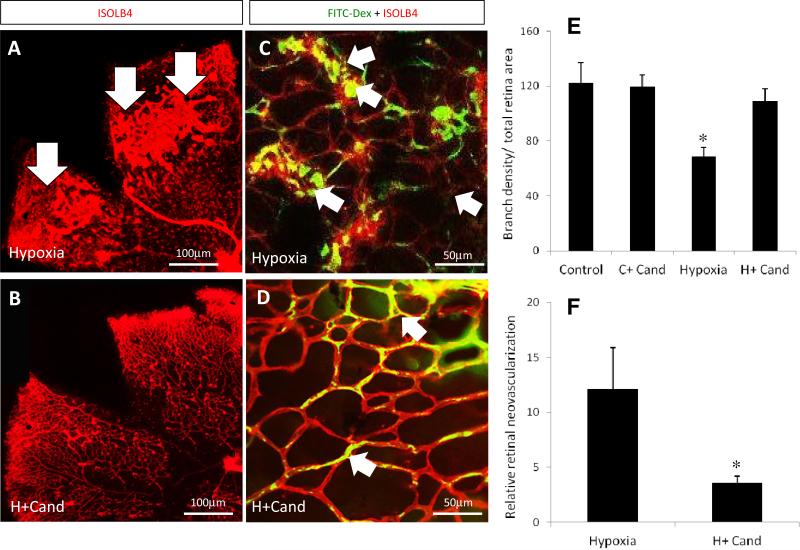
Figure-1. Candesartan prevented the hypoxia induced pathological retinal neovascularization.
(A, B) Representative images of flat-mounted retinas of animals subjected to normoxia or hypoxia and treated with candesartan on p17 and labeled with isolectin-B4 (red). (C, D) Higher magnification confocal images (63X) of retinas perfused with FITC-Dextran (green) and labeled with isolectin-B4 to examine vascular density and the neovascularization. In hypoxia, areas of tufts, a pathological bulb-like structure of new micro-blood vessels grew toward the vitreous far away from the retinal capillary plexus, are higher in the peripheral retinal-vasculature with less perfusion at the central areas (C, arrows) compared to those exposed to hypoxia treated with candesartan (10mg/kg/day, ip) (D, arrows). This indicates that candesartan had a reparative response stimulating intra-retinal angiogenesis in the ischemic retinal fields. (E) Quantification data of vascularized zones normalized to the whole retinal area and vessel density as measured by branch point number in randomized selected field. As the bar chart indicates, the vascular density significantly dropped in hypoxia but not in hypoxia after treatment with candesartan. (F) Quantification data of tufts (neovascular) area normalized to total the retina area. Tufts area reduced by ~70% in hypoxia-candesartan compared to hypoxia. p=postnatal, i.p= intraperitoneal, n=10-12/group, *p<0.05 vs the rest of groups.