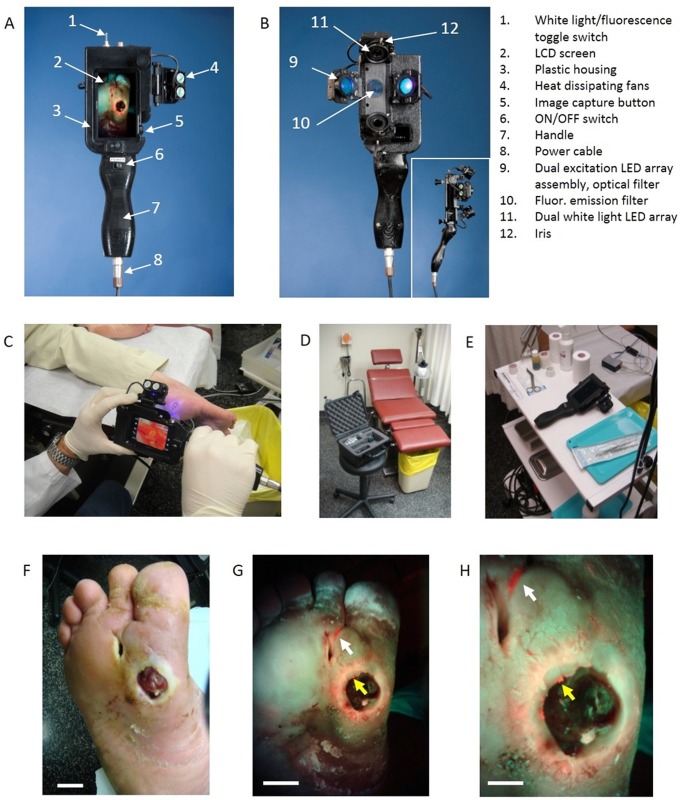
Fig 3. Photographs of the handheld prototype PRODIGI imaging device and its use for real-time autofluorescence imaging of bacterial load invisible by white light examination.
A. Front view of PRODIGI showing wound fluorescence image displayed in real-time on the LCD screen in high definition. B. Back view of PRODIGI showing white light and 405 nm LED arrays providing illumination of the wound, while the fluorescence mission filter is placed in front of the CCD sensor. Inset shows side profile of the device. C-E. Photograph of PRODIGI device used to examine a diabetic foot ulcer with room lights on, in a hard shell carrying case in a typical wound clinic setting, and placed on typical wound care cart, respectively. Room lights are turned off for fluorescence imaging. F. PRODIGI white light image of type II diabetic foot ulcer in a 52 y old male patient. G. Corresponding AF image taken in < 1 sec showing bright red fluorescence of pathogenic bacteria in the wound periphery (yellow arrow) and in ‘off site’ areas (white arrow) away from the primary wound (confirmed by swab microbiology as mainly heavy growth S. aureus). Bacterial fluorescence appears red against a background of green fluorescence from connective tissues of the healthy skin, which provides anatomical context for localizing the bacteria within and around the wound. The bacterial regions were not seen under white-light visualization. H. A magnified view of G. showing S. aureus growing within the fissures of the wound periphery. Bright fluorescent ‘hot spots’ (yellow arrow) illustrate heterogeneity in the distribution of bioburden in the wound periphery. Fluorescence imaging allowed targeted swabbing of bacterial areas not possible by white light visualization. The heavy growth S. aureus growing in the off-site area was invisible by traditional clinical examination. Scale bars: A. 2 cm, B. 2 cm, C. 1 cm.