue. In the first approach, the informal caregiving cost was estimated by comparing “pre-stroke” and “post-stroke” periods5–7 for those who developed stroke, and attributing to stroke all of the difference in informal caregiving costs. A second approach compared “stroke” and “non-stroke” groups4 and assumed that if stroke had not occurred, informal caregiving time for those in the stroke group would have been identical to those in the non-stroke group. However, both approaches may result in overestimates because informal caregiving needs may increase over time due to aging and other illnesses, and those in a stroke group may have used more informal caregiving before stroke.
We examined the stroke-related informal caregiving time and cost for the elderly in the U.S. We used a difference-in-differences (DID) method to combine the “pre-” and “post-” approach and the “stroke” vs. “non-stroke” comparisons, thus eliminating the overestimation issue from both approaches.
2. Materials and Methods
Data
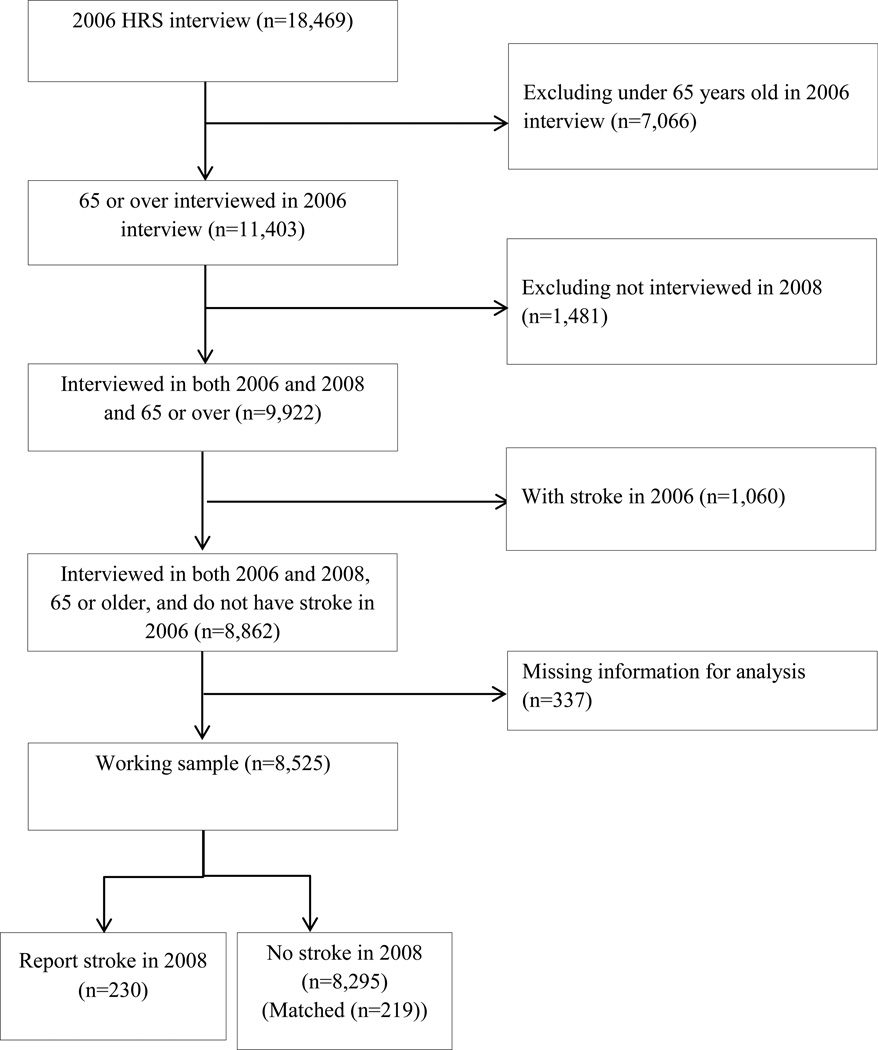
We used the 2006 and 2008 Health and Retirement Study (HRS) data8, including informal caregiving surveys, along with the RAND HRS version L9. The HRS is a biennial, nationally representative, longitudinal household survey initiated in 1992 for those who were near or past retirement age in the U.S. Many studies about informal caregiving burden have used these data.4, 10–17. The RAND Corporation produces RAND HRS data, a cleaned version of selected information from all available waves of the HRS data since 1992. We limited our study sample to those who were 65 and older in 2006 and who participated in both 2006 and 2008 interviews (Figure 1).
Figure 1.
Study design for case inclusion
Informal Caregivers
For this study, informal caregiving is defined as caregiving activities by relatives or unpaid non-relatives not in an organization18 to help a recipient complete their activities of daily living (ADLs) or instrumental activities of daily living (IADLs). We used a sequence of questions from the HRS to verify whether a respondent receives any informal caregiving. The first-level questions determined whether a respondent has difficulties with ADLs or IADLs due to a health or memory problem19. If so, respondents were asked whether a caregiver ever helped them to do these activities. Those who reported caregivers were asked additional questions about their relationship with each caregiver. In addition, HRS queries the respondent about the payment status of each caregiver except spouse/partner of a patient and an employee of an “institution”. We assumed that spouse/partner is an informal caregiver and an employee of an “institution” is a formal caregiver.
Weekly Informal Caregiving Hours
Our main outcome measures are weekly informal caregiving hours and cost associated with these hours. Hours are defined as caregiving hours provided by informal caregivers, reported by respondents as the number of hours per day and days during the preceding month that informal caregiving was received. For respondents with multiple informal caregivers, we calculated a weekly sum but limited to 16 hours the daily maximum number of hours of informal caregiving per informal caregiver4. We divided days per month by 4.3 to obtain a weekly average; and for respondents who needed help every day, we assumed 7 days per week.
Defining Stroke and Non-Stroke Groups
The longitudinal structure of the data set allowed us to identify stroke survivors with a first-ever-lifetime stroke between 2006 and 2008 by comparing self-reported stroke status in 2006 and 2008. The stroke status question in the HRS interview is: “Has a doctor ever told you that you had a stroke?” Respondents who completed a prior HRS interview were shown the answer they gave in that interview and then asked to update their stroke status in the current HRS interview. Stroke cases were defined as those who reported stroke in the 2008 survey and no stroke in the 2006. Participants who reported stroke in 2006 were excluded from the study (Figure 1). Further match was conducted between stroke and no-stroke groups.
Difference-in-Differences (DID) Approach
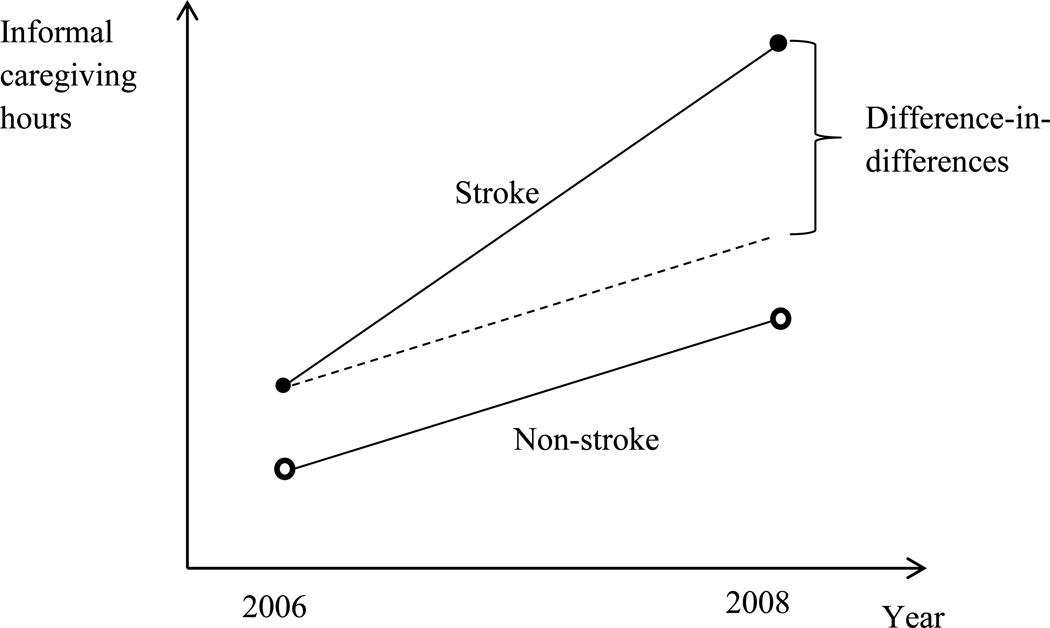
We applied a DID approach20, 21 to estimate the incremental informal caregiving hours due to stroke. The DID approach estimates the difference in informal caregiving hours between the stroke group and the non-stroke group in 2008, while adjusting for differences in informal caregiving hours between the 2 groups in 2006 (Figure 2). We assumed that if the stroke group had not had a stroke, the difference of informal caregiving hours between the stroke group and the non-stroke group in 2008 would be the same difference as it was in 200621.
Figure 2.
Difference-in-Differences approach
Stroke: Patients with first-ever stroke between year 2006 and 2008 based on self-report Non-Stroke: Those who reported never has been diagnosed as stroke before Difference-in-differences: Additional informal caregiving hours associated with stroke
The difference in socio-demographic characteristics and health conditions between two groups may lead to bias in estimating differences in usage of informal caregiving due to stroke. For instance, suppose that informal caregiving needs increase with faster pace over time among those who have large numbers of chronic diseases compared with those who have small numbers of chronic diseases. Those who are in non-stroke group were less likely to have chronic diseases and less likely to use informal caregiving in 2006 than those who are in stroke group. Then, in addition to stroke onset between 2006 and 2008, initial chronic conditions among stroke group cause the additional increase of informal caregiving hours compared with non-stroke group. To minimize potential biases, we derived matching samples by using the Mahalanobis propensity-score matching method22, 23.
We chose socio-demographic and economic characteristics, which has been commonly used as matching variables23, 24, and chronic diseases, number of ADLs and IADLs impaired, which has been known as having high impact on informal caregiving burden10, 12, 14, 15, 18 as matching variables. The matching variables we used were race; gender; education; marital status; age dummies; total non-housing household wealth; dummy variables for the following chronic conditions: diabetes, cancer, lung disease, heart problems (including heart attack, coronary heart disease, angina, congestive heart failure, or other heart problems), hypertension, psychiatric problem, and arthritis; a dummy variable to indicate whether a respondent reported any helpers for ADLs or IADLs due to health or memory problems or not; dummy variables of number of ADLs impaired; and dummy variables of number of IADLs impaired in 2006—a time when neither group reported stroke (Table 1). Since both groups with matched samples had similar characteristics in 2006, we assumed that any differences between the two groups in 2008 were caused by stroke. We used commands of –psmatch2– and –diff– from STATA 12.0 (StataCorp, College Station, TX) for the propensity score matching and the DID estimation, respectively25, 26.
Table 1.
Sample Characteristics by Stroke Status from the 2006 Samples Aged 65 and Over after Matching (%)
| Stroke Between 2006 & 2008 N=230 |
Non-Stroke N=219 |
p-Value | ||
|---|---|---|---|---|
| Race: | Non-Latino white | 80.4 | 82.6 | 0.565 |
| African-American | 14.3 | 13.0 | 0.700 | |
| Latino | 3.9 | 3.0 | 0.612 | |
| Other Race/ethnicity | 1.3 | 1.3 | 1.000 | |
| Gender: Male | 40.0 | 37.0 | 0.511 | |
| Age | 65–74 | 39.6 | 43.5 | 0.409 |
| 75–84 | 41.7 | 38.3 | 0.458 | |
| 85 & over | 18.7 | 18.3 | 0.907 | |
| Currently Married | 50.9 | 48.3 | 0.586 | |
| Education: | Less than high school | 34.8 | 35.7 | 0.850 |
| High school graduate | 36.5 | 37.0 | 0.925 | |
| Some college | 14.8 | 15.2 | 0.897 | |
| College & more | 13.9 | 12.2 | 0.587 | |
| Non-housing wealth ($ thousand) | 313 | 250 | 0.396 | |
| Census area: Northeast | 16.5 | 14.8 | 0.610 | |
| Midwest | 24.8 | 23.9 | 0.832 | |
| South | 39.1 | 42.6 | 0.463 | |
| West | 19.6 | 18.7 | 0.817 | |
| Chronic disease: Diabetes | 25.7 | 24.3 | 0.755 | |
| Cancer | 15.7 | 12.2 | 0.283 | |
| Lung disease | 13.9 | 11.3 | 0.434 | |
| Heart problems | 37.4 | 35.7 | 0.709 | |
| Hypertension | 68.7 | 71.7 | 0.485 | |
| Psychiatric problems | 20.4 | 17.8 | 0.492 | |
| Arthritis | 76.5 | 77.4 | 0.828 | |
| Use of caregiving | 27.4 | 27.8 | 0.922 | |
| No. of ADLs impaired: 0 | 66.5 | 67.0 | 0.925 | |
| 1~3 | 28.3 | 27.8 | 0.920 | |
| 4~6 | 5.2 | 5.2 | 1.000 | |
| No. of IADLs impaired: 0 | 70.4 | 70.4 | 1.000 | |
| 1~3 | 25.7 | 25.7 | 1.000 | |
| 4~5 | 3.9 | 3.9 | 1.000 | |
Notes: All estimates are weighted.
Cost Estimation
We estimated the economic value associated with informal caregiving using a replacement approach which assumes that informal caregiving activities substitute activities of (formal) paid workers4, 5. We used the median wage of home health aide workers ($9.84/hour) from the 2008 U.S. Bureau of Labor Statistics as the cost of an hour for informal caregiving4 and conducted sensitivity analyses using the 10th percentile ($7.65/hour) and the 90th percentile ($13.93/hour). We used our DID estimator to calculate incremental informal caregiving cost due to stroke as we did for incremental informal caregiving hours. The U.S. Census estimates that the U.S. population aged 65 years and older was 38,869,716 in July 1, 2008; and the prevalence of stroke in this age group in the US was 8.4 percent in 200827. Based on this, we estimated the number of stroke survivors in 2008 was 3,265,056 people. Annual national costs for informal caregiving were calculated by multiplying the weekly per patient informal caregiving cost, the number of stroke survivors, and 52 weeks.
3. Results
Among 8,525 study subjects, 230 had a new onset of stroke between 2006 and 2008. Before propensity-score matching, the stroke group (n = 230) and the non-stroke group (n = 8,295) differed significantly in all the socio-demographic characteristics such as race, age, marital status, education, self-reported chronic conditions, and ADL or IADL difficulties (Table e-1). Compared with people who never had stroke, those who had stroke between 2006 and 2008 were older, less likely to have additional education beyond high school, more likely to report chronic disease, less likely to report ADL or IADL difficulties, less likely to be currently married, and less likely to be Latino than the non-stroke group. After propensity score matching, we did not observe any significant differences in these characteristics between the stroke group (n = 230) and the non-stroke group (n = 219) (Table 1).
Table 2 shows the proportion of persons who reported having difficulties in each ADL and IADL from the matched stroke and non-stroke groups in 2006 and 2008. In 2006, the two groups were not significantly different in ADLs and IADLs. The 2008 data show that a stroke survivor was more likely to report problems in every ADL and IADL than a person in the non-stroke group.
Table 2.
Proportion of participants reporting difficulties in ADLs and IADLs by stroke status in 2006 and 2008 (%)
| 2006 (Pre-stroke period for the stroke group) |
2008 (Post-stroke period for the stroke group) |
|||||
|---|---|---|---|---|---|---|
| Stroke between 2006 & 2008 N=230 |
non- Stroke N=219 |
p-Value | Stroke between 2006 & 2008 N=230 |
non- Stroke N=219 |
p-Value | |
| Number of problems in ADLs | ||||||
| 0 | 67.0 | 66.5 | 0.925 | 52.2 | 65.2 | 0.006 |
| 1~3 | 28.3 | 27.8 | 0.920 | 25.7 | 27.8 | 0.618 |
| 4~6 | 5.2 | 5.2 | 1.000 | 22.2 | 7.0 | <0.001 |
| ADLs with difficulties | ||||||
| Bathing | 12.6 | 11.7 | 0.794 | 33.9 | 15.7 | <0.001 |
| Dressing | 15.7 | 20.4 | 0.218 | 31.7 | 19.1 | 0.003 |
| Eat | 5.2 | 7.4 | 0.404 | 18.7 | 9.6 | 0.006 |
| Getting in and out of bed | 7.0 | 9.6 | 0.362 | 23.5 | 10.9 | <0.001 |
| Walking across a room | 14.3 | 12.2 | 0.532 | 30.0 | 16.1 | <0.001 |
| Using a toilet | 13.0 | 11.3 | 0.612 | 23.0 | 10.0 | <0.001 |
| Number of problems in IADLs | ||||||
| 0 | 70.4 | 70.4 | 1.000 | 47.8 | 67.4 | <0.001 |
| 1~3 | 25.7 | 25.7 | 1.000 | 30.9 | 27.0 | 0.380 |
| 4~5 | 3.9 | 3.9 | 1.000 | 21.3 | 5.7 | <0.001 |
| IADLs with difficulties | ||||||
| Using a phone | 11.3 | 9.1 | 0.460 | 26.1 | 11.7 | <0.001 |
| Managing Money | 13.0 | 8.3 | 0.116 | 30.9 | 12.2 | <0.001 |
| Taking Medication | 6.1 | 6.5 | 0.865 | 19.6 | 8.3 | <0.001 |
| Shopping for groceries | 18.3 | 20.4 | 0.585 | 38.7 | 19.6 | <0.001 |
| Preparing hot meals | 10.9 | 11.7 | 0.792 | 33.0 | 14.8 | <0.001 |
Notes: All estimates are weighted.
Table 3 shows the DID estimators from informal caregiving hours and costs. In 2006, the stroke group used an average of 6.8 hours of informal caregiving per week while the non-stroke group used an average of weekly 3.6 hours per person. The stroke group used 3.2 hours more informal caregiving per week than the non-stroke group in 2006, but the difference was not statistically significant. We assumed that if the stroke group had not had a stroke, they still used 3.2 hours more informal caregiving per week than the non-stroke group in 2008. In 2008, a stroke survivor used 16.1 hours of informal caregiving per week when a non-stroke counterpart used 4.4 hours, a difference of 11.7 hours. After subtracting baseline difference in 2006 (3.2 hours) from the difference of informal caregiving hours in 2008 (11.7 hours) for adjustment, the DID estimator shows that the need for an additional 8.5 hours informal caregiving per week (p < 0.01) could be attributable to stroke.
Table 3.
Stroke-related informal care burden among U.S. elderly population
| Weekly average informal care hours | Annual average informal care cost ($2008) | |||||
|---|---|---|---|---|---|---|
| Stroke between 2006 & 2008 (A) |
Non-stroke (B) |
A–B | Stroke between 2006 & 2008 (C) |
Non-stroke (D) |
C–D | |
| 2006 (Pre-stroke period for the stroke group) | 6.8** (1.6) | 3.6** (1.0) | 3.2 (1.8) | 3,477** (794) | 1,855** (493) | 1,622 (935) |
| 2008 (Post-stroke period for the stroke group) | 16.1** (2.3) | 4.4** (1.1) | 11.7** (2.6) | 8,211** (1,201) | 2,233** (582) | 5,978** (1,334) |
| Stroke associated burden from a difference-in-differences approach | - | - | 8.5** (3.2) | - | - | 4,356** (1,630) |
Notes:
p < 0.01. Standard errors are in parentheses. All estimates are weighted.
Using the median wage of home health aid workers in 2008 ($9.84/hour), we estimated that a person who never experienced stroke spent $2,233 for informal caregiving in 2008 while a stroke patient spent on average $8,211, a difference of $5,978 (Table 3). Using the DID estimator we then adjusted the costs to reflect baseline differences in informal caregiving use between the stroke and non-stroke group in 2006 ($1,622), and estimated that stroke-related informal caregiving costs in 2008 were $4,356 per patient (Table 3). Applying our results to the U.S. population of stroke patients 65 years and over in 2008 using the number of stroke patient derived from the methods section (n = 3,265,056), we estimated that informal caregiving costs for stroke patients were $26.8 billion per year ($8,211 per year per patient×3,265,056 stroke patients), and the portion attributable to stroke was 53 percentage of the cost or $14.2 billion ($4,356 per year per patient). The estimated range of additional cost attributable to stroke by using the 10th and the 90th percentiles of home health aide wages are from $11.1 billion to $20.1 billion per year.
4. Discussion
We used the DID method and a nationally representative sample to estimate the informal caregiving cost of stroke survivors in the U.S. Our estimates reinforced the high economic burden of stroke in the U.S. and are consistent with the results from previous studies. A previous study of U.S. adults over 70 years old reported that those with stroke-related health problems used an additional 12.5 hours of weekly informal caregiving compared with those who never had a stroke; and those who had stroke without stroke-related health problems needed less—an additional 2.5 hours per week4. Using those findings, Brown and colleagues estimated the average annual informal caregiving cost as $4,038 per ischemic stroke patient in 2005 dollars2. Several technological and pharmacological advances have been made in the treatment of stroke during the last 15 years which we suspected might reduce the informal caregiving burden, but our estimation with 2008 data ($4,356) is surprisingly similar to the estimation based on 1993 data ($4,038).
Compared with non-U.S. studies about stroke, we found that stroke survivors in other countries used more informal caregiving hours than stroke survivors in the U.S. A study in Thailand showed an average 94.6 hours per month informal caregiving hours among stroke survivors in 20067; and a study in the Netherlands showed an average of 20.2 hours per week in 20016.
Studies with recent data such as ours provide policy makers with up-to-date information that can inform policy development and decision-making. For instance, a change in Medicare policy to reduce costs by restricting reimbursements to paid home health care resulted in a shift of part of the caregiving burden from formal to informal caregiving as well as the expected decreases in Medicare payments28. Then, the high burden of informal caregiving is recognized by the National Family Caregiver Support Program (NFCSP) that provides informal caregivers with training, counseling, and respite services; by employment policies, such as the Family and Medical Leave Act; and by state-level polices that provide tax credits to informal caregivers17, 29. Recent new technologies (e.g., telemedicine, and tissue plasminogen activator (t-PA)) and changes in policies to improve stroke outcomes (e.g., cross-jurisdiction policies for telemedicine, and medical licensure policies for administration of t-PA) which have the potential to affect informal caregiving burden also underscore the need for studies such as ours that use the most recent national data.
Another notable strength of our study is the DID estimate, which provides more accurate estimates, compared with other methods, because of its uniqueness of considering both pre- and post- stroke period differences, as well as the stroke group and the non-stroke group differences. We could use this method because of the longitudinal structure of the HRS. We minimized the sample selection bias between stroke and non-stroke group using extensive socioeconomic and demographic variables available in the HRS.
There are some limitations, which may make our estimates conservative. First, our samples were limited to those who participated in both the 2006 and 2008 interviews. This may underestimate the burden of informal caregiving if 2006 participants’ lack of participation in the 2008 survey was due to more severe health conditions that precluded their participation. Next, we used people aged 65 or older because of data limitation, and thus we provide only a partial picture of the costs of informal caregiving associated with stroke. The informal caregiving burden of stroke survivors under 65 years old is an important future research area. Population trends show an increased incidence of stroke in younger populations30; these patients may require informal caregiving for longer periods than the elderly population does. Also, our cost estimates are limited to the economic value of caregiving hours and do not value intangible costs such as informal caregivers’ emotional stress or deterioration of physical health. Because of the survey structure, the informal caregivers were limited to those who provided help for ADL or IADL. The informal caregiving burden to those who provided help for other activities, such as household chores, social visits, psychological support, and exercise could not be included in this study4, 13.
Next, we were focused on the effect of the new onset of stroke; the effect of recurrent stroke on informal caregiving cost has not yet been investigated. Because the numbers of new onset are small, the representativeness of sample with respect to severity of stroke is unclear. Because sample size is too small for racial/ethnic minorities, we could not further investigate racial/ethnic issues. However, it will be an important topic for investigation since African-American and Hispanics are more likely to use informal caregiving than non-Hispanic whites in general.31, 32
Another limitation is a potential bias associated with the self-reported data. Self-report of stroke may cause exclusion of extreme cases and under- or over-estimation of informal caregiving associated with stroke by losing generalizability of sample. For instance, patients with extremely mild stroke may not self-report stroke because they did not recognize it. However, we expect that the impact of extremely severe cases is small because of high mortality rate. Also, patients with stroke and cognitive impairment might misreport their stroke status. We expect that the misreporting bias is not severe because the HRS did proxy interview to prevent the issue. Self-report informal caregiving hours may depend on socio-demographic characteristics and may lead biased estimates. The issue has not been fully investigated yet, but the self-report bias could be minimized in this study because of propensity score matching.
Finally, to apply DID method, we assumed that the difference of informal caregiving hours in the baseline year is consistent over time and there was no interaction between pre- and post- periods’ informal caregiving hours. When these assumptions are invalid, the estimations could be biased. There could be non-stroke factors, such as injuries from falling, which increase the caregiving needs but which occurred unequally between stroke and non-stroke groups during the post-stroke period. It may lead to our estimate being less conservative, but still the burden is partly associated with stroke since stroke increase the probability of having non-stroke factors. Propensity score matching reduced the potential bias caused by different characteristics between stroke and non-stroke groups at the pre-stroke period.
Despite these limitations, our study derived a reasonable estimate of the cost of informal caregiving for stroke survivors. Public health decision makers can consider this cost when they assess the total economic burden of stroke, set public health priorities, and allocate resources for stroke prevention. The cost information presented here can also be incorporated into public health program evaluations, especially those that examine the cost-effectiveness or comparative-effectiveness of stroke prevention and treatment programs.
Supplementary Material
Acknowledgments
Study Funding: None
Footnotes
The findings and conclusions of this article are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention (CDC).
H. Joo planned the study, performed all statistical analyses, and wrote the manuscript.
D.O. Dunet helped plan the study, and contributed to revising the manuscript.
J. Fang helped plan the study, and contributed to revising the manuscript.
G. Wang supervised the study, and contributed to revising the manuscript.
Disclosure: None
Dr. Joo reports no disclosure.
Dr. Dunet reports no disclosure.
Dr. Fang reports no disclosure.
Dr. Wang reports no disclosure.
Contributor Information
Diane O. Dunet, Email: dianedunet@gmail.com.
Jing Fang, Email: cvy8@cdc.gov.
Guijing Wang, Email: gbw9@cdc.gov.
References
- 1.Han B, Haley WE. Family caregiving for patients with stroke. Review and analysis. Stroke. 1999;30:1478–1485. doi: 10.1161/01.str.30.7.1478. [DOI] [PubMed] [Google Scholar]
- 2.Brown DL, Boden-Albala B, Langa KM, et al. Projected costs of ischemic stroke in the United States. Neurology. 2006;67:1390–1395. doi: 10.1212/01.wnl.0000237024.16438.20. [DOI] [PubMed] [Google Scholar]
- 3.Leal J, Luengo-Fernandez R, Gray A, Petersen S, Rayner M. Economic burden of cardiovascular diseases in the enlarged European Union. European Heart Journal. 2006;27:1610–1619. doi: 10.1093/eurheartj/ehi733. [DOI] [PubMed] [Google Scholar]
- 4.Hickenbottom SL, Fendrick AM, Kutcher JS, Kabeto MU, Katz SJ, Langa KM. A national study of the quantity and cost of informal caregiving for the elderly with stroke. Neurology. 2002;58:1754–1759. doi: 10.1212/wnl.58.12.1754. [DOI] [PubMed] [Google Scholar]
- 5.Dewey HM, Thrift AG, Mihalopoulos C, et al. Informal care for stroke survivors: results from the North East Melbourne Stroke Incidence Study (NEMESIS) Stroke. 2002;33:1028–1033. doi: 10.1161/01.str.0000013067.24300.b0. [DOI] [PubMed] [Google Scholar]
- 6.van den Berg B, Brouwer W, van Exel J, Koopmanschap M, van den Bos GA, Rutten F. Economic valuation of informal care: lessons from the application of the opportunity costs and proxy good methods. Social Science & Medicine. 2006;62:835–845. doi: 10.1016/j.socscimed.2005.06.046. [DOI] [PubMed] [Google Scholar]
- 7.Riewpaiboon A, Riewpaiboon W, Ponsoongnern K, Van den Berg B. Economic valuation of informal care in Asia: a case study of care for disabled stroke survivors in Thailand. Social Science & Medicine. 2009;69:648–653. doi: 10.1016/j.socscimed.2009.05.033. [DOI] [PubMed] [Google Scholar]
- 8.Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number U01AG009740) Ann Arbor, MI: 2012. Health and Retirement Study,2006 and 2008 Core (Final V2.0) public use dataset. [Google Scholar]
- 9.Produced by the RAND Center for the Study of Aging, with funding from the National Institute on Aging and the Social Security Adminstration. Santa Monica, CA: 2012. Mar, RAND HRS Data, Version L. [Google Scholar]
- 10.Hayman JA, Langa KM, Kabeto MU, et al. Estimating the cost of informal caregiving for elderly patients with cancer. Journal of Clinical Oncology : Official Journal of the American Society of Clinical Oncology. 2001;19:3219–3225. doi: 10.1200/JCO.2001.19.13.3219. [DOI] [PubMed] [Google Scholar]
- 11.Langa KM, Chernew ME, Kabeto MU, et al. National estimates of the quantity and cost of informal caregiving for the elderly with dementia. Journal of General Internal Medicine. 2001;16:770–778. doi: 10.1111/j.1525-1497.2001.10123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Langa KM, Fendrick AM, Flaherty KR, Martinez FJ, Kabeto MU, Saint S. Informal caregiving for chronic lung disease among older Americans. Chest. 2002;122:2197–2203. doi: 10.1378/chest.122.6.2197. [DOI] [PubMed] [Google Scholar]
- 13.Langa KM, Fultz NH, Saint S, Kabeto MU, Herzog AR. Informal caregiving time and costs for urinary incontinence in older individuals in the United States. Journal of the American Geriatrics Society. 2002;50:733–737. doi: 10.1046/j.1532-5415.2002.50170.x. [DOI] [PubMed] [Google Scholar]
- 14.Langa KM, Valenstein MA, Fendrick AM, Kabeto MU, Vijan S. Extent and cost of informal caregiving for older Americans with symptoms of depression. The American Journal of Psychiatry. 2004;161:857–863. doi: 10.1176/appi.ajp.161.5.857. [DOI] [PubMed] [Google Scholar]
- 15.Langa KM, Vijan S, Hayward RA, et al. Informal caregiving for diabetes and diabetic complications among elderly americans. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2002;57:S177–S186. doi: 10.1093/geronb/57.3.s177. [DOI] [PubMed] [Google Scholar]
- 16.Amirkhanyan AA, Wolf DA. Parent care and the stress process: findings from panel data. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2006;61:S248–S255. doi: 10.1093/geronb/61.5.s248. [DOI] [PubMed] [Google Scholar]
- 17.Van Houtven CH, Norton EC. Informal care and health care use of older adults. Journal of Health Economics. 2004;23:1159–1180. doi: 10.1016/j.jhealeco.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 18.Gure TR, Kabeto MU, Blaum CS, Langa KM. Degree of disability and patterns of caregiving among older Americans with congestive heart failure. Journal of General Internal Medicine. 2008;23:70–76. doi: 10.1007/s11606-007-0456-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spector WD, Fleishman JA. Combining activities of daily living with instrumental activities of daily living to measure functional disability. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 1998;53:S46–S57. doi: 10.1093/geronb/53b.1.s46. [DOI] [PubMed] [Google Scholar]
- 20.Card D, Krueger AB. Minimum-Wages and Employment - a Case-Study of the Fast-Food Industry in New-Jersey and Pennsylvania. American Economic Review. 1994;84:772–793. [Google Scholar]
- 21.Zeng F, An JJ, Scully R, Barrington C, Patel BV, Nichol MB. The impact of value-based benefit design on adherence to diabetes medications: a propensity score-weighted difference in difference evaluation. Value in Health. 2010;13:846–852. doi: 10.1111/j.1524-4733.2010.00730.x. [DOI] [PubMed] [Google Scholar]
- 22.Baser O. Too much ado about propensity score models? Comparing methods of propensity score matching. Value in Health. 2006;9:377–385. doi: 10.1111/j.1524-4733.2006.00130.x. [DOI] [PubMed] [Google Scholar]
- 23.Wang G, Zhang Z, Ayala C. Hospitalization costs associated with hypertension as a secondary diagnosis among insured patients aged 18–64 years. American Journal of Hypertension. 2010;23:275–281. doi: 10.1038/ajh.2009.241. [DOI] [PubMed] [Google Scholar]
- 24.Schonlau M, van Soest A, Kapteyn A, Couper M. Selection bias in web surveys and the use of propensity scores. Sociological Methods & Research. 2009;37:291–318. [Google Scholar]
- 25.PSMATCH2: Stata module to perform full Mahalanobis and propensity score matching, common support graphing, and covariate imbalance testing. [computer program] Version 4.0.6. 2012 May 17; 2003. [Google Scholar]
- 26.Version 3.0.1. Boston College: Department of Economics; 2013. Aug, DIFF: Stata Module to Perform Differences in Differences Estimation [computer program] 2011. [Google Scholar]
- 27.Fang J, Shaw KM, George MG. Prevalence of stroke- United States, 2006–2010. Morbidity and Mortality Weekly. 2012;61:379–383. [PubMed] [Google Scholar]
- 28.Golberstein E, Grabowski DC, Langa KM, Chernew ME. Effect of Medicare home health care payment on informal care. Inquiry. 2009;46:58–71. doi: 10.5034/inquiryjrnl_46.01.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Colombo F, Llena-Nozal A, Mercier J, Tjadens F. Chapter 4 Policies to support family carers. [Accessed June 30, 2014];Help wanted? Providing and paying for long-term care [online] Available at: http://www.oecd.org/health/longtermcare/helpwanted. [Google Scholar]
- 30.Kissela BM, Khoury JC, Alwell K, et al. Age at stroke: Temporal trends in stroke incidence in a large, biracial population. Neurology. 2012;79:1781–1787. doi: 10.1212/WNL.0b013e318270401d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peek MK, Coward RT, Peek CW. Race, aging, and care - Can differences in family and household structure account for race variations in informal care? Research on Aging. 2000;22:117–142. [Google Scholar]
- 32.McCann JJ, Hebert LE, Beckett LA, Morris MC, Scherr PA, Evans DA. Comparison of informal caregiving by black and white older adults in a community population. Journal of the American Geriatrics Society. 2000;48:1612–1617. doi: 10.1111/j.1532-5415.2000.tb03872.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.